
Basophils characteristics, morphology, functions, diseases

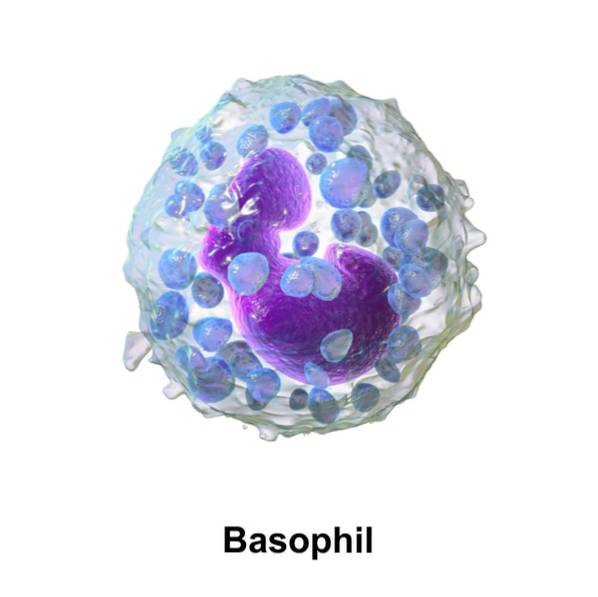
The basophils, or basophilic leukocytes, are non-phagocytic granulocytes whose cytoplasmic granules release substances that defend the body from endo and ectoparasites, and which are important in inflammation and allergies. They are the smallest (5-15 μm in diameter) and least numerous (0-2%) of leukocytes (white blood cells).
Polymorphonuclear leukocytes get their name from having lobulated nuclei. They are also called granulocytes because their cytoplasm contains granules that can be easily colored. They include neutrophils, eosinophils, and basophils, whose names refer to the affinity of their cytoplasmic granules for specific dyes..
In basophils, the cytoplasmic granules, which are uniform in size and overshadow the nucleus, turn blue due to the action of chemically basic dyes, such as hematoxylin and methylene blue, which bind to the histamine and heparin present in their inside.
Functionally, basophils, which are blood cells, are similar to mast cells, which are tissue cells. Both types of cells possess Fc receptors. These cell surface receptors owe their name to the fact that they show a high affinity for the Fc region of immunoglobulin E (IgE) antibodies..
Article index
- 1 Features
- 2 Morphology
- 3 Bioactive compounds of the granules
- 4 Life cycle
- 5 Activation
- 6 Functions
- 7 Inflammation
- 8 Normal Values
- 8.1 High and low basophils
- 9 Related diseases
- 9.1 Allergies
- 9.2 Myeloproliferative disorders
- 10 References
Characteristics
Undergoing staining procedures, basophils can be observed by light microscopy. Because they are not abundant in the blood, it is convenient to isolate and purify them previously.
They have a specific gravity (1.070-1.080 g / mL) similar to that of monocytes and lymphocytes, which is why centrifugation of the blood separates these three types of cells together. Centrifugation makes it possible to isolate basophils with a purity of 1-20%. Additional techniques are required to achieve higher purities.
Basophils are more abundant in inflamed tissues than in blood. Its identification in these tissues requires monoclonal antibodies..
Compared to mast cells, basophils are activated by more types of artificial stimuli, including calcium ionophores (ionomycin, polybasic amines), and tumor-producing phorbol esters that in turn activate kinase C.
Basophils express receptors for immunoglobulin G (IgG), complement, cytokine, chemokine, histamine, certain short peptides and soluble lipids, histamine, various peptidases, and many adhesion molecules of the integrin and selectin families. In this characteristic, they are more like eosinophils than mast cells..
Morphology
Electron microscopy shows that basophils have: 1) a cell surface with multiple, irregular, short and thick projections; 2) two types of granules, a smaller one close to the nucleus and a larger one containing electron opaque matter; 3) an elongated and curved nucleus with strong condensation of ultrastructurally segmented chromatin.
Although basophils are blood cells, in response to the release of chemotaxins and chemokines during inflammation, they penetrate the tissues in which functionally similar mast cells are found..
Morphologically, basophils are distinguished from mast cells by having a smaller number of larger granules (up to 1.2 μm), and non-rounded nuclear lobes. Furthermore, basophils lack intragranular coils, which represent the diagnostic ultrastructure of mast cells..
Basophil granules, like those of mast cells, are rich in proteoglycans composed of a polypeptide core and multiple unbranched glycosaminoglycan side chains. The latter impart a strong negative charge to the molecules, which explains the staining with basic dyes..
Basophils share with eosinophils the characteristic of having the Charcot-Leyden crystalline protein in their granules.
Bioactive compounds in the granules
Basophil granules contain biogenic amines, proteoglycans, and enzymes. Biogenic amines are low molecular weight compounds with an amino group. Proteoglycans include heparin and chondroitin sulfate. Enzymes include proteases and lysophospholipases, which can cause tissue damage.
The most important of the biogenic amines is histamine, which diffuses rapidly in the blood and tissues. Histamine has vasodilatory effects and increases vascular permeability, which is manifested in redness and local hyperthermia. It also contracts the smooth muscle of the bronchi, producing bronchospasm in asthmatics exposed to allergens..
Due to their strong negative charge, within the granules, heparin and chondroitin sulfate bind to positively charged biogenic amines and proteases. Upon exiting the granules, heparin and chondroitin sulfate release biogenic amines and proteases.
Lifecycle
Like other blood cells and mast cells, basophils originate from hematopoietic cells.
The blood carries mast cell progenitor cells to the tissues, where they proliferate and mature. Basophils mature in hematopoietic tissues. Like other granulocytes, they do not proliferate once they pass into the blood..
Two days after the basophils have reached their mature morphology, they are released into the blood, in which they have very short half-lives (about one day). Therefore, these cells need to be continually replaced. However, basophils can survive for a longer time (probably up to several weeks) in tissues..
The life cycle of basophils can culminate in two different ways. If they have undergone degranulization (discharge of the content of their granules), having therefore fulfilled their function, they become necrotic. If they have remained intact, that is, if they have not undergone degranulization, they perish by apoptosis.
Basophil residues present in tissues and in the circulatory system are phagocytosed and thus eliminated by other leukocytes.
Activation
Basophils are effector cells of immune and allergic reactions. They rapidly release chemical mediating compounds, with inflammatory effects, during IgE-dependent reactions that respond to the presence of allergenic substances, such as those that cause rhinitis, asthma and anaphylaxis..
Said compounds can be synthesized and stored (examples: histamine; proteoglycans, biogenic amines) during the differentiation and maturation of basophils, or synthesized (examples: cytokines; lipid mediators; IL-4 and IL-13; leukotriene C4, which is an arachidonic acid derivative) at the time of activation.
The activation of basophils is due to the cross-reaction of IgE bound to the IgE receptors on their surface (IgEr). Molecules produced during inflammation can activate them.
Several enzymes (such as serine protease, phospholipases A and C, methyltransferases, phosphodiesterase and adenylate cyclase) linked to the surface of the cell membrane play a fundamental role in the activation of basophils, causing them to degranulate and therefore release mediators. mainly histamine and leukotriene C4.
The phases of basophil activation are: 1) sensitization, IgE antibodies produced in response to antigens bind to specific basophil receptors; 2) activation, re-exposure to antigens causing degranularization; (3) effector response, allergic manifestations in response to inflammatory mediators released by the granules.
Features
Like all leukocytes, basophils participate in the immune response against organisms that threaten the integrity of the body. An important difference of basophils (and eosinophils) from other leukocytes is their ability to neutralize multicellular endoparasites (helminths) too large to be phagocytosed..
Basophils use the substances in the granules to attack these endoparasites, piercing their protective cuticle. This immune response is dominated by IgE antibodies, which recognize the antigens on the surface of endoparasites. Basophils show high affinity for IgE antibodies.
During roundworm infections Ascaris lumbricoides there is elevation of serum IgE levels. Immunization with antigens of this helminth induces the formation of IgE.
Basophils also help reject ectoparasites, such as the tick Haemaphysalis longicornis. The cutaneous edema produced by these cells can prevent the tick from locating the host's blood vessels..
Endoparasites employ mechanisms of evasion (encystment, molecular camouflage, antigenic variation) of the immune response, and of suppression of the effector pathways of the immune response.
Basophils, along with mast cells and eosinophils, are also involved in angiogenesis, tissue remodeling, and the response to cancer..
Inflammation
The inflammatory properties of basophils, mast cells, and eosinophils are an integral component of the immune response and have evolved because they possess a protective function against parasites and infections. However, these inflammatory properties are also the cause of diseases.
The three named cell types produce lipid mediators and cytokines. They are unique cells because they store histamine (an inflammatory molecule) and have membranes with a large number of receptors with a high affinity for IgE (involved in inflammation)..
Lipid mediators induce blood leakage, bronchoconstriction, and intestinal hypermotility, which are components of the immediate immune response. Lipid mediators and cytokines contribute to inflammation, which is a component of the late immune reaction.
Basophils are the blood equivalent of mast cells, which are strictly tissue. Eosinophils are primarily tissue, but are also found in the circulatory system. Due to their location, mast cells are the first to activate. Molecules secreted by mast cells attract basophils and eosinophils to affected tissues.
Basophils produce mediators that constrict the smooth muscles of the airways. Found in large numbers in the lungs after fatal asthma episodes and on inflamed skin.
Normal values
Due to differences in quantification procedures, “normal” values for basophils vary between authors and clinical laboratories. A representative range of values for adult individuals would be 0.02-0.10 × 109 basophils for each liter of blood, or what is the same, 20-100 basophils for each cubic millimeter of blood.
Basophil values depend on age and change throughout the day due to the influence of hormones. They are also affected by environmental temperature, increasing in number during hot seasons and in the face of sudden cooling of the environment..
High and low basophils
Possession of a number of basophils higher than normal is called basophilia. This condition is seen in blood diseases, including polycythemia vera, myelofibrosis, thrombocythemia, and myeloid leukemia..
It is also seen in other diseases, including allergies, estrogenic abnormalities, juvenile rheumatoid arthritis, ulcerative colitis, diabetes mellitus, hypothyroidism, infections and parasites, autoimmune inflammation, myxedema, and myeloproliferative neoplasms..
The number of basophils may drop below normal values in response to diseases, or under certain physiological conditions, such as surgery, diarrhea, hyperthyroidism, infections, anaphylactic manifestations, ovulation, severe allergic reaction, hypersensitivity reactions, glucocorticoid therapy, thyrotoxicosis and trauma.
Related diseases
Allergies
Allergies are various forms of inflammation, technically known as type I hypersensitivity reactions, due to an overreaction to an allergen (antigen) to which you have been previously exposed. The clinical manifestations of type I hypersensitivity include skin allergies, allergic rhinitis, and asthma..
When the allergic reaction is severe it is called anaphylaxis. The most serious form of anaphylaxis, called anaphylactic shock, can be fatal. The treatment of choice is the injection of epinephrine (adrenaline).
The fundamental components of the allergic response are: 1) exposure to the antigen; 2) immunoglobulin E (IgE); 3) IgE receptors on basophils and mast cells; 4) the release of histamine and cytokines into the blood and tissues by these cells as a result of the interaction IgE-IgE receptors.
The allergic response is rapid since it occurs within a few minutes of exposure to the antigen. The role of basophils in the allergic reaction is manifested in their rapid recruitment at the site of contact with the allergen, be it the skin, nasal mucosa or lungs..
Myeloproliferative disorders
Myeloproliferative disorders are malignant diseases of the bone marrow that lead to excessive proliferation of red blood cells, granulocytes, and platelets. The four main myeloproliferative disorders are polycythemia vera, myelofibrosis, thrombocythemia, and myeloid leukemia..
Polycythemia vera is a bone marrow disorder that leads to the overproduction of all three types of blood cell lines (leukocytes, erythrocytes, platelets). Progresses slowly and can lead to myelofibrosis and acute leukemia.
Myelofibrosis is fibrosis of the bone marrow. It leads to severe anemia and causes an enlarged spleen. Progresses slowly and can lead to preleukemic disorders.
Thrombocythemia is the possession of an abnormally high number of platelets. Also known as thrombocytosis.
Myeloid leukemia is cancer of the blood cells belonging to the myeloid line (granulocytes, monocytes, erythrocytes). It can be chronic or acute.
The association of myeloproliferative disorders with basophilia produces serious biochemical and immunological disorders. For example, elevated intracellular histamine and histidine decarboxylase.
References
- Abbas, A. K., Lichtman, A. H., Pillai, S. 2017. Cellular and molecular immunology. Elsevier, Amsterdam.
- Bochner, B. S., Schroeder, J. 2001. Basophils. In: Austen, K. F., Frank, M. M., Atkinson, J. P., Cantor, H., eds. Samter's immunologic diseases, Volume I. Lippincott Williams & Wilkins, Philadelphia.
- Bos, J. D. 2004. Skin immune system cutaneous immunology and clinical immunodermatology. CRC Press, Boca Raton.
- Delves, P. J., Martin, S. J., Burton, D. R., Roitt, I. M. 2017. Roitt's essential immunology. Wiley, Chichester.
- Eales, L.-J. 2003. Immunology for life scientists. Wiley, Chichester.
- Falcone, F. H., Haas, H., Gibbs, B. F. 2000. The human basophil: a new appreciation of its role in immune responses. Blood, 96, 4028-4038.
- Galli, S. J. 2000. Mast cells and basophils. Current Opinion in Hematology, 7, 32-39.
- Hoffman, R., Benz, E. J., Jr., Silberstein, L. E., Heslop, H., Weitz, J. I., Anastasi, J., Salama, m. E., Abutalib, S. A. 2017. Hematology: basic principles and practice. Elsevier, Amsterdam.
- Lazarus, H. M., Schmaier, A. H. 2019. Concise guide to hematology. Springer, Cham.
- Longo, D. L. 2010. Harrison's hematology and oncology. McGraw-Hill, New York.
- Murphy, K., Weaver, C. 2016. Janeway's immunobiology. Garland Science, New York.
- Parham, P. 2014. The immune system. Garland Science, New York.
- Paul, W. E. 2012. Fundamental immunology. Lippincott Williams & Wilkins, Philadelphia.
- Pinchuk, G. 2002. Theory and problems of immunology. McGraw-Hill, New York.
- Prussin, C., Metcalfe, D. D. 2003. IgE, mast cells, basophils, and eosinophils. Journal of Allergy and Clinical Immunology, 111, S486-S494.
- Valent, P. 1995. Immunophenotypic characterization of human basophils and mast cells. Chemical Immunology, 61, 34-48.
- Valent, P., Bettelheim, P. 1990. The human basophil. Critical Reviews in Oncology and Hematology, 10, 327-352.


Yet No Comments