
He cells history, characteristics, cell cycle and uses
The HeLa cells they are a group of cancer cells that have been continuously cultured since 1951, when they were isolated from an African-American patient with a cervical malignant tumor. Her name is derived from the first two letters of the first and last name of the patient from whom they were obtained, Henrietta Lacks (HeLa). They are also called immortal cells, and it is the oldest cell line known and used by humans.
The discovery and development of HeLa cells in medical research has been a huge contribution to humanity. These cells have been used in more than 70 thousand investigations around the world.
They were a fundamental part in the development of the polio vaccine, and have been of great help in research related to cancer, HIV, genetic mapping, among many more..
Article index
- 1 History
- 1.1 HeLa cell cultures
- 2 Why Henrietta Lacks?
- 3 Features
- 4 Cell cycle
- 5 Uses
- 5.1 Other uses
- 6 Legal aspects
- 7 References
Story
The story of HeLa cells begins with an African-American patient diagnosed with cervical cancer in 1951. Henrietta Lacks arrived at Jhon Hopkins Hospital, located in Baltimore City, Maryland, USA, for a gynecological consultation due to atypical intermenstrual bleeding..
Said bleeding was recurrent after her last delivery and the patient also indicated that she felt a kind of knot in the uterus. An analysis of cervical cancer confirmed the medical suspicions. The patient had a tumor about 2.5 centimeters in diameter, easily palpable.
At that moment the doctors took Henrietta's first tissue sample for pathological analysis. Histopathological tests indicated that it was a squamous cell-type uterine cancer, that is, a malignant tumor with uncontrolled proliferation of cells..
The treating gynecologist mentioned that it seemed very atypical to him that after the last delivery of Mrs. Lacks, which had occurred just six weeks before, the analysis of the cervix (inner part of the uterus, at the end of the vagina) indicated that everything had a normal appearance. the date of diagnosis a tumor was found in such an advanced stage of development.
Before Henrietta Lacks began her cancer treatment, a hospital resident had taken a new cancer tissue sample from the patient and sent it to Dr. George Otto Gey's human and animal cell culture lab..
The patient did not react positively to cancer treatment, which consisted of deep radiation, and eight months after diagnosis Henrietta succumbed to the disease at the age of 31. One of the treating doctors said that he had never seen a type of cancer like that and never saw it again.
HeLa cell cultures
Dr. George Gey was a prominent tissue culture researcher at the John Hopkins Institute. This scientist was searching for years for an immortal cell line, that is, a group of cells that could divide unlimitedly under laboratory conditions (in vitro).
Gey and his wife had been trying for more than 20 years to obtain a cell line that they could maintain indefinitely under culture conditions. For this they had focused on cancer cells, however they did not achieve the expected results.
It was then that the gynecologist and head of the department of gynecology at the Jhon Hopkins Institute, Dr. Richard TeLinde, recommended that they use cervical cells, supplying them with the cells from the patient Henrietta Lacks..
When the cells were cultured, they began to multiply in an extraordinary way, at the rate of one generation every 24 hours. These results changed the lives of the Gey spouses as researchers, they also changed medicine and allowed them to innovate and create new fields of cell research.
Why Henrietta Lacks?
The discovery of HeLa cells was not a single patient or donor trial. On the contrary, the Geys had tried unsuccessfully to obtain adequate cell cultures from many cancerous tissues..
Following TeLinde's recommendation, the pair of researchers accessed cervical samples from various patients, but only those from Henrietta Lacks gave the desired results..
A study conducted 20 years after the death of Ms. Lacks revealed that the cancer that this patient suffered from was an aggressive type of adenocarcinoma of the cervix. Later it was also learned that the cells were infected with the human papillomavirus (HPV).
The HPV strain that infected these cells belongs to serotype 18, which is precisely associated with aggressive cancers of the human cervix.
The patient's medical history also indicated that she had syphilis. This, together with the presence of HPV serotype 18, could help explain the results obtained by the Gey spouses, regarding the rapid growth of these cells under laboratory conditions and their immortality..
Characteristics
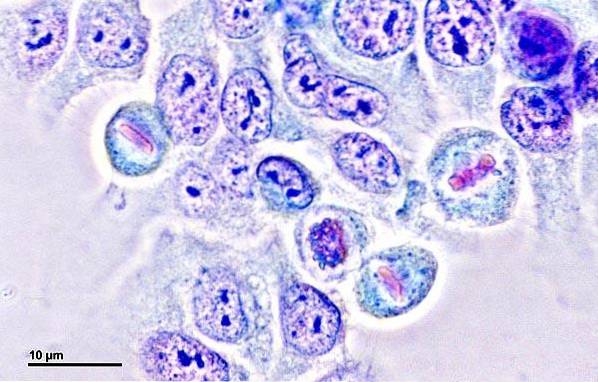
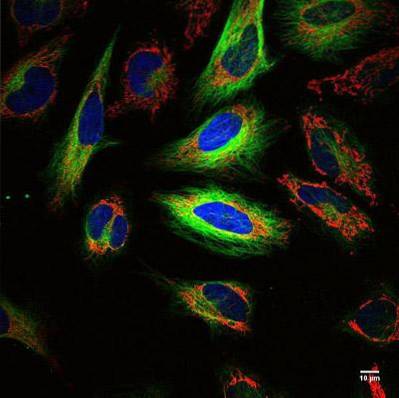
HeLa cells are cancer cells. They are 20 microns in diameter with a 10 micron core. Both its karyotype and its genome are unusual; on the one hand, genes are full of errors, and on the other, they have additional copies of some chromosomes, presenting between 76 and 80 total chromosomes.
They are infected by the human papilloma virus, the main cause of cervical cancer; this causes some chromosomes in HeLa cells to be heavily mutated.
They grow considerably faster, even for cancer cells; additionally, they are capable of contaminating and overcoming a wide variety of cell cultures, so extreme precautions must be taken when working with them.
They are cells called immortal, since they can divide infinitely under ideal conditions. They have an active version of a protein called telomerase during cell division.
This protein prevents HeLa cells from reaching the Hayflick limit. This limit was proposed by Leonard Hayflick and determines the number of times that a population of normal human cells reaches its maximum level of replication, and then enters the senescence phase..
Cellular cycle
The cell cycle of HeLa cells is not very different from the cell cycle of other normal human cells..
In eukaryotic cells (including HeLa), the cycle consists of 2 phases: an interface, where cells develop and duplicate their genetic material and organelles, and a mitotic phase, where the cell separates its genetic material, divides the cytoplasm and gives rise to a daughter cell.
HeLa cells in culture undergo a cell division cycle every 20 hours. Within this cycle the interface is the longest stage, with 19 hours, while the mitotic phase lasts only one hour. Normal cells can divide in a finite number of times, while Hela cells can repeat the cycle countless times..
Applications
Researchers have used HeLa cells in more than 70,000 investigations around the world. Its uses have been incredibly varied, some of them have been unethical and others have allowed great advances in medicine.
One of the most controversial cases of the use of HeLa cells occurred in 1954, when a scientist, without the prior consent of the patients, injected them with HeLa cells to assess whether or not they developed cancer from these cells. It was not until 1965 that he was accused of unethical and unprofessional conduct..
The years after this case were very productive for medicine and histology. In 1955, Jonas Salks developed and put the polio vaccine into use; discovered that HeLas became infected and died with the polio virus, which helped him develop a vaccine.
In 1966, the first hybridization of human cells with those of another animal (mice) was carried out thanks to HeLa cells..
Currently there are known studies developed with HeLa cells that have allowed to expand knowledge in fields such as immunology, with several studies on parvovirus, human immunodeficiency virus, human papilloma and polio.
In genetics, they have been used to perform genome sequencing; They have also been used to understand the mechanisms of cell aging, by analyzing cell reproduction and the functioning of the telomerase enzyme, an enzyme involved in a shortening of telomeres after each cell division.
Additionally, HeLa cells have helped in the production of drugs for diseases such as Parkinson's disease, leukemia, among others..
Other uses
They are used by the cosmetic industry to ensure that products do not have unwanted side effects. Additionally, they are used in bioassays of tolerance and effects of toxic substances in humans..
HeLa cells also traveled to outer space during space missions in the 1970s. Scientists used HeLa cells to understand the effects of the absence of gravity on human cells.
Legal aspects
Most of the writings concerning HeLa cells agree on one general point. Obtaining these cells from the patient Henrietta Lacks was done without her consent and without knowledge of the use that these cells would have..
By the 50s of the last century, the consent of patients was not necessary to obtain tumor tissues. However, today, and thanks in part to the Lacks family, there are laws to protect the patient.
These laws regulate aspects such as the protection of medical information of patients, communication with donors of cells, tissues, and participation in trials or research..

In the United States, there are state and federal laws that control and regulate patient consent and the use and exchange of information from medical records..
Currently to use HeLa cells, or genetic information from these cells, it needs to be approved by a committee. In this committee participate, among others, relatives of Henrietta Lacks
References
- HeLa. Wikipedia. Recovered from en.wikipedia.
- Helas cells. EcuRed. Recovered from ecured.cu.
- C. Dosne Pasqualini (2006). HeLa cells as a prototype of immortalized cell culture. Medicine.
- HeLa cells (1951). British Society for Immunology. Recovered from immunology.org.
- Henrietta Lacks. Encyclopædia Britannica. Recovered from britannica.com.
- The Legacy of Henrietta Lacks. Johns Hopkins Medicine. Recovered from hopkinsmedicine.org.
- Phases of the cell cycle. Recovered from es.khanacademy.org.
- J.P. Álvarez (2013) Henrietta Lacks. the name behind hela cells, the first human immortal cell line. Los Condes Clinical Medical Journal.
- YE. Portillo (2014) .The eternal HeLa cells, today's ethical dilemma. Honduran Medical Journal.



Yet No Comments