
Cytotrophoblast characteristics, development and function
The cytotrophoblast or Langhans cells, is the portion of the basement membrane of the trophoblast composed of mononucleated cells. This portion corresponds to the population of stem cells, from which the other trophoblasts are derived..
This layer of cells from the mitotic point of view, is very active, producing cells that bind to the syncytiotrophoblast. The cytotrophoblast originates from the implantation period of the blastocyst in mammalian embryonic development. During this phase of development, trophoblastic cells proliferate giving way to invasion into the endometrial epithelium..
Article index
- 1 Features
- 1.1 Extravillous cytotrophoblast
- 2 Development and function
- 2.1 Formation of the placenta
- 2.2 Maternal-fetal interface
- 2.3 The placental barrier separates maternal and fetal blood
- 3 References
Characteristics
A layer of mononucleated cells make up the cytotrophoblast, on the inner side of the trophoblast. These cells are located in the chorionic villi, and are covered by the syncytiotrophoblast. The cytotrophoblast is characterized by high cell differentiation and proliferation capacity and low functional activity.
During the embryo implantation phase or window, the cytotrophoblast cells originate, becoming cubic and pale with a good nuclear image, and well differentiated from each other..
The proliferation of cytotrophoblastic cells occurs through continuous cell multiplication. It is estimated that at least half of the cells in this layer are undergoing a cell cycle. In addition to proliferation, there is a high cell differentiation that generates the syncytiotrophoblast layer and the extravillous cytotrophoblast.
Extravillous cytotrophoblast
The extravillous cytotrophoblast is located externally on the chorionic villi. This cell layer proliferates rapidly invading the uterine stroma and the spiral arteries of the endometrium, reducing the resistance of the vascular walls. Two types of extravillous cytotrophoblast are distinguished: interstitial and endovascular.
In the interstitial, cells invade the myometrium to fuse and become large placental cells. These cells do not invade the vascular walls.
The endovascular, on the other hand, invades the vascular walls, destroying the smooth cells of the middle layer of the blood vessel, disposing of fibrinoid material instead. The diffusion of molecules that simulate an endothelial phenotype allows the endothelium of the maternal blood vessels to be replaced by a new internal surface.
Cytotrophoblast activity is regulated by genetic, transcription, growth, hormonal, and chemical factors (such as molecular oxygen concentration).
Development and function
In mammals, after fertilization of the ovum by a sperm, a series of cell divisions take place until the blastocyst is formed, which is a hollow cell sphere where the layer of peripheral cells gives rise to the trophoblast, while the cluster of internal cells originates the tissues of the embryo, being called embryoblast.
The blastocyst attaches to the endometrium during implantation. Trophoblastic cells begin to diffuse when they come into contact with the endometrium, thus differentiating between the cytotrophoblast and the syncytiotrophoblast..
In the human species, implantation occurs approximately on the sixth day after ovulation and fertilization of the ovum..
In some mammals, this phase is postponed for days, weeks, or even months, in order to avoid the arrival of a new calf at a non-beneficial time, such as in periods when resources are diminishing or while the mother is nursing another calf..
In animals such as bears, badgers, seals and camels there is a delay in the implantation window known as embryonic diapause..
The blastocyst remains in this state, without proliferation of cytotrophoblastic cells, due to hormonal action. This mechanism is triggered in response to environmental factors or prolonged lactation periods in the mother..
Formation of the placenta
The placenta is responsible for maintaining the developing fetus, and is derived from the chorion (fetal portion) and the decidua basalis (maternal portion). In it, gas and metabolite exchanges occur between the maternal and fetal circulations. This organ develops when differentiable villi originate.
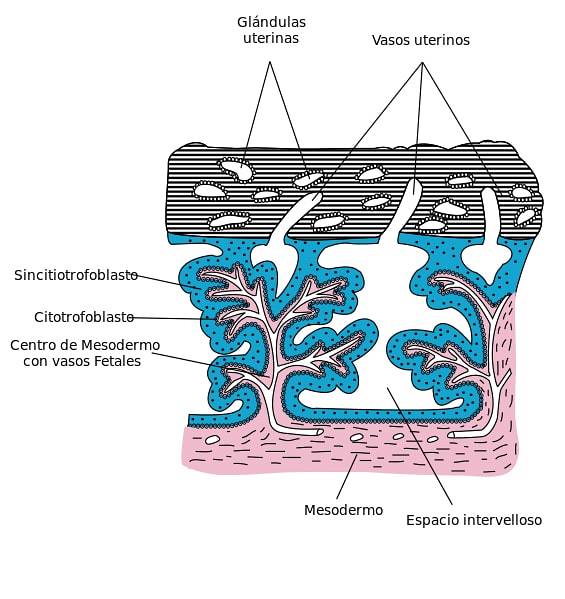
As cytotrophoblast cells expand and with the development of the chorionic mesentery and blood vessels, primary, secondary, and tertiary chorionic villi are formed.
The cytotrophoblast proliferates rapidly, passing its cells into pools of blood within the syncytiotrophoblast, forming the primary chorionic villi.
Subsequently, these villi are invaded by the embryonic mesenchyme of the chorion that remains inside and surrounded by the cytotrophoblast, thus forming the secondary villi that cover the chorionic sac.
Tertiary villi are formed with the appearance of blood vessels within the mesenchyme of the secondary villi.
As the tertiary villi form, threads or clusters of cells from the cytotrophoblast diffuse outward through the syncytiotrophoblast..
In this way, various cell agglomerates go outside and join each other, covering the syncytiotrophoblast with a cytotrophoblastic covering. This covering is interrupted where the maternal blood vessels pass to the inter-villous spaces.
Maternal-fetal interface
The first stage of the maternal-fetal interface consists of the invasion of the extravillous cytotrophoblast (located outside the placental villi) in the uterine spiral arteries, giving these arteries the characteristics of being of high caliber and having low resistance to flow. In this way, adequate perfusion for fetal growth is maintained..
In the second phase, the cytotrophoblast cells combine, undoing their cell membranes, to give rise to the multinucleated layer of the syncytiotrophoblast. The latter envelops the differentiated villi of the placenta.
The proper development of these two stages of the interface, ensure the correct placentation and therefore a successful fetal development and a safe progress of the state of pregnancy..
The placental barrier separates maternal and fetal blood
A placental barrier, formed essentially by the layers of fetal tissue, is responsible for separating the blood of the fetus from the maternal blood. In humans, from the fourth month of development, this barrier becomes very thin, facilitating the transfer of products through it..
The degeneration of the shell or cytotrophoblastic covering is the cause of the thinning of the placental barrier, in whose degenerated state it is composed of syncytiotrophoblast, discontinuous cytotrophoblastic covering, trophoblast basal lamina, villus mesenchyme, endothelial basal lamina and placental capillary endothelium fetal tertiary villi.
The placental barrier, in addition to separating the mother's blood and fetal blood, is responsible for the exchange of oxygen and carbon dioxide and metabolites between the maternal and fetal circulations.
References
- Hernández-Valencial, M., Valencia-Ortega, J., Ríos-Castillo, B., Cruz-Cruz, P. D. R., & Vélez-Sánchez, D. (2014). Elements of implantation and placentation: clinical and melecular aspects. Mexican Journal of Reproductive Medicine, 6 (2), 102-116.
- Hill, R. W., Wyse, G. A., Anderson, M., & Anderson, M. (2004). Animal physiology (Vol. 2). Sunderland, MA: Sinauer Associates.
- Kardong, K. V. (1995). Vertebrates: comparative anatomy, function, evolution. Ed. McGraw Hill.
- Rodríguez, M., Couve, C., Egaña, G., & Chamy, V. (2011). Placental apoptosis: molecular mechanisms in the genesis of preeclampsia. Chilean Journal of Obstetrics and Gynecology, 76 (6), 431-438.
- Ross, M. H., & Pawlina, W. (2007). Histology. Panamerican Medical Ed..
- Welsch, U., & Sobotta, J. (2008). Histology. Panamerican Medical Ed..



Yet No Comments