
Nervous colitis symptoms, causes and treatments

The colitis nervosa, Irritable bowel syndrome or irritable bowel syndrome, is a functional intestinal disorder characterized by abdominal pain or discomfort and change in bowel or bowel habits, presenting constipation, diarrhea or alternating these symptoms.
Chronic diseases such as nervous colitis affect different aspects of the lives of the people who suffer from them. At first, a period of crisis begins where the patient accuses an imbalance at different levels: physical, social, psychological (with fear and anxiety) until finally he assumes that his problem is chronic.

All this necessarily implies adopting changes in life habits: physical, work and social activity.
Article index
- 1 Symptoms of nervous colitis
- 2 Causes of Nerve Colitis
- 3 Evaluation and Treatments for Nervous Colitis
- 4 Treatment
- 4.1 Cognitive-behavioral therapy
- 4.2 Relaxation techniques
- 5 References
Symptoms of nervous colitis
Patients with nerve colitis usually present with abdominal pain, which is localized in the lower abdomen and which can be colic, cramping or stabbing, with evacuation showing relief from the pain. However, this pain can also be present in other parts of the abdomen. In addition, another characteristic symptom is diarrhea or constipation..
These patients also show other gastrointestinal symptoms such as:
- Abdominal distension
- Gases
- Flatulence
- Feeling of incomplete evacuation
- Bowel movements with mucus
- Urgent evacuations
There are differences between men and women in some symptoms, not in abdominal pain but in the emission or not of rectal mucus, the sensation of incomplete evacuation, abdominal distention or the presence of goat feces, which are more frequent in women than in men..
Likewise, these patients present limitations at the physical, social, vitality and emotional role level. In addition, pain is one of the conditions that most affects their quality of life, since it reduces their daily functioning, in the social sphere and in the workplace..
The fact of perceiving a lower well-being and a poorer quality of life is necessarily associated with a lower satisfaction in their mental health, they have high levels of anxiety and depression and less control of their emotions.
In general, these patients show emotional alterations, concern for their health to a greater extent, a negative assessment of their physical condition and present more disease behaviors.
Causes of nerve colitis
It is a multifactorial problem, with no single or well-defined cause. So the approach applied is biopsychosocial given the number of factors that can affect its appearance and development..
Different triggers have been identified for the appearance of symptoms related to nervous colitis:
- Vital changes
- Labor disputes
- Financial or interpersonal difficulties
- Consumption of some foods
- Drug intake
- Psychoactive substance abuse
- Hormonal factors
- Psychological states: anxiety, panic, perfectionism, frustration, low self-esteem, depression, need for social approval, rigidity to comply with social norms.
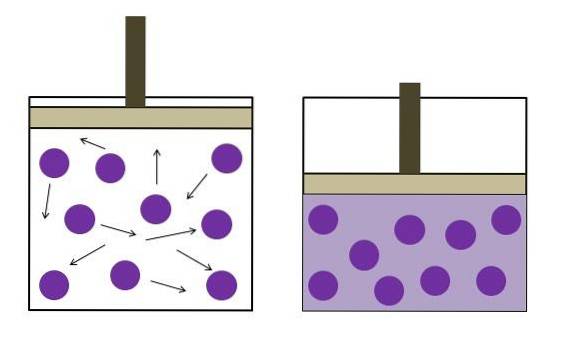
One explanation for this problem argues that it may be due to a failure in regulation between the central nervous system and the enteric nervous system. Some laboratory tests do not support this hypothesis.
The different theories in relation to this problem are divided into the following:
Motility disorders
They tend to present greater motility disorders than the general population, so that there are more problems in gastric activity, exaggerated motor responses to food, increased frequency in the migratory motor complex, etc..
Visceral hypersensitivity and the brain-gut axis
There are different studies that have shown that subjects with this pathology perceive pain abnormally when faced with visceral stimuli that are not painful for the normal population. This is what is called 'visceral hypersensitivity'.
They tend to have greater sensations of pain or evacuation of the rectum than normal people. And this perception is caused by the afferent fibers that carry information to the spinal cord and brain stem, and from these it is projected to the hypothalamus and amygdala..
Likewise, regulation takes place at the central level that is subjectively affected by emotional, cognitive and motivational factors..
An abnormality has also been found regarding the hypothalamic-pituitary-adrenal axis, such that there is a hyperresponsiveness of the visceral axis.
Inflammation of the intestinal wall
Some studies link this inflammation to nerve colitis. And in addition, the alteration of the intestinal flora can also be related to these symptoms.
Psychological factors
What weight is given to these factors is not clear; however, more than 2/3 of patients with this problem show psychological problems.
Although an attempt is made to clarify what the genetic factor may be within nervous colitis, greater factors of an environmental and family nature and not so much hereditary can be observed when developing it.
Likewise, it has been shown that the children of patients with this problem tend to visit the doctor to a greater extent, have higher rates of absenteeism in school and greater gastrointestinal and other symptoms than people who do not suffer from it.
Evaluation and Treatments for Nervous Colitis
Some alarm data must be taken into account, for which it must be attended in the evaluation of the problem, among which are:
- Be over 50 years old
- Abrupt onset of symptoms
- Weightloss
- Nocturnal symptoms
- Male gender
- Family history of colorectal cancer
- Anemia
- Rectal bleeding
- Recent use of antibiotics
Faced with these alarm symptoms, a subsequent clinical investigation is required and nervous colitis cannot be diagnosed until organic pathologies have been ruled out..
Treatment
The treatment should optimize the relationship between the patient and the professionals who work with him, reinforce the certainty of the diagnosis, treat the diet to exclude those foods that can precipitate the symptoms.
Lifestyle should also be addressed, to advise those changes that may be beneficial for him, drugs that act on the predominant symptoms such as abdominal pain, constipation and diarrhea (antidiarrheals, laxatives, spasmolytics, anti-inflammatories, antidepressants should also be administered , antibiotics, probiotics)
Likewise, psychotherapy is also included, even more so if we take into account that emotional factors can trigger symptoms. We highlight cognitive-behavioral therapy and relaxation techniques.
Cognitive behavioral therapy
It works through the behavioral patterns that lead the person to negative emotions, helping them to recognize these beliefs, analyze them and use more adaptive behaviors. It has been shown to be useful in reducing both symptoms and stress.
Relaxation techniques
For example progressive muscle relaxation or meditation (mindfulness). They have shown efficacy in some studies conducted. They should not be done in isolation but within other psychological treatments.
Today some experts question the idea that Nervous Colitis is a functional disorder, since they have shown that in this pathology there is low-grade inflammation of the mucosa (inflammatory cells).
References
- Balboa, A., Martínez, G. Brief epidemiological data on irritable bowel syndrome. Monographic Topic.
- Castañeda-Sepúlveda, R. (2010). Irritable bowel syndrome. University Medicine, 12 (46), 39-46.
- Geijo, F., Piñeiro, C., Calderón, R., Álvarez, A., Rodríguez, A. (2012). Irritable bowel syndrome. Medicine, 11 (6), 325-330.
- Lagunes Torres, F. S. (2005). Bibliographic review of Irritable Bowel Syndrome. Thesis of the Universidad Veracruzana, Faculty of Medicine.
- Sebastían Domingo, J. J. (2013). Irritable bowel syndrome, should it no longer be considered a functional disorder? Clinical medicine, 140 (9), 403-405.
- Vinaccia, Stefano (2005). "Quality of Life, Anxiety and Depression in Patients with a Diagnosis of Irritable Bowel Syndrome.". Psychological therapy, 23 (2), p. 65.


Yet No Comments