
Placental accreta symptoms, causes, types, treatment
The placental accreta defines a condition where the placenta is abnormally attached to the mother's uterus. The abnormal adherence of the placenta produces a delay in the expulsion of this, requiring its manual and even surgical removal. It was first described in 1937 by physician Frederick Irving.
The placenta is an important structure for embryonic and fetal development. In pregnancy, it is a uterine annex necessary for nutrition and oxygen supply to the gestation product. The anchorage of the placenta to the uterus is due to chorionic villi.
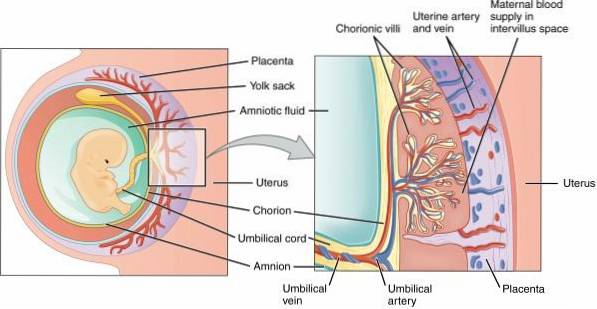
After the fertilization of the ovum by the sperm, the egg formed undergoes a series of changes due to cell division. Multiple divisions form the blastocyst, and its outermost layer, the trophoblast, will give rise to the placenta. Trophoblastic cells associate with uterine decidual cells, determining the implantation of this organ.
There are multiple problems associated with placental implantation, from an abnormal location to premature detachment. Placental accreta allows normal fetal development, but has a maternal complication postpartum. Puerperal hemorrhage is the main clinical sign and symptom.
The first cause of placental accreta is previous uterine surgery. It is estimated that the incidence of this abnormality has increased in the last thirty years, currently being 3 per thousand pregnancies. It is probably related to the increase in surgeries and cesarean sections in that period of time.
Three types of abnormal placental implantation have been described, depending on the invasion of the chorionic villi into the myometrium: accreta, increta, and percreta..
Treatment, in most cases, consists of a total hysterectomy immediately after delivery..
Article index
- 1 Symptoms
- 1.1 Limitation to deliver the placenta
- 1.2 Puerperal maternal hemorrhage
- 1.3 Pain
- 2 Causes
- 2.1 Previous caesarean sections
- 2.2 Multiple pregnancies
- 2.3 Short intergenetic period
- 2.4 Age
- 2.5 Excision of uterine fibroids
- 2.6 Uterine curettage
- 2.7 Asherman's syndrome
- 3 Types
- 3.1 - According to the depth of the villi
- 3.2 - According to the degree of implementation
- 4 Treatment
- 5 Complications
- 6 References
Symptoms
Initially, clinical signs and symptoms are rare. In fact, symptoms are often absent during pregnancy. The most frequent clinical findings are limitation to deliver the placenta and puerperal maternal hemorrhage..
Pain is not a common symptom, however, difficulty in expelling the abnormally attached placenta can cause it..
Limitation in expelling the placenta
It consists of the delay of placental expulsion -birth- that should occur within 30 minutes after delivery. The adherence of the chorionic villi to the myometrium prevents detachment of the placenta.
Puerperal maternal hemorrhage
The pregnant uterine bed has a great blood supply. In normal cases, postpartum, there is limited bleeding as part of the placental abruption. Sustained uterine contraction contributes to the closure of bleeding blood vessels.
When there is accreta, the placenta may partially detach or not detach; in both cases, significant bleeding occurs.
The degree of invasion of the villi is related to the intensity of the bleeding. Attempted manual delivery only makes bleeding worse.
Pain
Placental adherence to the uterus is painless. The prenatal diagnosis of placental accreta occurs by ultrasound observation, or when there is a clinical suspicion.
However, if delivery does not occur, moderate to severe pain may occur as a result of uterine contractions..
As with bleeding, assisted or manual delivery is painful and is also contraindicated.
Causes
The decidua is a linear structure found in the endometrium and forms during pregnancy. This structure allows the anchorage of the placenta, in addition to providing oxygen, nutrients and protection to the embryo.
The decidua also contributes to the secretion of hormones, growth factors, and important proteins, such as cytokines..
The portion of the decidual line in contact with the placenta is called the decidua basalis or placental. Specifically, this portion of the decidua maintains control over trophoblast growth and invasion. The absence or deterioration of the decidua basalis allows trophoblastic invasion - and of the chorionic villi - into the myometrium.
Any abnormal condition in the formation of the decidua basalis can cause accreta. The main cause of placental adherence is previous uterine surgeries, due to the potential scar or adhesion damage that results from these procedures..
Previous cesarean sections
Statistically, there is a correlation between the number of cesarean sections and the possibility of presenting placental accreta. Cesarean section is the surgical assistance to pregnancy, and both instrumentation and manual delivery are factors that can damage the endometrium.
Multiple pregnancies
Repeated pregnancies increase the risk of placental adherence. Each pregnancy involves uterine trauma and, consequently, possible endometrial injury, scars or adhesions.
The greater the number of pregnancies in a woman, there is also a greater risk of presenting placental retention that requires manipulation and manual extraction.
Short intergenetic period
It refers to the short time that elapses between one pregnancy and another in women. This results in a uterine structure that may not have fully recovered from the previous pregnancy..
Age
Age is an important factor that must be taken into account before the possibility of placental accreta. The uterus is subjected to the same aging process as the rest of the organs. The risk of placental adherence due to accreta increases with age.
It has been established that age over 35 years is a cause, as well as a risk factor, of placental accreta.
Excision of uterine fibroids
The removal of benign myometrial tumors involves not only manipulating the uterus but also the production of residual scars..
Uterine curettage
In cases of abortion, uterine curettage is a way of cleaning the endometrial surface. This is done in order to extract placental remains and avoid bleeding due to retention of these.
It is a procedure that can result in endometrial or myometrial injuries, in addition to scars.
Asherman's syndrome
It is a syndrome caused by the existence of endometrial scar tissue that produces alteration or absence of menstruation. It is called intrauterine synechiae (adhesions), promoted by uterine curettage or endometriosis.
Asherman's syndrome makes the existence of pregnancies difficult, however, when these occur, the condition becomes an important risk factor for the existence of placental accreta.
Types
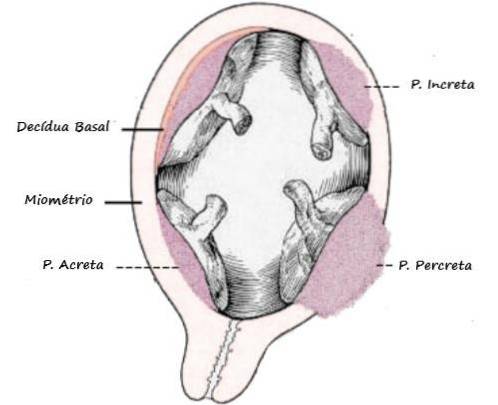
Abnormal uterine implantation can be classified according to the depth of penetration of the chorionic villi into the myometrium. In addition, the surface of adherence of the placenta with respect to the uterus provides another classification.
- According to the depth of the villi
There are three degrees of accreta with respect to myometrial invasion: placenta accreta, increta, and percreta..
Placenta accreta
It is the most common of the 3, characterized by the adhesion of the placenta to the myometrium in the absence of a decidual line. Occurs in 70% to 75% of cases, and manual removal may sometimes be considered, preserving the uterus.
Placenta increta
It occurs in 15 to 20% of cases. The chorionic villi reach the uterine muscle. This type of accreta is firm and the only way of resolution is total hysterectomy..
Placenta percreta
The least common and most severe type of accretion (5% to 10%). In this variety, the villi pass through the myometrium and can reach the serosa of the organ. Invasion of neighboring organs and structures to the uterus is possible and increases severity.
- According to the degree of implantation
Placental adherence can be total or partial, depending on the placental contact surface - myometrium.
Total
The entire placenta is attached to the uterine muscle, and is a consequence of the presence of scar tissue or extensive damage.
The previous endometrial injury predisposes to the absence of a decidual line that prevents the penetration of the villi. When it occurs, hysterectomy is the only possible treatment.
Partial
Also called focal placental accreta. It consists of a portion of the placenta attached to the myometrium. When it occurs, it is possible to perform a conservative treatment thus avoiding uterine excision.
Treatment
Placenta accreta is a condition that poses a high risk of maternal-fetal morbidity and mortality. It is a fact that both prevention and conservative treatment are difficult in these cases..
Manual removal of an abnormally adherent placenta has been described as an alternative, especially in the true placenta accreta. However, total hysterectomy is the treatment of choice.
The Royal College of Obstetricians and Gynecologists (RCOG) have developed a guide for the management of placental accreta. Carrying out an early diagnosis and monitoring the patient during pregnancy is of vital importance..
For this reason, the expectant mother must be informed and correctly oriented before the possibility of a hysterectomy..
The fundamental elements that must be considered to guarantee a good result in the hysterectomy:
- Specialized medical care from the beginning of pregnancy, in addition to surveillance and guidance to the patient.
- Planning of the surgical act that includes the best alternative for both anesthesia and procedural.
- Have blood and blood products at the time of surgery.
- Multi-disciplinary approach to patient care and preparation for surgery.
- Have an intermediate or intensive care room in the center where the hysterectomy will be performed.
Other conservative techniques have been described. Ligation or embolization of the uterine artery, in addition to the use of methotrexate to dissolve the placental junction.
Currently the therapeutic approach is aimed at performing the hysterectomy immediately after the scheduled cesarean section..
Complications
Complications of placental adherence can be avoided with early diagnosis, pregnancy monitoring, and proper medical management..
When the presence of placental accreta is unknown, the diagnosis is a finding within delivery or cesarean section. The rapid action of the medical staff will define the prognosis of the box.
Complications that can arise from placental accreta are:
- Massive hemorrhage, with risk of hypovolemia or hypovolemic shock.
- Premature births, including all possible complications from fetal immaturity.
- Infertility, secondary to hysterectomy.
- Disseminated intravascular coagulation.
- Venous thromboembolism.
- Urological lesions, both in the ureter and the bladder.
- Fistula formation between the vagina and the urinary bladder.
- Uterine rupture - due to placenta accreta - is very rare, but has been described.
- Maternal death.
References
- Irving, F; Hertig, A (1939). A study of placenta accreta. Recovered from ajog.org
- (s.f.). Placental development. Recovered from teachmephisiology.com
- Wikipedia (last rev 2018). Deciduous. Recovered from en.wikipedia .org
- Moldenhauer, JS (s.f.). Placental accreta (placenta accreta). Recovered from msdmanuals.com
- Silver, RM; Branch, W (2018). Placenta accreta spectrum. New england journal of medicine. Recovered from intramed.net
- Bartels, HC; Postle, JD; Downey, P; Brennan, DJ (2018). Placenta accreta spectrum: a review of pathology, molecular biology, and biomarkers. Disease markers. Recovered from hindawi.com
- Kilcoyne, A; Shenoy-Bhangle, AS; Roberts, DJ; Clark S, R; Gervais, DA Lee, SI (2017). MRI of placenta accreta, placenta increta, and placenta percreta: pearls and pitfalls. Recovered from ajronline.org
- American Pregnancy staff (Last rev 2017). Placenta accreta. Recovered from americanpregnancy.org
- (s.f.). Asherman's syndrome. Recovered from my.clevelandclinic.org
- Resnik, R; Silver, RM (Last rev 2018). Clinical features and diagnosis of placenta accreta spectrum (placenta accreta, increta, and percreta). Recovered from uptodate.com
- Resnik, R; Silver, RM (Last rev 2018). Management of the placenta accreta spectrum (placenta accreta, increta, and percreta). Recovered from uptodate.com
- Resnik, R (2011). Placenta accreta - a dreaded and increasing complication. Recovered from medscape.com
- Moriya, M; Kusaka, H; Shimizu, K; Toyoda, N (1998). Spontaneous rupture of the uterus caused by placenta percreta at 28 weeks of gestation: a case report. In The journal of obstetrics and gynaecology research. Recovered from ncbi.nlm.nih.gov
- Broyd, N (2018). Latest rcog guidance on placenta praevia and accreta. Recovered from medscape.com
- Jauniaux, ERM; Alfirevic, Z; Bhide, AG; Belfort, MA; Burton, GJ; Collins, SL; Dornan, S; Jurkovic, D; Kayem, G; Kingdom, J; Silver, R; Sentilhes, L (2018). Placenta praevia and placenta accreta: diagnosis and management. Green-top Guideline No. 27ª. Recovered from obgyn.onlinelibrary.wiley.com.



Yet No Comments