
Apraxia types and their characteristics

The apraxia it is defined as the inability to perform voluntary movements in the absence of paralysis or other motor or sensory disorders. It is an inability to carry out intentional movements, even if mobility is preserved.
That is, people who suffer from this type of disorder cannot perform the movements required to carry out an action, such as fastening a button, but they can move normally if the movements are spontaneous..

Apraxia should not be confused with dyspraxia or ataxia, since these disorders involve a general lack of motor coordination in a way that affects all types of movements.
Article index
- 1 Types of apraxia
- 1.1 Ideomotor apraxia
- 1.2 Construction apraxia
- 1.3 Ideational apraxia
- 1.4 Apraxia of speech
- 1.5 Apraxia of gait
- 1.6 Kinetic apraxia of the extremities
- 1.7 Orofacial or facial-oral apraxia
- 1.8 Oculomotor apraxia
- 2 References
Types of apraxia
Apraxias are classified according to the type of specific motor action that is affected or the area of the brain that is injured. The most frequent apraxias will be described: ideomotor, constructive, ideational apraxia and apraxia of speech. The less frequent ones will be included in the section "other apraxias".
Ideomotor apraxia
This type of apraxia is the most common. It is characterized by the fact that patients who suffer from it cannot copy movements or make everyday gestures such as nodding or waving..
These patients can describe the steps to follow to perform the action, but are unable to imagine doing the action or doing it themselves.
There are several levels of ideomotor apraxia according to its severity; in mild cases, patients perform actions inaccurately and clumsily, while in more severe cases, actions are vague, becoming unrecognizable.
At all levels of severity, the type of actions most affected are those that must be carried out when verbal instructions are given, so this is a type of test widely used to check if the person suffers from ideomotor apraxia..
Another type of test widely used in the diagnosis of this disorder is the serial movement copy test, developed by Kimura, who demonstrated that the deficits in these patients can be quantified if they were instructed to copy a series of movements performed with a specific area of the body.
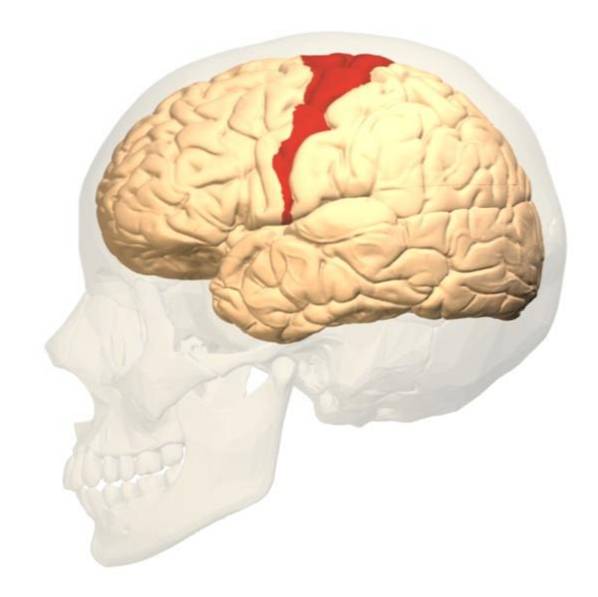
According to Heilman, the lesions in the parietal lobe would cause ideomotor apraxia, because that is the place where humans would have stored the "motor programs" to perform daily actions.
In order to perform the actions, these programs should be transmitted to the primary motor area (in the frontal lobe), which would be in charge of sending the order to perform the action to the muscles..
According to Heilman's theory, there are two types of lesions that could cause ideomotor apraxia: (1) direct lesions in the areas that contain the “motor programs” and (2) the lesion of the fibers that connect the “motor programs” with the primary motor area.
Cases with symptoms similar to those of ideomotor apraxia have also been observed after an injury to the corpus callosum, which connects both hemispheres, but it is necessary to study these cases further to know if we are really facing ideomotor apraxia and what is its effect. cause.
There is no specific method to treat apraxia since its symptoms are not reversible, but occupational therapy can help improve the patient's quality of life..
This type of therapy consists of dividing daily actions into components, such as brushing teeth and teaching the components separately, with a lot of perseverance the patient can perform the actions again, although in a somewhat clumsy way.
Construction apraxia
Construction apraxia is the second most common. Patients with this type of apraxia are unable to perform motor actions that require spatial organization, such as drawing a picture, making figures with blocks, or imitating a specific facial movement..
This type of apraxia can develop after suffering a lesion in the posterior part of the parietal lobe of any of the hemispheres, although it is not clear if the symptoms differ depending on the hemisphere where they occur..
Mountcastle proposes that lesions in the parietal lobe would cause apraxias because this area receives information from the position and movement of our own body, therefore, if it is injured it would cause a dysfunction when controlling the movement of our members.
Construction apraxias usually occur due to cerebral infarcts or as a cause of the development of Alzheimer's disease.
One of the most used tests to diagnose this type of apraxia is asking the patient to copy a drawing. With this test it is possible to differentiate even if the apraxia is caused by lesions in the left parietal lobe, in the right or by Alzheimer's disease, since the type of damage causes patients to copy the drawings with certain characteristics.
The most used therapy in cases of construction apraxia is the mental simulation of motor acts, as its name indicates, this therapy consists of making the patient imagine himself performing the motor actions step by step.
Ideational apraxia
Patients with ideational apraxia are characterized by a deficit in performing complex actions that require planning, such as sending an e-mail or preparing food. Some researchers believe that it is simply a more serious level of ideomotor apraxia but there are others who defend that it is another type of apraxia.
Like ideomotor apraxia, it is caused by lesions in the parietal lobe of the dominant hemisphere, but the exact area where this lesion occurs is not known..
This type of apraxia is difficult to diagnose since it usually occurs together with other disorders such as agnosia or aphasia. One of the most used tests to diagnose it is to present the patient with a series of objects, he must simulate that he is using each one three times using different steps for each simulation. De Renzi and Luchelli will develop a scale to check the level of deterioration of the patient according to the mistakes made.
Treatment for this type of apraxia is complicated because it is usually irreversible but occupational therapy can help, performing the same type of exercises as in the treatment of ideomotor apraxia.
The prognosis is better if the patient is young and the injury has been caused by a cerebral infarction since, thanks to brain plasticity, other brain regions can supply part of the function of the injured region.
Speech apraxia
Speech apraxias are described as the inability to reproduce the necessary motor sequence with the mouth to be able to speak clearly and intelligibly. It can occur in both adults and children of learning age to speak, although in childhood patients it is often called dyspraxia of verbal development.
This type of apraxia is caused by lesions in the regions in the motor areas that control the muscular movement of the mouth, although cases of patients with lesions in the insula and in Broca's area have also been found..
Although it is in English, in the following video you can see children with apraxia of speech from minute 1:55 on:
These lesions are usually caused by a heart attack or a tumor, but they can also be a consequence of the neuronal degeneration typical of neurodegenerative diseases such as Alzheimer's.
Speech apraxias are usually diagnosed by a language specialist, who must carry out an exhaustive examination of the patient's deficits that includes tasks such as pursing the lips, blowing, licking, raising the tongue, eating, speaking ...
You should also perform a physical examination of the mouth to verify that there are no muscle problems that prevent the patient from speaking correctly. The diagnosis is usually supported by magnetic resonance imaging in which the damaged regions can be seen.
Most apraxias of speech caused by heart attack usually recover spontaneously, but those caused by neurodegenerative disorders usually require the use of therapies. Of the therapies studied, those that have shown greater effectiveness are those that include exercises to produce sounds and repetitions of speed and rhythm.
These sound exercises are usually performed with the support of the professional in terms of the positioning of the muscles and the articulatory movement. These treatments usually work well and are effective in the long term..
Gait apraxia
Gait apraxia is defined as the inability to move the legs to be able to walk naturally, without the patient having any paralysis or muscle problems.
This type of apraxia usually occurs in elderly people who have suffered an ischemia, magnetic resonance imaging usually shows a dilation of the ventricles, which are involved in the correct movement of the lower limbs.
In addition to gait problems, patients often present other symptoms such as urinary incontinence, imbalance and even cognitive deficits.
If left untreated, patients with this type of disorder may experience total paralysis of their lower limbs and severe cognitive deficits..
One type of therapy that is proving to be quite effective is magnetic stimulation, in a study by Devathasan and Dinesh (2007) it was shown that patients treated with magnetic stimulation in motor areas for a week significantly improved their way of walking.
Kinetic apraxia of the extremities
The kinetic apraxia of the extremities, as its name suggests, implies a deficit in the fluid movement of both the upper and lower extremities..
People who suffer from this disorder usually have problems with both gross motor skills (moving arms and legs) and fine motor skills (moving fingers, writing, picking up things ...).
This type of apraxia usually occurs due to the degeneration of motor neurons, located in the frontal and parietal lobes, as a consequence of a neurodegenerative disorder such as Parkinson's or Multiple Sclerosis, although it can also occur as a cause of a cerebral infarction.
The treatment of kinetic apraxias usually focuses on training the patient in the use of everyday objects to improve their quality of life..
Orofacial or facial-oral apraxia
Patients suffering from orofacial apraxia are unable to properly control the muscles of the face, tongue and throat, therefore, they have problems chewing, swallowing, winking, sticking out the tongue, etc..
This disability occurs when the person intends to perform the movements on purpose and not when they are involuntary, that is, it only occurs when the person thinks about the movements before performing them..
Orofacial apraxias usually occur together with kinetic apraxias of the extremities. The relationship between these two types of apraxia is not yet known, since kinetic apraxia usually occurs after suffering injuries in the frontal and parietal lobe, while the injuries suffered by people who suffer orofacial apraxia have very different locations such as the cortex prefrontal, insula, or basal ganglia.
Biofeedback treatment has been shown to be effective in this type of apraxia, but it is not yet known whether this treatment is effective in the long term. Biofeedback treatment consists of the provision of sensors that detect the muscular activation of the face and mouth, in this way the professional can observe the muscles that the patient is trying to move and correct them if necessary..
Oculomotor apraxia
Oculomotor apraxia involves the difficulty or inability to perform eye movements, especially saccades (moving the eyes to the side) intended to direct the gaze to a visual stimulus..
This type of apraxia differs from the previous ones in that it can occur both in an acquired and congenital form, that is, it can occur from birth due to the inheritance of a gene. Congenital oculomotor apraxia can be of several types depending on the affected gene.
One of the most studied is type 2 oculomotor apraxia, caused by a mutation in the SETX gene. This apraxia is a characteristic symptom of Gaucher disease, which is degenerative and unfortunately often causes early death in children who suffer from it. The most severe cases usually require a bone marrow transplant.
When apraxia is acquired it is usually due to lesions in the corpus callosum, cerebellum and fourth ventricle, usually caused by several cerebral infarcts.
References
- Guérin, F., Ska, B., & Belleville, S. (1999). Cognitive processing of drawing abilities. Brain Cogn, 464-478. doi: 10.1006 / brcg.1999.1079
- Heilman, L. R. (1982). Two forms of ideomotor apraxia. Neurology (NY), 342 - .
- Katz, W. F., Levitt, J. S., & Carter, G. C. (2003). Biofeedback treatment of buccofacial apraxia using EMA. Brain and Language, 75-176. doi: 10.1016 / S0093-934X (03) 00257-8
- Mohr, J., Lazar, R. M., Marshall, R. S., & Hier, D. B. (2004). Middle Cerebral Artery Disease. In J. Mohr, D. W. Choi, J. C. Grotta, B. Weir, & P. A. Wolf, Stroke (pp. 123-151). Philadelphia: Elsevier.
- Raade, A. S., Gonzalez Rothi, L. J., & Heilman, K. M. (1991). The relationship between buccofacial and limb apraxia. Brain and cognition, 130-146. doi: 10.1016 / 0278-2626 (91) 90002-P
- Tada, M., Yokoseki, A., Sato, T., Makifuchi, T., & Onodera, O. (2010). Early-onset ataxia with ocular motor apraxia and hypoalbuminemia / ataxia with oculomotor apraxia 1. Advances in Experimental Medicine and Biology, 21-33.
- Vromen, A., Verbunt, J., Rasquin, S., & Wade, D. (2011). Motor imagery in patients with a right hemisphere stroke and unilateral neglect. Brain Inj, 387-393. doi: 10.3109 / 02699052.2011.558041
- Wheaton, L., & Hallett, M. (1-10). Ideomotor apraxia: a review. Neurol Sci, 2007. doi: 10.1016 / j.jns.2007.04.014


Yet No Comments