
Uterine atony


What is uterine atony?
Uterine atony is the medical term that is used to describe a serious pathological condition that occurs in some women after childbirth and that has to do with the inadequate contraction of the muscles of the uterus after delivery, resulting in a postpartum hemorrhage.
Uterine atony is one of the 5 most common causes of maternal mortality, causing between 50 and 70% of cases of severe postpartum hemorrhage, that is, the loss of large amounts of blood due to the rupture of related blood vessels with the female reproductive system after giving birth.
This condition, listed as a obstetric emergency, It is a consequence of the fact that, after childbirth, the muscle cells that form the walls of the uterus fail to contract again, preventing compression of the blood vessels that supplied the placenta with blood..
The uterus
To better understand what uterine atony is about, it is necessary to keep in mind some basic notions about the uterus, which is one of the organs that are part of the set of reproductive organs of women and other animals.
The uterus is a hollow muscular organ, best described as a coat inverted pear-shaped, where fetuses get food and protection during the gestation months. It has three parts:
- The fundus o background uterine, which is the upper part, is located above the entry sites of the uterine tubes.
- The Body is the place where the embryo is implanted and where it develops during pregnancy.
- The cervix is the lower area and connects with the vagina.
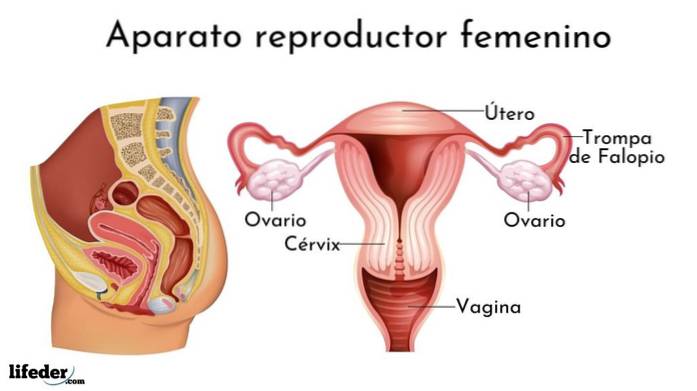
Both the fundus and the corpus uteri are made up of three layers of tissue known as the peritoneum, the myometrium and the endometrium.
The peritoneum, also known as perimetrium, it is a continuous membrane with the abdominal peritoneum; the myometrium is a thick muscular layer and the endometrium is the mucous membrane that lines the inside of the uterus.
During pregnancy, the muscle cells of the myometrium undergo some modifications that allow the tissue to which they belong to expand to house the fetus and, during delivery, these cells contract to expel both the baby and the placenta that fed it.
The maternal vascular tissue, which supplied the developing fetus with blood and nutrients through the placenta, ruptures when delivery occurs. However, under normal conditions, blood loss is minimal, as the myometrium contracts, compressing the “broken” blood vessels and maintaining blood pressure. hemostasis.
Signs and symptoms of uterine atony
One of the main signs that a patient is suffering uterine atony is, as we discussed, that the muscular walls of your uterus remain relaxed after delivery, causing bleeding.
The diagnosis is usually made through a physical examination by the treating physician after delivery, whether it was a natural delivery or a cesarean section..
The examination is manual, as the physician must ensure that the uterus is not abnormally large, boggy, or too soft. In some cases it is also necessary to obtain ultrasound images.
Since this pathology causes bleeding, another of the signs that the doctor takes into account is the fact that there is more blood loss than occurs in a normal delivery. Thus, other symptoms include those related to bleeding:
- Decreased blood pressure
- Accelerated heart rate
- Headache
- Dizziness
- Loss of consciousness
- Paleness and cooling of the skin
- Body weakness
- Difficulty breathing
It is important to mention that the obstetrician in charge of the woman who gives birth must make some differential diagnoses, to rule out any other reason for the bleeding that is different from the atony of the uterus.
Causes
Among the most commonly indicated causes for uterine atony by specialists are:
- Having had a prolonged labor
- Having labor too fast
- Having used some drugs such as exogenous oxytocin
- Having undergone deep anesthesia during childbirth
- Have had an induced labor
Risk factor's
The risk factors associated with uterine atony are diverse and some of them are:
- Having multiple pregnancies, where more than one fetus develops at the same time, such as twins or triplets, for example
- That the baby has fetal macrosomia, that is, that it has a size and weight above the average
- Exaggerated accumulation of amniotic fluid (polyhydramnios) occurs
- Having high levels of oxytocin, a peptide hormone that participates in contraction during labor, but whose excess can produce a desensitization, limiting its functions, ergo, not achieving myometrial contraction
- That the placenta has been removed manually
- Having had previous postpartum hemorrhages
- Having a condition of obesity, that is, a body mass index greater than 40
- Be over 35 years old
- Having anemia
Treatment
Good medical practice implies that the obstetrician in charge is aware of the physiological conditions of his patient before delivery, both of their conditions immediately before, and of any previous condition or pathology that the patient may suffer and that represents a risk factor for bleeding caused by uterine atony.
For this reason, some measures that are included in the treatment may be previous, especially when it comes to patients with a history or at risk. Among these measures are the review of certain blood parameters and the review of medical history.
During labor, however, appropriate patient management includes uterine massage during the third phase of labor, oxytocin infusion, and low-level umbilical cord traction..
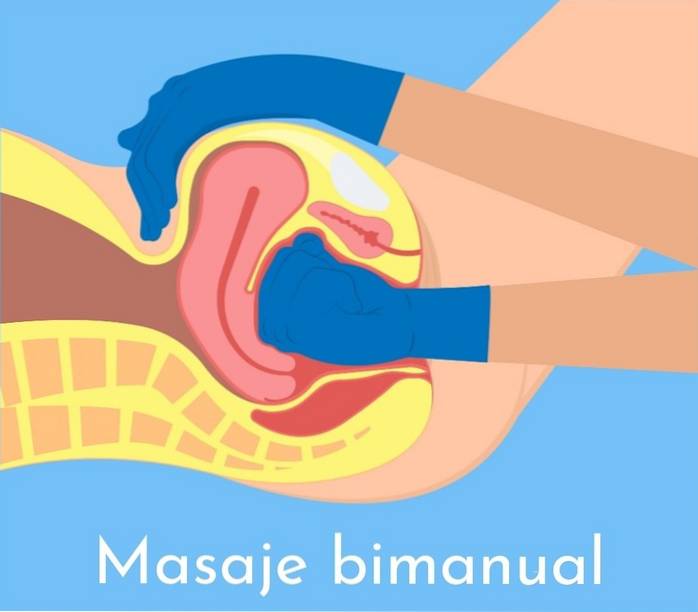
If uterine atony occurs, the procedure generally involves: doing a bimanual massage of the uterus, as shown in the image, administering some drugs that induce contraction of the uterus and / or beginning the administration of fluids intravenously.
The most commonly used drugs for the treatment of uterine atony and for the prevention of the development of severe bleeding are:
- Oxytocin: intravenous or intramuscular (10-40 units per 1,000 ml)
- Methylergonovine: intramuscular (0.2 mg every 2 or 4 hours)
- 15-methyl-PGF2-alpha: intramuscular (0.25 mg every 15 or 90 min, maximum 8 doses)
- Misoprostol: rectally (800-1000 mg)
- Dinoprostone: vaginal or rectal suppository (20 mg every 2 hours)
Surgical treatment
In the event that the medication does not induce the contraction of the uterine walls or reduce blood loss, then surgical methods are generally used, among which are:
- Applying gauze to the uterus, which necessarily involves the application of a catheter to drain the urinary bladder.
- Application of a Bakri balloon, which is specially designed for hydrostatic compression of the uterus. The introduction of a Bakri balloon is a common surgical practice for the treatment of bleeding caused by uterine atony, since the hydrostatic pressure exerted by the balloon against the walls of the uterus causes compression of the broken blood vessels.
- Uterine curettage to remove retained products.
- Ligation of retained arteries.
- Compression sutures.
- Hysterectomy or removal of the uterus.
References
- Breathnach, F., & Geary, M. (2009, April). Uterine atony: definition, prevention, nonsurgical management, and uterine tamponade. In Seminars in perinatology (Vol. 33, No. 2, pp. 82-87). WB Saunders.
- Gill P, Patel A, Van Hook JW. Uterine Atony. [Updated 2020 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493238/
- Jones, R. E., & Lopez, K. H. (2013). Human reproductive biology. Academic Press.
- Moore, K. L., Persaud, T. V. N., & Torchia, M. G. (2018). The Developing Human-EBook: Clinically Oriented Embryology. Elsevier Health Sciences.
- Wetta, L. A., Szychowski, J. M., Seals, S., Mancuso, M. S., Biggio, J. R., & Tita, A. T. (2013). Risk factors for uterine atony / postpartum hemorrhage requiring treatment after vaginal delivery. American journal of obstetrics and gynecology, 209 (1), 51-e1.



Yet No Comments