
What are antiphymics for, mechanism of action, side effects?

The antifimic are anti-tuberculosis drugs, that is, a set of drugs (antibiotics) that are used to treat tuberculosis. Tuberculosis is believed to be one of the oldest infectious diseases, and there are indications that it may have affected humanity since the Neolithic period..
Findings of human tuberculosis include those found in Egyptian mummies, dating from between 3500 and 2650 BC, and human remains found in Sweden and Italy dating back to the Neolithic period..
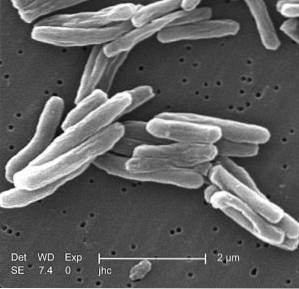
Tuberculosis, also called “consumption”, “wasting” or “white plague”, is an infectious disease caused by microorganisms called mycobacteria, belonging to the Mycobacteriaceae family and the Actinomycetales order..
The pathogenic species of mycobacteria belong to the complex Mycobacterium tuberculosis. This complex M. tuberculosis includes the M. tuberculosis or Koch's bacillus (in honor of the one who discovered it), at M. bovis, to the M. africanum, to the M. canetti, to the M. pinnipedii and to M. microti.
Tuberculosis is a contagious disease that mainly affects the lungs, but in a third of cases other organs are involved, such as the gastrointestinal system, the skeleton, the genitourinary system, the lymphatic system and the central nervous system..
According to the World Health Organization (WHO), more than two million new cases of tuberculosis appear worldwide each year; Therefore, the use of antifungal drugs and the development of new drugs is essential to combat this disease, especially in the face of the appearance of resistant and highly virulent strains.
Article index
- 1 What are antiphymics for?
- 1.1 Classification of drug groups for tuberculosis
- 2 Mechanism of action
- 2.1 rifampicin
- 2.2 Isoniacin
- 2.3 Pyrazinamide
- 3 Side effects
- 4 References
What are antiphymics for?
Antifimic drugs are used to treat tuberculosis. These are classified into first and second line medications. This classification is due to the moment in which they are used during treatment, the effectiveness they have to combat the disease and the collateral or toxic effects of the same.
The first line are those used as the first choice and the second line are used in combination with the first or when resistant strains appear..
As strains resistant to different drugs appear, experts in the field modify the groups.
First-line antiphymics initially included only isoniazine, rifampin, and pyrazinamide. Then streptomycin and ethambutol were added, and currently, due to efficacy against resistant strains, ciprofloxacin, levofloxacin, and rifabutin have been added..
Second-line drugs are much less effective and have higher toxicity than first-line drugs. The oldest of this line is para-aminosalicylic acid (PAS) and ethionamide, cycloserine, amikacin, capreomycin and floxacin are also included.
Classification of drug groups for tuberculosis
For drug-resistant tuberculosis, the WHO has modified the original list to include the following group of drugs:
1- Isoniacin, Ethambutol, Pyrazinamide, Rifampicin.
2- Second-line injectables: amikacin, kanamycin, capreomycin.
3- Fluoroquinolones: levofloxacin, moxifloxacin.
4- Second-line orals: prothionamide, cycloserine, PAS.
5- Unclear efficacy: thioacetone, clofazimine, amoxicillin / clavulanate, clarithromycin, linezolid, carbapenems C.
They have currently been reclassified as:
- GROUP A: levofloxacin, moxifloxacin and gatifloxacin
- GROUP B: amikacin, capreomycin, kanamycin (streptomycin); in children who are not serious, the use of these agents can be avoided
- GROUP C: ethionamide (or prothionamide), cycloserine (Terizidone), linezolid, clofazimine
- GROUP D (to add; they are not part of the core group of drugs)
- GROUP D1: pyrazinamide, ethambutol, high-dose isoniazine
- GROUP D2: bedaquiline and delamanid
- GROUP D3: PAS, imipenem-cilastatin, meropenem, amoxicillin-clavulanate
Mechanism of action
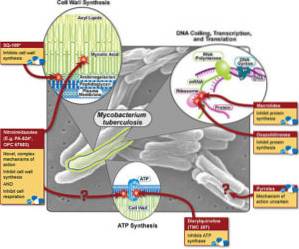
As the list of antiphymics is quite long, only the mechanisms of action of the three main first-line drugs which are rifampicin, isoniazine and pyrazinamide will be included as examples..
Rifampicin
Rifampin is considered the most important and potent antifungal drug. It is a semi-synthetic derivative of Streptomyces mediterranei, and it is fat soluble (fat soluble). It has a bactericidal activity (kills the mycobacterium) intra- and extracellularly.
This drug blocks RNA synthesis, specifically blocking and inhibiting the DNA-dependent enzyme RNA polymerase, also blocking protein synthesis in mycobacterium..
Isoniacin
Isoniazine can be included in all treatment regimens, unless there is resistance. It is soluble in water and easily penetrates into cells. This drug inhibits the synthesis of mycolic acid in the cell wall.
Has a bacteriostatic effect (inhibits bacterial growth) against resting bacilli and bactericidal (kills bacteria) against multiplying bacilli.
Pyrazinamide
Pyrazinamide is an important bactericidal antituberculous drug derived from nicotinic acid and used primarily for the short-term treatment or therapy of tuberculosis..
Its mechanism of action is similar to that of isoniazine, but with a narrower spectrum of action. Its spectrum of action only includes Mycobacterium tuberculosis. This drug slows down the metabolism of microorganisms found in an acid medium or in a caseous granuloma.
Side effects
The side effects described below are the adverse effects of the three drugs described in the previous section..
Although rifampicin is generally well tolerated, in patients with gastrointestinal problems, patients suffering from alcoholism, and the elderly, it may be associated with hepatitis, hemolytic anemias, thrombocytopenia, and immunosuppression..
Isoniazine has two major adverse effects: hepatotoxicity (toxic to the liver) and peripheral neuropathy (affects peripheral nerves). Some less common side effects also include anemia, acne, joint pain, and seizures, among others..
In the case of liver toxicity, it occurs more frequently in the elderly, when patients consume alcohol daily, when used in combination with rifampicin, in patients with HIV and in pregnant women or in the postpartum period. For these reasons, patients undergoing treatment with isoniazine should routinely undergo liver function checks..
Peripheral neuropathy is due to an interference with the metabolism of vitamin B12 and is more common when given to patients with other diseases that also cause peripheral neuropathies, such as diabetes mellitus, for example.
The adverse effects of this drug are hepatotoxicity, when high doses are used and hyperuricemia (increased uric acid in the blood), and joint pain not related to hyperuricemia..
This antifimic is, according to the WHO, the drug of choice for pregnant women who are diagnosed with tuberculosis. However, in the United States (USA) its use is not recommended due to insufficient data on the teratogenic effects of the drug..
References
- Goodman and Gilman, A. (2001). The pharmacological basis of therapeutics. Tenth edition. McGraw-Hill
- Hauser, S., Longo, D. L., Jameson, J. L., Kasper, D. L., & Loscalzo, J. (Eds.). (2012). Harrison's principles of internal medicine. McGraw-Hill Companies, Incorporated.
- Janin, Y. L. (2007). Antituberculosis drugs: ten years of research. Bioorganic & medicinal chemistry, fifteen(7), 2479-2513.
- Meyers, F. H., Jawetz, E., Goldfien, A., & Schaubert, L. V. (1978). Review of medical pharmacology. Lange Medical Publications.
- Tiberi, S., Scardigli, A., Centis, R., D'Ambrosio, L., Munoz-Torrico, M., Salazar-Lezama, M. A.,… & Luna, J. A. C. (2017). Classifying new anti-tuberculosis drugs: rationale and future perspectives. International Journal of Infectious Diseases, 56, 181-184.
- World Health Organization. (2008). Policy guidance on drug-susceptibility testing (DST) of second-line antituberculosis drugs (No. WHO / HTM / TB / 2008.392). Geneva: world health organization.



Yet No Comments