
Aminoglycosides classification, effects, indications, contraindications

The aminoglycosides They are a set of antibiotics that share the same chemical and pharmacological characteristics. They have a bactericidal effect against aerobic Gram negative bacteria (bacteria that stain pale pink and not dark blue or violet with Gram stain).
The first aminoglycoside discovered was streptomycin, in 1943. Later, tobramycin and gentamicin appeared as effective anti-Gram negative antibiotics. In the 1970s (1970), semisynthetic aminoglycosides such as amikacin, netilmycin and dibekacin were developed..
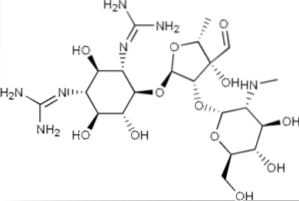
Most of the members of this family have in their structure an amino-cyclitol (a cyclic alcohol with an amino group R-NH2) linked by a glycosidic bond to one or more amino sugars, so they are actually aminoglycosides- aminocyclitols.
These antibiotics are not absorbed orally, so they are administered parenterally (intravenous, intramuscular, or subcutaneous) or used topically. They are eliminated by glomerular filtration without being previously metabolized.
All members of this family show some degree of nephrotoxicity (kidney toxins) and / or ototoxicity (toxic to both the ear and the vestibular system, can cause hearing and balance disorders).
They are generally used in combination with some beta-lactam (another family of antibiotics) and their use is usually restricted to severe infections.
These antibiotics are contraindicated in patients who have developed allergic reactions to these drugs. Although they pass into breast milk, as they are not absorbed by the intestinal (oral) route, they are considered suitable to be administered to the mother, if necessary, during lactation..
Its use during pregnancy is allowed only in cases where the clinical benefits outweigh the risks (risk category D).
Article index
- 1 Mechanism of action
- 2 Classification
- 2.1 Aminoglycoside with aminocyclitol
- 2.2 Aminocyclitol without aminoglycoside: Spectinomycin
- 3 Adverse effects
- 3.1 - Ototoxicity
- 3.2 - Nephrotoxicity
- 3.3 - Neurotoxicity and other toxic effects
- 4 Resistance to aminoglycosides
- 5 Indications
- 6 Contraindications
- 7 References
Mechanism of action
All aminoglycosides inhibit protein synthesis in susceptible bacteria. These adhere to the 30S unit of bacterial ribosomes and inhibit its function. Unlike most antimicrobial agents that inhibit protein synthesis that are bacteriostatic, these are bactericidal.
"Bacteriostatic" derives from the prefix "bacter" which means bacteria and "stasis" the Greek ending which means static, without change. In medicine, bacteriostatic agents are used to reduce the metabolism of bacteria and slow their growth and reproduction..
If the bacteriostatic agent is eliminated by dissolution, the previously inhibited bacteria will continue to develop. A bactericidal agent is one that is capable of killing bacteria. Aminoglycosides are bactericidal.
The bactericidal effect of aminoglycosides is concentration dependent. Aminoglycosides penetrate into the periplasmic space of aerobic Gram negative bacteria through water channels called aquaporins..
Transport across the cytoplasmic membrane depends on electron transport and can be inhibited or blocked by anaerobiosis (absence of oxygen), calcium, magnesium, acidic pH, or hyperosmolarity..
Once inside the cell, aminoglycosides bind to polysomes (multiple ribosomes translating the same mRNA) at the 30S subunit. They interfere with protein synthesis generating a reading failure and an early termination of the mRNA translation process.
This generates defective proteins that, when inserted into the cell membrane, alter its permeability, which will later facilitate the subsequent entry of these antibiotics. Later, ion leaks are observed, followed by larger molecules until, prior to the death of the bacteria, the proteins are lost..
Classification
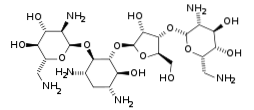
Aminoglycosides are classified into two large groups depending on whether they have an aminocyclitol with or without aminoglycoside component: aminoglycosides with aminocyclitol and aminocyclitol without aminoglycoside.
In the first group, which are those that contain aminocyclitol with aminoglycoside component, there are two subgroups. These subgroups are formed by the different components of aminocyclitol: streptidine and deoxystreptamine.
Thus, there is a subgroup with aminocyclitol streptidine and another with aminocyclitol deoxystreptamine. The most important aminoglycosides in each group are shown below.
Aminoglycoside with aminocyclitol
Aminocyclitol Streptidine: Streptomycin
Aminocyclitol deoxystreptamine: within this group are the Kanamycin, Gentamicin and other families.
Kanamycin family:
- Kanamycin
- Amikacin
- Tobramycin
- Dibekacin
Gentamicin family:
- Gentamicin
- Sisomycin
- Netilmycin
- Isepamycin
Others:
- Neomycin
- Paromomycin
Aminocyclitol without aminoglycoside: Spectinomycin
Adverse effects
All aminoglycosides are potentially toxic to the renal system, the auditory system, and the vestibular system. These toxic effects can be reversible or irreversible. These adverse secondary consequences make the administration and use of these antibiotics difficult..
When it is necessary to supply an aminoglycoside for long periods and at high doses, it is necessary to monitor auditory, vestibular and renal function, since in the initial stages these damages are reversible.
- Ototoxicity
When aminoglycosides are administered, dysfunction of both the auditory system and the vestibular system can occur. These drugs accumulate and concentrate in the perilymph and endolymph of the inner ear, especially when high doses are used..
Diffusion from these ear fluids back into the plasma is very slow, and the half-life of aminoglycosides in the ear is 5 to 6 times greater than in blood plasma. Ototoxicity is more common in those patients who have persistently high plasma concentrations.
With low doses, damage to the sensory cells of the vestibular organ and the cochlea is observed, affecting the ends (stereocilia) of the hair cells. With higher doses, basal damage is observed in these cells, until the destruction of sensory cells is generated..
When the sensory cells are destroyed the effect is irreversible and consequently permanent hearing losses occur. As cochlear sensory cells are lost with age, elderly patients are more susceptible to ototoxicity with the use of these antibiotics..
Drugs like furosemide or the acid ethacrinic they enhance the ototoxic effect of aminoglycosides. Both drugs are loop diuretics (increase urine output) used to treat high blood pressure and edema..
Although all aminoglycosides can affect both cochlear and vestibular function, there is an evident preferential toxicity.
Thus, streptomycin and gentamicin preferentially affect the vestibular system, whereas amikacin, kanamycin and neomycin primarily affect auditory function and tobramycin affects both functions equally..
Symptoms of cochlear ototoxicity
As the first symptom of ototoxicity, high-frequency tinnitus (hissing or buzzing not associated with any sound coming from outside) usually occurs. If the treatment is not suspended, in a few days the damage will be permanent.
Tinnitus can last for up to two weeks, and since the perception of high-frequency sounds is lost first, the patient is initially unaware of their hearing loss. If treatment is continued under these conditions, the hearing loss progresses to develop speech problems.
Vestibular ototoxicity symptoms
Initially, a headache of moderate intensity appears. Then vomiting, nausea, and postural balance problems appear that can persist for one to two weeks. The most prominent symptoms are vertigo in an upright position, with difficulty sitting or standing without visual cues.
The acute symptoms subside abruptly and are replaced by manifestations of chronic labyrinthitis for a period of approximately two months. Progressively compensation occurs and then only symptoms appear when closing the eyes. Recovery from this phase requires 12 to 18 months.
Most of these patients are left with some degree of permanent residual damage. As there is no specific treatment for vestibular damage, suspending the aminoglycoside at the first clinical manifestations is the only efficient measure to avoid permanent injuries.
- Nephrotoxicity
Approximately 8 to 25% of patients who receive treatment with an aminoglycoside for several days develop some reversible renal impairment. This toxicity is the result of the accumulation, concentration and retention of aminoglycosides in the cells of the renal proximal tubule..
Consequently, the structure and function of the proximal tubule is altered. Moderate proteinuria and hyaline casts initially appear in the urine. After several days, a reduction in glomerular filtration volume appears with a slight increase in plasma creatinine values..
Renal alterations are often reversible, since the proximal tubule has the capacity for regeneration. Renal toxicity depends on the total amount delivered and depends on the aminoglycoside used..
Neomycin is one of the aminoglycosides that exhibits greater renal toxicity, since it is concentrated in the renal cortex in much greater quantities than the other aminoglycosides.
- Neurotoxicity and other toxic effects
Other less frequent toxic effects have been described, among them is the neuromuscular blockade that can cause respiratory problems and / or paralysis in some muscles. Alterations in optic nerve function with the appearance of scotomas, which are transient areas of blindness, and peripheral neuritis.
Resistance to aminoglycosides
The resistance of microorganisms to aminoglycosides may be due to any of the following causes: 1) The membranes of the bacteria are impermeable to these antibiotics 2) the ribosomes of these bacteria have a low affinity for the antibiotic 3) the bacteria synthesize enzymes that inactivate the aminoglycoside.
The first two causes explain natural resistance to aminoglycosides. In contrast, enzymatic inactivation explains the acquired resistance that has been clinically described with the use of aminoglycosides..
The genes for the synthesis of these enzymes are transmitted through plasmids. Plasmids are circular structures of extrachromosomal DNA. These plasmids are widely distributed in nature, but especially in bacteria around hospital environments..
Plasmids code for many enzymes and these inactivate aminoglycosides. Since the enzymes that inactivate each aminoglycoside are different, resistance for one does not necessarily lead to resistance for another..
However, while this is true for streptomycin and gentamicin, in the case of resistance to gentamicin (as the enzyme that causes it is bifunctional), resistance to tobramycin, amikacin, kanamycin and netilmicin will occur concomitantly..
Indications
Although less toxic antibiotics have been developed, the use of aminoglycosides remains an important tool to combat severe infections caused by enterococci or streptococci..
Gentamicin, amikacin, tobramycin, and netilmicin have a broad spectrum against aerobic Gram negative bacteria. Kanamycin and streptomycin have a narrower spectrum and should not be used for Pseudomonas aeruginosa or Serratia spp.
Gentamicin is used together with penicillin or vancomycin for streptococci and enterococci. Tobramycin is used to Pseudomonas aeruginosa and some species of Proteus. For nosocomial infections (hospital infections) amikacin and netilmicin are used.
Although the foregoing represents the most frequent indications for aminoglycosides, the rational use of these antibiotics should be based on the culture and antibiogram of the offending agent..
Contraindications
Aminoglycosides are contraindicated in patients with allergic reactions to these antibiotics. They should not be used in cases of diseases caused by germs that are resistant. They should not be used during pregnancy if there are less toxic alternatives..
There are relative contraindications in patients with kidney disease and / or hearing problems.
References
- Boussekey, N., & Alfandari, S. (2007). Aminoglycosides. EMC-Treaty of Medicine, eleven(1), 1-4.
- During-Mangoni, E., Grammatikos, A., Utili, R., & Falagas, M. E. (2009). Do we still need the aminoglycosides? International journal of antimicrobial agents, 33(3), 201-205.
- Goodman and Gilman, A. (2001). The pharmacological basis of therapeutics. Tenth edition. McGraw-Hill
- Kotra, L. P., Haddad, J., & Mobashery, S. (2000). Aminoglycosides: perspectives on mechanisms of action and resistance and strategies to counter resistance. Antimicrobial agents and chemotherapy, 44(12), 3249-3256.
- Meyers, F. H., Jawetz, E., Goldfien, A., & Schaubert, L. V. (1978). Review of medical pharmacology. Lange Medical Publications.
- Palomino, J., and Pachon, J. (2003) Aminoglycosides, Infectious diseases and clinical microbiology 21 (2), 105-115.
- Rodríguez-Julbe, M. C., Ramírez-Ronda, C. H., Arroyo, E., Maldonado, G., Saavedra, S., Meléndez, B.,… & Figueroa, J. (2004). Antibiotics in older adults. Puerto Rico health sciences journal, 2. 3(1).


Yet No Comments