
Liver abscess symptoms, causes, treatments
The liver abscess it is a collection of pus surrounded by a fibrous capsule within the liver. It is the result of any infectious process that leads to the secondary destruction of the parenchyma (tissue) and stroma (structure) of the liver.
Various germs are involved in its origin, being more frequent in men and between 30 and 60 years of age. It occurs most commonly in tropical countries. It can present as a single abscess or multiple abscesses, and in up to 90% of cases it involves the right lobe of the liver.

By James Heilman, MD [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], from Wikimedia Commons
In its clinical course, it has a moderate mortality (2-12%) and can seriously compromise the life of the patient, having a generally fatal outcome if it is not diagnosed and treated promptly and properly.
Its prognosis and treatment depend on the germ involved, with surgery being necessary in almost all complicated cases for its definitive resolution..
Article index
- 1 Symptoms
- 2 Causes
- 2.1 Pyogenic liver abscess
- 2.2 Amebic liver abscess
- 2.3 Fungal liver abscess
- 3 Diagnosis
- 4 Complications
- 5 Forecast
- 6 Treatment
- 7 References
Symptoms
The symptoms that a person with liver abscess presents are diverse and their severity will be related to the agent that produces the abscess, the time of evolution and the integrity of their immune system.
They will be installed in a variable period of between 2 and 4 weeks, being more severe and faster in their presentation the more young the person is. In general we will find:
- Fever (with or without chills). Depending on the severity of the causative agent. Almost nonexistent in mycoses; moderate to high in amebiasis; severe in pyogenic abscesses.
- Abdominal pain. Of progressive onset, located on the right side (rarely involving the entire abdomen), of variable intensity, of an oppressive or stabbing nature, continuous, without mitigating and exacerbated by movements.
- Rapid and involuntary weight loss.
- Night sweats.
- Yellowing of the skin (jaundice) with or without accompanying itching (itching).
- Nausea and / or vomiting.
- Clay-colored stools. Product of the decrease in the metabolism of bilirubin by the liver.
- Cloudy or colored urine, usually brown to black (looks like cola).
- General weakness.
The symptoms will be less florid in the elderly. If the abscess is located below the diaphragm, respiratory symptoms such as cough and pleuritic pain radiating to the right shoulder may coexist.
It is common to find a history of cholecystectomy (removal of the gallbladder), gallstones (gallstones), alcohol consumption and diabetes.
Causes
The cause of liver abscess is an infection at the liver level. The origin of this infection can be:
- Biliary (40%), due to stones, stenosis or neoplasms, and it occurs ascendingly, from the gallbladder to the liver.
- Portal (16%), secondary to an infectious process in another intra-abdominal organ, as evidenced in cases of appendicitis, diverticulitis, or inflammatory bowel disease that compromises portal venous circulation.
- Infection of a neighboring structure (6%), such as the gallbladder or colon, and by contiguity spreads directly to the liver.
- Bacteremias of any origin (7%).
- Hepatic trauma (5%), previously developing a hematoma that becomes secondarily infected.
- Cryptogenic (26%), infections of obscure or unknown origin.
Abscesses can be single (60-70%) or multiple (30-40%). Depending on the germs involved, we can divide liver abscesses into three large groups:
- Pyogenic (bacterial)
- Amebian
- Mycotic.
There are no conclusive statistics regarding the prevalence of one or the other, as it depends on the place where the study was carried out, the majority being of the pyogenic type in developed countries and of the amoebic type in developing countries..
Yes, a clear prevalence of pyogenic abscesses has been established in people with diabetes.
Pyogenic liver abscess
Enterobacteriaceae, especially Escherichia coli Y Klebsiella spp, are the most common etiology, although it can be found Streptococcus spp., Enterococcus spp, Peptococcus spp., Peptostreptococcus spp. Y Bacteroides spp.
Amebic liver abscess
It is more frequent in developing countries, being endemic in some countries such as Mexico, where it represents a public health problem..
The amoebaEntamoeba histolytica) reaches the liver via the portal circulation, being the most common form of extraintestinal amebiasis.
In general, the patient has a history of having visited an endemic area in a period that may span up to 5 months previously, or having suffered from amoebic dysentery within 8 to 12 weeks prior to the onset of symptoms.
Fungal liver abscess
They occur almost exclusively in immunosuppressed patients with HIV infection or who receive chemotherapy or who have received an organ transplant. The administration of corticosteroids enhances the possibility of its appearance.
Cases are reported by Mucor spp and Candida spp.
Diagnosis
In addition to the clinical findings (hypotension, tachycardia and tachypnea) and the symptoms referred by the patient, the diagnosis of liver abscess involves carrying out laboratory tests and imaging studies for its confirmation..
In the laboratory, there will be significant elevation of white blood cells, anemia, and elevated sedimentation rate and C-reactive protein (CRP)..
Likewise, liver function tests will be altered, with elevated transaminases, alkaline phosphatase (its elevation suggests pyogenic abscess in 70% of cases) and bilirubins, and decreased proteins at the expense of albumin (hypoalbuminemia).
The single standing plain abdominal X-ray may present suggestive signs: air-fluid levels in the abscess cavity. The image of the liver can be seen shifted downward, larger than usual, or by shifting the diaphragm upward..
If the abscess is subdiaphragmatic, the chest X-ray may also show alterations: atelectasis and even pleural effusion.
The diagnostic method of choice is abdominal ultrasound, which has a sensitivity of 85-95%. It has the benefit of being non-invasive, easily accessible and inexpensive, while it can be therapeutic (the abscess can be drained by directing the fine needle puncture).
Computerized axial tomography (CT) has a sensitivity of 95-100%, with the inconvenience of its high cost and not being available in all sites, but it is the definitive confirmatory study.
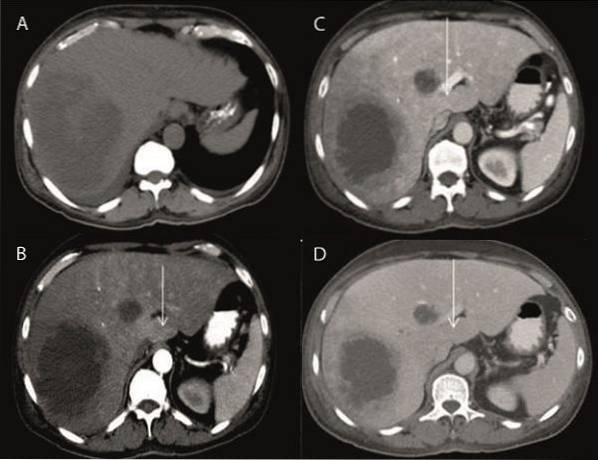
A- CT without contrast in the axial plane shows a hypodense, well-defined multilocular abscess in the right liver lobe (segment VII and VIII) and in the medial segment of the left lobe (IV b).
B- CT with contrast in the arterial phase shows a regional attenuation difference in the left lobe adjacent to the abscess of the left liver lobe (white arrow) with a subtle increase in density (transient liver attenuation differences, THAD).
C- Portal phase: shows that the previously noted THAD in the left lobe adjacent to the abscess has become isodense with the rest of the liver (white arrow).
D- Late phase: once again the THAD remains isodense with the rest of the liver (white arrow).
By Dr. Sanjay M. Khaladkar, Dr. Vidhi Bakshi, Dr. Rajul Bhargava and Dr. VM Kulkarni [CC BY 4.0 (https://creativecommons.org/licenses/by/4.0)], via Wikimedia Commons and modified by the author (@DrFcoZapata)
Complications
The complications of liver abscess derive mainly from its origin.
10-20% of cases can be complicated by rupture of the abscess with subsequent leakage of the contents into the abdominal cavity, which will lead to peritonitis, septicemia and sepsis..
The other possibility is that the rupture occurs due to contiguity and extension to neighboring structures, the most frequent being the pleural cavity (subdiaphragmatic abscesses) which leads to empyema, pericardial cavity (those located in the left lobe) or more rarely to colon.
Immunocompromised patients, with severe hypoalbuminemia (malnutrition) and with diabetes are more susceptible to complications. In the latter, the risk of complications triples.
Forecast
In general, the prognosis of cases diagnosed early and treated appropriately is good. Poor prognostic factors are:
- Multiple abscesses
- Abscess cavity volume> 500 ml
- Elevation of the right hemidiaphragm or pleural effusion
- Spontaneous or traumatic rupture of the abscess with intra-abdominal drainage
- Encephalopathy
- Total bilirubin> 3.5 mg / dL
- Hemoglobin < 8 g/dL
- Albumin < 2 g/dL
- Diabetes.
Cases that are complicated by sepsis or shock are those that generally have a fatal outcome, especially in the case of abscesses that drain into the thoracic cavity.
Treatment
Like complications, treatment will be oriented according to the cause, in addition to considering the clinical conditions (seriousness or not) of the person at the time of diagnosis..
In uncomplicated cases, the treatment of choice is the administration of the appropriate medication plus drainage of the abscess, either by echo-guided needle puncture, by placement of a drainage catheter, or surgically..
In the case of pyogenic abscesses, there are several schemes, but the combination of two broad-spectrum antibiotics is always used (if the possibility of culturing is not available). In all cases, 2 to 4 weeks of treatment.
Amebic liver abscesses should be treated with metronidazole for 7 to 10 days or subsequently with tinidazole for a minimum of 10 days..
Fungal abscesses are treated with amphotericin B or fluconazole for at least 15 days, monitoring the high toxicity of amphotericin.
Although surgery was previously the common treatment modality, in combination with drug therapy, technological advances have allowed it to be reserved for complicated cases.
Management should always include drainage of the abscess. Drainage techniques include ultrasound- or CT-guided percutaneous needle drainage, catheter placement drainage, surgical drainage, or drainage by a special technique called endoscopic retrograde cholangiopancreatography (ERCP).
In the case of abscesses greater than 5 centimeters located in the right lobe of the liver, the placement of a drainage catheter is preferred since therapeutic failure of up to 50% has been evidenced in cases drained by needle aspiration.
Surgery has its absolute indication in the case of abscesses located in the left lobe (due to the risk of complications with drainage towards the pericardium), in multiple abscesses, loculated abscesses (internally septate and divided into small cavities) or when there has been a poor response to treatment after 7 days of percutaneous drainage.
References
- Carrillo Ñ, L; Cuadra-Urteaga, JL, et al. Hepatic Abscess: Clinical and Imaging Characteristics and Management at Hospital Loayza in 5 years. Rev. Gastroenterol. Peru; 2010; 30-1: 46-51.
- Reyna-Sepúlveda, M. Hernández-Guedea, S. García-Hernández, J. Sinsel-Ayala, L. Muñoz-Espinoza, E. Pérez-Rodríguez, G. Muñoz-Maldonado. Epidemiology and prognostic factors of liver abscess complications in northeastern Mexico. University Medicine. 2017; 19 (77): 178-183.
- Osman K, Srinivasa S, Koea J. Liver abscess: contemporary presentation and management in a Western population. NZMJ 2018; 131: 65-70.
- Wang WJ, Tao Z, Wu HL. Etiology and clinical manifestations of bacterial liver abscess. A study of 102 cases. Medicine 2018; 97: 38 (e12326).
- Zhang J, Du Z, Bi J, Wu Z, et al. The impact of previous abdominal surgery on clinical characteristics and prognosis of pyogenic liver abscess. Medicine 2018; 97: 39 (e12290).
- Diagnosis and treatment of uncomplicated amebic liver abscess. 2014. IMSS 282-10 Clinical Practice Guide. www.cenetec.salud.gob.mx.
- Rivera J, Soler Y, et al. Complicated amoebic liver abscess open to the pleural cavity. An Med (Mex) 2017; 62 (4): 293-297.
- Romano AF, González CJ. Hepatic abscesses due to mucormycosis. An Med (Mex) 2008; 53 (2): 100-103.
- Abusedera MA, El-Badry AM. Percutaneous treatment of large pyogenic liver abscess. Egypt J Rad and Nucl Med 2014; 45 (1): 109-115.
- Khan A et al. Liver abscess drainage by needle aspiration versus pigtail catheter: a prospective study. Int Surg J 2018; 5 (1): 62-68.
- Lamagrande A, Sánchez S, De Diego A et al. Liver abscesses Radiological diagnosis and percutaneous treatment. DOI: 10.1594 / seram2014 / S-0982.



Yet No Comments