
Angiomatosis symptoms, causes, treatments, prevention

The bacillary angiomatosis It is an infection that causes the enlargement of small blood vessels in the skin and visceral organs. Almost all cases of bacillary angiomatosis are seen in immunocompromised patients, with the majority of cases reported in AIDS patients. Immunocompetent people can also develop the disease, but it is rare..
In people with HIV / AIDS, the disease can cause severe inflammation of the brain, bone marrow, lymph nodes, lungs, spleen and liver, which can be fatal in people with HIV..
The disease is caused by a bacteria called Rochalimaea henselae, which was reclassified as Bartonella henselae. It was named for Diane Hensel, a microbiologist.
Bacillary angiomatosis has also been called cat scratch disease, cat scratch fever, regional lymphadenitis, and benign lymphoreticulosis..
Article index
- 1 Causes of bacillary angiomatosis
- 1.1 Bartonella henselae
- 1.2 Bartonella quintana
- 2 Symptoms
- 2.1 Skin lesions
- 2.2 Areas most affected
- 2.3 Pain
- 2.4 Systemic participation
- 2.5 Mass in the abdomen
- 2.6 If the colon is affected
- 2.7 If the central nervous system is affected
- 2.8 If the larynx is obstructed
- 3 Diagnosis
- 3.1 Steps for diagnosis
- 4 Differential diagnosis
- 4.1 Kaposi's sarcoma
- 4.2 Pyogenic granulomas
- 4.3 Peruvian wart
- 5 Treatments
- 5.1 Studies on medical treatments
- 6 Forecast
- 7 Prevention
- 8 References
Causes of bacillary angiomatosis
Bacillary angiomatosis is caused by bacteria Bartonella quintana or Bartonella henselae. Bacterial infection can occur with the following organisms:
Bartonella henselae
- Transmission method - cat scratch / bite
- Transmission vector - ticks / fleas
Bartonella quintana
- Transmission method - from one human being to another
- Transmission vector - lice.
Symptoms
Skin lesions
- Its color varies from person to person (flesh color, purple, or no color)
- A single lesion or multiple lesions (papules) may appear on the skin
- Lesions resemble hemangiomas
- Variable nodule size (1 mm to 10 cm)
- Squamous nodules may also be present on the skin
- They can also be found in large masses
The extremities can be affected by extensive plaques
- Excessive pigmentation
- Excessive keratinization
Areas most affected
- Language
- Oropharynx
- Oral mucosa
- Nose
Pain
The areas most affected by pain include the forearms and legs (bone pain).
Systemic participation
- Sweating at night
- Fever / chills
- General consumption
- Weightloss
- Anorexy
- Abdominal pain
- Often accompanied by nausea and vomiting
Mass in the abdomen
This mass is accompanied by bleeding within the gastrointestinal tract..
If the colon is affected
- Bloody diarrhea
- Abdominal cramps
If the central nervous system is affected
- Headache
- Back pain
- Depression
- Anxiety
- Psychosis
- Changes in personality
- Excessive irritability
- Neuralgia (most commonly affected - trigeminal nerve)
- Seizures
If the larynx is obstructed
The patient may have difficulty breathing
The most common cardiac manifestation is endocarditis. Lung involvement is rare and can take the form of pneumonia or pleural effusion..
Neurologic complications of bacillary angiomatosis infection are rare, and the most common presentation is encephalopathy. Ocular manifestations are not rare, being neuroretinitis the most frequent.
Diagnosis
Steps for diagnosis
1-A complete physical examination is generally performed with an evaluation of the medical history.
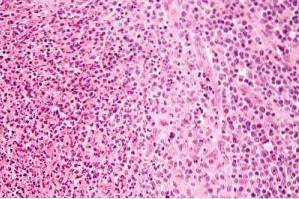
2-The tissue is biopsied and sent to a laboratory for a pathological examination.
3-The pathologist examines the biopsy under a microscope. After gathering the clinical findings and special studies on the tissues, the pathologist arrives at a definitive diagnosis. For this, it uses special techniques, such as immunohistochemical staining, which help reveal the presence of bacteria..
4-Additional tests may be necessary to rule out other clinical conditions in order to reach a definitive diagnosis, as many conditions may have similar signs and symptoms.
Differential diagnosis
The differential diagnosis of bacillary angiomatosis includes Kaposi's sarcoma, pyogenic granuloma, Peruvian wart, and various angiomas, particularly epithelioid hemangioma..
Kaposi's sarcoma
The differentiation of Kaposi's sarcoma is of greater importance, since both conditions usually occur in HIV-infected patients and in other states of community immune competence..
Although bacillary angiomatosis is potentially treatable, if it is overlooked, the result can be fatal. Rarely, Kaposi's sarcoma and bacillary angiomatosis can coexist in the same patient.
The patches, macules, and superficial plaques that are characteristic of Kaposi's sarcoma are generally not seen in bacillary angiomatosis. If plaques appear in bacillary angiomatosis, the lesions are poorly defined and often resemble cellulitis.
Histopathologic features also often allow differentiation between bacillary angiomatosis and Kaposi's sarcoma. Detection of granular groups of bacteria is a distinctive marker of bacillary angiomatosis.
Both conditions are angio-proliferative, but the vascular spaces in bacillary angiomatosis are round while those in Kaposi's sarcoma are slit-shaped..
On the other hand, endothelial cells in bacillary angiomatosis are polygonal, but in Kaposi's sarcoma they are spindle-shaped. The hyaline blood cells frequently seen in Kaposi's sarcoma are absent in bacillary angiomatosis..
Pyogenic granulomas
Pyogenic granulomas can be clinically indistinguishable from bacillary angiomatosis. Pyogenic granuloma-like lesions are one of the main clinical presentations of bacillary angiomatosis and can also resemble these histopathologically.
Pyogenic granuloma is usually solitary, although grouped lesions have been reported, as well as widely disseminated lesions.
In bacillary angiomatosis, the lesions are frequently multiple and have variable morphology, although single lesions may occur..
Histopathology differs. Neutrophils in pyogenic granuloma are present only in eroded or ulcerated lesions. The clinical and histopathological similarities between bacillary angiomatosis and pyogenic granuloma have motivated investigations as to a possible similarity in the cause, but neither has been positive.
Peruvian wart
The Peruvian wart is endemic in some parts of Peru and neighboring Andean countries, and the diagnosis should be considered only if the patient visited endemic areas.
This is caused by Bartonella bacilliformis; it may resemble bacillary angiomatosis, as the lesions are papules or nodules, some pedunculated, often hemangiomatous or hemorrhagic. The lesions in the Peruvian wart are generally multiple and involve the face, limbs and mucous membranes..
The Peruvian wart biopsy, although showing the characteristics of angioproliferation, lacks a dense neutrophilic infiltrate. The Bartonella bacilliformis can be seen in the cytoplasm of endothelial cells.
Vascular tumors, particularly epithelioid hemangioma (angiolymphoid hyperplasia with eosinophilia) can cause diagnostic difficulties in clinical diagnosis.
Solitary or multiple dermal or subcutaneous nodules are located mainly on the scalp and face. Peripheral blood eosinophilia is usually present in epithelial hemangioma.
On biopsy, there is proliferation of small to medium-sized blood vessels, often showing a lobular architecture. Vascular channels are lined by enlarged endothelial cells (epithelioids). A perivascular infiltrate is composed primarily of lymphocytes and eosinophils, not neutrophils..
Treatments
Bacterial infection can be treated with antibiotics. Administration of these medications can normally cause tumors to shrink in size and disappear, resulting in a full recovery..
This can usually take more than a month. However, drug therapy must continue for several months. If the underlying immunodeficiency cannot be cured, relapses are likely. In these cases, antibiotic therapy will be resumed or prescribed for life.
Since tumors respond well to antibiotic therapy in most cases, surgery to remove them is not usually necessary. Follow-up care with regular exams and checkups is important.
Studies on medical treatments
Despite its bacteriostatic properties, according to studies, erythromycin has shown a dramatic effect on bacillary angiomatosis, since it significantly inhibits the proliferation of dermal microvascular cells induced by both strains (Bartonella quintana and Bartonella henselae).
Doxycycline and gentamicin do not appear to be able to exert this effect. These data indicate that erythromycin, regardless of its unique bacteriostatic effects, markedly inhibited endothelial cell proliferation, which may be a clue to its efficacy against bacillary angiomatosis..
Doctors usually administer erythromycin in a dose of 2.0 g orally (most often 500 mg 4 times a day). It is used intravenously in cases of gastrointestinal intolerance or when greater absorption is expected.
Some doctors recommend clarithromycin (250 mg twice a day by mouth) or azithromycin (1.0 g a single daily dose). Clarithromycin has fewer gastrointestinal side effects. Clarithromycin and azithromycin drug concentrations in the skin after oral administration are higher than erythromycin.
Doxycycline has also been found effective and can be administered orally or intravenously. The doctor may prescribe 100 mg of Doxycycline twice a day.
Combination therapy with the addition of rifampin to erythromycin or doxycycline is recommended for immunocompromised patients with serious life-threatening illnesses..
Treatment failures have been observed when fluoroquinolones, trimethoprim-sulfamethoxazole, and narrow-spectrum cephalosporins were used..
Similar antibacterial regimens are used for extracutaneous involvement of bacillary angiomatosis. Treatment depends on the affected organ.
Forecast
The prognosis for bacillary angiomatosis is very good, as patients generally respond very well to antibiotic treatment and lesions in all affected organ systems are restored after cure..
Only slightly hardened hyperpigmented spots can remain on the skin. Delayed or absent therapy makes angiomatosis a life-threatening condition.
In order to avoid relapses, the immunocompromised condition must be treated. If that is not possible, recurrence of bacillary angiomatosis tends to occur.
Prevention
Current medical research has not established a way to prevent bacillary angiomatosis. However, any measure to prevent HIV infection also helps prevent bacillary angiomatosis..
Cats, cat fleas, and lice can all transmit bacillary angiomatosis. Therefore, contact with unfamiliar cats should be avoided and known cats should be regularly dewormed..
Proper personal hygiene is recommended, as well as keeping clothing for personal use and bedding clean. If a lice infestation is detected at home, school, or work, it should be treated immediately.
References
- Neal (2014). Bacillary Angiomatosis. University / Kirksville College of Osteopathic Medicine. Recovered from: atsu.edu.
- Mddk Staff (2016). Bacillary Angiomatosis. Mddk Online Medical Doctor. Recovered from: mddk.com.
- Christopher D.M. Fletcher (2015). Bacillary Angiomatosis. DoveMed Editorial Board. Recovered from: dovemed.com.
- Symptoma Team (2013). Bacillary Angiomatosis. Symptoma. Recovered from: symptoma.com.
- Witold Kamil Jacyk (2016). Bacillary Angiomatosis. Frontline Medical Communications. Recovered from: mdedge.com.



Yet No Comments