
Bacteriostatic characteristics, mechanisms of action and examples

The drugs bacteriostatic They are antibiotics that reversibly stop the reproduction and growth of bacteria. They are used against infections by sensitive microorganisms and in patients with a competent immune system.
Pasteur and Joubert were the first to recognize the potential therapeutic effect of some microbial products. In 1877 they published their observations, where they showed how common microorganisms could stop the growth of the Anthrax bacillus in urine..
Streptomycin, chloramphenicol, and chlortetracycline were identified at the end of World War II. Since that time, hundreds of antimicrobial drugs have been developed and these are available for the treatment of different infectious diseases..
Currently, antibiotics are one of the most used drugs in medical treatment, more than 30% of hospitalized patients receive antibiotics. However, they are one of the most misused drugs by doctors and patients. Unnecessary and mismanaged therapies with these drugs have been the cause of the development of bacterial resistance against many antibiotics.
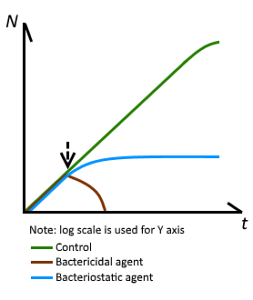
Antimicrobials are classified, according to their general mechanism of action, as bactericidal (those that kill bacteria) and bacteriostatic (those that inhibit their growth and reproduction). While this differentiation is clear when tested in vitro, when used in therapeutics this distinction is not so defined.
Article index
- 1 Features
- 2 Mechanism of action
- 3 Mechanism of action in the case of bacteriostats
- 3.1 Inhibition of the activation phase
- 3.2 Inhibition of the initiation of protein synthesis
- 3.3 Inhibition of elongation by various mechanisms
- 4 Examples of each mechanism of action and sensitive microorganisms
- 4.1 Activation phase inhibitors
- 4.2 Inhibition of the initiation of protein synthesis
- 4.3 Inhibition of the binding of aminoacyl-tRNA to the ribosome
- 4.4 Elongation inhibitors
- 4.5 Macrolides
- 5 References
Characteristics
As explained above, antimicrobial drugs can be classified into those capable of killing sensitive bacteria, which are called bactericides, and those that reversibly inhibit their growth and development, called bacteriostats..
Currently, this differentiation is considered, from a clinical point of view, somewhat diffuse. For this reason it is said that a given antibiotic acts preferentially as a bacteriostatic or a bactericide..
Therefore, the same antibiotic can have a dual effect (bacteriostatic or bactericidal) depending on certain conditions such as the concentration that it can reach in the area where its effect is needed and the affinity it has for the microorganism involved..
In general, bacteriostats, with the exception of aminoglycosides, are antibiotics that interfere with the protein synthesis of sensitive bacteria. If the body's immune system is a competent system, it is enough to inhibit the growth and reproduction of a bacterium so that it can eliminate it.
On the other hand, bactericides can have different mechanisms of action: they can interfere with the synthesis of the bacterial cell wall, alter the cytoplasmic membrane or interfere with some processes related to the synthesis and metabolism of bacterial DNA..
Mechanism of action
Several schemes have been used to classify antimicrobial drugs, among them is the grouping of these drugs according to common mechanisms of action. Thus, according to their mechanism of action, antibiotics are classified into:
- Antibiotics that inhibit the synthesis of the bacterial wall: among which are penicillins and cephalosporins, cycloserine, vancomycin and bacitracin.
- Antibiotics that alter the membrane permeability of microorganisms, allowing intracellular compounds to escape: this includes detergents such as polymyxin and polyene.
- Agents that affect the function of the 30S and 50S ribosomal subunits and cause a reversible inhibition of protein synthesis: these are bacteriostatic drugs. Examples chloramphenicol, tetracyclines, erythromycin, clindamycin, and pristanamycin.
- Agents that bind to the 30S subunit and alter protein synthesis and eventually cause the death of the bacteria: among these are aminoglycosides.
- Antibiotics that affect nucleic acid metabolism inhibit RNA polymerase: rifamycin is an example.
- Antimetabolite agents that inhibit folate metabolism enzymes - examples of these are trimethoprine and sulfonamides.
Mechanism of action in the case of bacteriostats
The mechanism of action of bacteriostatic agents has to do with the alteration of the protein synthesis of the target bacteria. This is achieved by various mechanisms:
Activation phase inhibition
- Isoleucyl-tRNA synthetase enzyme inhibitors.
Inhibition of the initiation of protein synthesis
- Prevent formation of the 70S initiation complex or bind to the 50S subunit.
- Inhibition of the binding of aminoacyl-tRNA to the ribosome.
Inhibition of elongation by various mechanisms
- Interfering with the transpeptidation process.
- Interfering with peptidyltransferase, in the 23S rRNA of the 50S subunit of the ribosome.
- Inhibiting elongation factor G translocation.
A separate case includes the mechanism of action of aminoglycosides, since they act on the 30S ribosomal subunit, thus interfering with protein synthesis and therefore are bacteriostatic. However, they exert an effect on the membrane of some bacteria, which causes a mainly bactericidal effect..
Examples of each mechanism of action and sensitive microorganisms
Activation phase inhibitors
Mucopyrocin is a bacteriostatic antibiotic capable of competitively inhibiting the enzyme isoleucyl-tRNA synthetase, thus inhibiting the incorporation of isoleucine and stopping synthesis..
This antibiotic is synthesized by some species of Pseudomonas, so it is extracted from there. It has an especially powerful effect against gram-positive bacteria. It is used primarily for skin infections, topically, or for the eradication of the healthy carrier state of Staphylococcus aureus.
Inhibition of the initiation of protein synthesis
In bacteria, the initiation of synthesis occurs with the incorporation of methionine as formylmethionine linked to a tRNA (transfer RNA). The 30S and 50S ribosomal subunits participate in the initiation complex, with two important loci: Locus A and Locus P.
The group of oxazolidinones and aminoglycosides exhibit this mechanism of action. The group of oxazolidinones is a group of synthetic antibiotics recently introduced into clinical practice, which do not exhibit cross-resistance with other bacteriostatic antibiotics..
Linezolid is the representative of the oxazolidinones, it is active against gram-positive bacteria, including strains of Staphylococcus aureus and of Streptococcus spp. multiresistant and have no activity against gram-negative agents.
Aminoglycosides are of natural origin, they are synthesized by actinomycetes in the soil or from semisynthetic derivatives thereof. They are active against a wide variety of bacterial species, especially against aerobic gram-negatives.
Depending on the bacteria and its location, they can exhibit a bacteriostatic or bactericidal effect..
Inhibition of the binding of aminoacyl-tRNA to the ribosome
The tetracyclines and their derivatives, the glycylcyclines, are representatives of this group. They block or inhibit Locus A. Tetracyclines can be naturally occurring (streptomyces) or semisynthetic; These include doxycycline, minocycline, and oxytetracycline..
Tigecycline is a glycylcycline derived from minocycline, with the same mechanism of action, but with five times more affinity than minocycline and which also affects the cytoplasmic membrane. They are very active against enterococci and against many bacteria resistant to other antibiotics.
Elongation inhibitors
Chloramphenicol and lincosamides are examples of this group, acting on the P locus. Fusinic acid is an example of the mechanism of inhibition of the translocation of elongation factor G. Macrolides and ketolides bind to peptidyltransferase, in the 23S rRNA of the 50S subunit of the ribosome.
Chloramphenicol and its derivatives such as thiamphenicol are broad spectrum bacteriostatic antibiotics against gram-positive and negative and against anaerobics. They are very active against salmonella and shigella, as well as against bacteroides, with the exception of the B. Fragilis.
The main lincosamide is clindamycin, which is a bacteriostatic, however, depending on the dose, its concentration in the target and the type of microorganism, it can exhibit a bactericidal effect..
Clindamycin is effective against gram-positive agents, with the exception of enterococci, it is of choice for B. fragilis and it is effective against some protozoa like Plasmodium Y Toxoplasma gondii.
Macrolides
These drugs include erythromycin, clarithromycin, and roxithromycin (as 14-carbon macrolides) and azithromycin (as 15-carbon group). Spiramycin, josamycin, and midecamycin are examples of 16-carbon macrolides.
Telithromycin is a ketolide derived from erythromycin. Both macrolides and ketolides are active against gram-positive bacteria, Bordetella pertussis, Haemophilus ducreyi, Neisseria ssp, Helicobacter pylori (clarithromycin is more effective) and Treponemes, among others.
References
- Calvo, J., & Martínez-Martínez, L. (2009). Mechanisms of action of antimicrobials. Infectious diseases and clinical microbiology, 27(1), 44-52.
- Goodman and Gilman, A. (2001). The pharmacological basis of therapeutics. Tenth edition. McGraw-Hill
- Meyers, F. H., Jawetz, E., Goldfien, A., & Schaubert, L. V. (1978). Review of medical pharmacology. Lange Medical Publications.
- Ocampo, P. S., Lázár, V., Papp, B., Arnoldini, M., Zur Wiesch, P. A., Busa-Fekete, R.,… & Bonhoeffer, S. (2014). Antagonism between bacteriostatic and bactericidal antibiotics is prevalent. Antimicrobial agents and chemotherapy, 58(8), 4573-4582.
- Rodríguez-Julbe, M. C., Ramírez-Ronda, C. H., Arroyo, E., Maldonado, G., Saavedra, S., Meléndez, B.,… & Figueroa, J. (2004). Antibiotics in older adults. Puerto Rico health sciences journal, 2. 3(1).


Yet No Comments