
When the mind makes the body sick Hypochondriacs

It seems that I am fine, but I always doubt that I have something wrong. (Hypochondriac patient)
The body is the memory of absolutely everything that has ever been lived. Miller alice
Contents
- Excessive concern for health
- Famous hypochondriacs
- Studies on attitude and health
- The health paradox
- The complexity of hypochondria
- Hypochondriasis or hypochondria and hypochondriacs
- Comorbidity complicates understanding of hypochondriasis
- Generally, someone who suffers from hypochondriasis also has other psychosocial conditions:
- Clinical symptoms observed in other sources:
- Clinical symptoms seen in people who are hypochondriacal and do NOT show up on DSM-IV:
- The DSM-V solution to hypochondriasis
- The neurophysiological origin of fears
- Three characteristics about the brain, considering that when used to the fullest you can feel tired
- Consequences of being a hypochondriac
- Treatment
- References
Excessive concern for health
- Roberto, he has so many medicines in his travel bag that it seems to be what a medical visitor or an itinerant pharmacy is. He knows all of them perfectly, the interesting thing is that he takes them in case any of his colleagues or acquaintances ever need them.
- Lupita, you've had a stomach ache for months that won't go away. You have visited at least three different specialists, they have carried out all the cabinet studies and all the specialists tell you that you have nothing, that you go home calmly and that worries you more.
- Victor, you have all the basic medical devices at home to take your vital signs. When you have a strong emotion, you feel like you are going to go into cardiac arrest, even several times you have ended up in the emergency room at the hospital and they tell you that you have a healthy heart as well as your normal blood pressure. Don't know what's up? and thinks the doctors are inept.
- Alejandra, is a Google doctor, every time she feels any symptoms of something, she looks for it on the net and her last search led her to the conclusion that she has a rare disease, just diagnosed on an island many thousands of kilometers from her home.
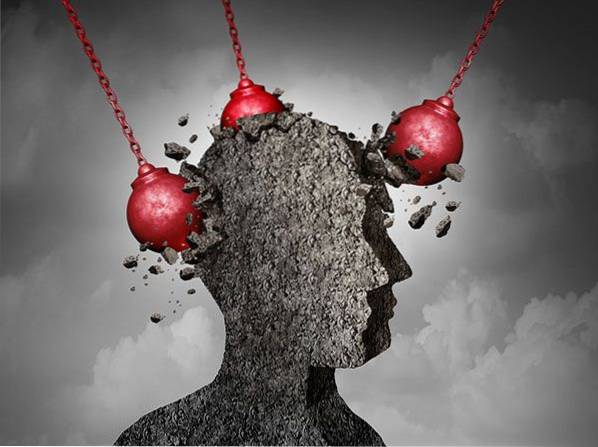
What do all these people share? They have a disorder where they have a negative attitude towards their own state of health being its mental origin and it is called: hypochondria. However, can the mind make the body sick? And if so, can this be considered a disease or is it someone with a very creative imagination?
An attitude is composed of affects, behaviors and cognitions (Fazio, cited in Morales, 1994), it can be positive or negative, it is presented towards someone or towards something and in this case, hypochondriacal people present it towards themselves, in particular towards his own state of health.
However, can having a negative attitude towards ourselves bring us any illness? Or even, is a person who constantly thinks they are sick taken in their right mind? As we will see later, negative thoughts themselves can make the body sick, especially when they constantly haunt our heads and that is the case of people who are hypochondriacs, because for the brain the imagined reality is the same as the reality experienced..
All of us have come to feel a little concerned about our health, but what happens when this becomes permanent? Interest in health is something natural but not when it becomes an obsession, in the paradox, people obsessed with health rarely have a healthy body, and this can happen to anyone.
Famous hypochondriacs
- Adolf Hitler (1889-1945), complained of stomach pains (constipation and gas), some heart disorders, insomnia and paranoia about food, he made at least 15 women try his food so as not to be poisoned.
- Andy Wharhol (Andrew Warhola; 1928-1987), spent his whole life thinking that he was sick, saying that his hair was falling out, that he had a disease that caused skin cancer, brain tumors and AIDS. He was afraid of death (Herre, 2016; Ramírez, 2015).
- Woody Allen (1935 -), says that he is an alarmist and not a hypochondriac, but because of a chapped lip he thinks he may have a brain tumor or even "mad cow disease".
- Charles Darwin (1809-1882), had stomach problems, headaches and hands, and constant concern about the size of his nose.
- Hans Christian Andersen (1805-1875), Hypochondriac and always afflicted by nightmares, every time he stayed in a hotel he carried a few meters of rope with him to escape through the window in case of fire. He felt eternal toothache and assumed that he would be in the middle of a terrible catastrophe (Ramírez, 2015; Herre, 2016; Norogaca, 2011).
A negative past experience creates a negative perception in the present and a negative attitude in the present and in the future. From there, no one escapes, not people like you or me, not famous people in history. Because before being famous they are and have been human beings.
Studies on attitude and health
Currently many studies show that our attitude affects our health, including life expectancy. A longitudinal study (30 years), with 447 subjects, from the Mayo Clinic (2002), concluded: that optimistic people were healthier physically and mentally. They experienced less pain, had more energy, enjoyed social activities more, and felt more content, calm, and collected most of the time. And optimistic subjects lived longer than pessimists. In another longitudinal study at Yale University, they followed 660 people aged 50 and over, and found that people who had a positive attitude about aging lived seven years longer than those who faced it with a negative attitude . Attitude had more influence on longevity than blood pressure, cholesterol levels, smoking, being overweight or the amount of physical exercise. Finally, another study carried out at Duke University with 866 patients with cardiovascular problems found that those who felt positive emotions daily were 20 percent more likely to be alive after eleven years than those who usually experienced negative emotions (Dispenza, 2014).
The health paradox
We are all concerned about our state of health, as part of our own survival. And, the perceptions that we have of her, could go; from living in total unconcern, going through intermediate scales, to living a lot, very worried.
A paradox is a saying or fact contrary to logic. Then then, for hypochondriacs, the more they worry about their health, the more they get sick. And, the more studies are carried out and no disease is revealed, the more they believe they have that one or another masked out there. A characteristic to come to consider a person, with this disorder, is that medical studies have been carried out of what they believe they suffer and in all of them the constant is "that they have nothing", medically speaking.
The complexity of hypochondria
Since the prehistoric era, we have not understood mental illness!!
In the beginning of the treatments there was no hope of a cure, and it was synonymous with being stigmatized and tortured.
The mentally ill were considered lunatics for having a different behavior, and it was due to the influence of the moon. It was also considered that other types of invisible forces controlled his life, such as demons, or even the influence of planets such as Mars, the planet associated with war..
At least the concept of stigmatizing a person with different behavior continues to this day and is associated with negative labels. So many times, people decide to isolate themselves from social interaction, or have as little contact if possible with others as happens with hypochondriacs.
Diagnosis is the process of identifying a disease by its signs and symptoms. In general, there are two different models that allow the diagnosis of any disease to be made, namely:
- Symptomatic: the disease is diagnosed based on the symptoms.
- Etiological: the diagnosis is made based on the cause of the disease.
Reaching an etiological diagnosis is only possible in those conditions in which the relationship between a cause and an effect is unequivocally established, as occurs with infectious or chromosomal diseases, to name two examples. In the case of mental disorders, only in some cases is it possible to establish this relationship. Thus, most of the diagnosis of mental disorders is made based on the symptoms that the patient presents, since it is accepted that the etiology of mental disorders is "biopsychosocial", so biological, psychological and social: genes and environment (Lara, cited in De la Fuente and Heinze, 2015).
Hypochondriasis is a disorder or disease where the symptoms have several constants: the fear of getting sick from one or some diseases, the constant thoughts related to them, emotional pain caused by their own thoughts and by the misunderstanding of those around them, They become specialists (theoretical, practical) in various diseases, experience symptoms that appear to occur only in their heads, they exacerbate their own symptoms, whether serious or not, many times they do not have credibility of suffering from any disease before doctors and family or friends around them, do not have supportive therapeutic strategies and do not have a clear explanation of what is happening to them.
Hypochondriasis or hypochondria and hypochondriacs
Specialized sources define "Hypochondriasis" as a somatoform disorder characterized by worry, fear or the belief that one has a serious physical illness, which is based on the incorrect and unrealistic interpretation of bodily symptoms. This fear or belief persists for at least six months and interferes with social or occupational functioning despite reassuring words from doctors that there is no physical disorder (APA, 2010).
A very important annotation that contradicts the definition of the APA, is that although it is said to be an incorrect and unrealistic interpretation, that does not matter to the brain of the person who suffers from it. For the person, if his interpretation is realistic or not, for his brain it is his reality.
Hypochondria is part of the so-called somatoform disorders, they include various conditions in which a psychological conflict results in physical problems or symptoms that cause disturbance or deterioration in the life of the person. In addition to presenting somatizations, people constantly live with maladaptive thoughts, feelings, behaviors and attitudes.
Other sources define hypochondria as an excessive and irrational fear and concern to suffer some disease, and the consequent obsession and assurance that it is so, at the slightest symptom or change in our body. Those who suffer from this disorder live permanently alert to any signal from their body that may make them suspect a disease and therefore, this leads to a truly exhausting state of anguish and restlessness (Ortega, 2017). According to the dictionary of the APA (2010), hypochondria is a morbid concern of the person for their state of health, includes unfounded beliefs of poor health.
A person with hypochondria or hypochondriasis is called a hypochondriac. People called hypochondriacs believe or fear that they have a serious illness, when in reality they are only experiencing normal bodily reactions (Halgin & Krauss, 2004).
However, this condition can become a little more serious, as this disorder is also associated with other disorders. A person can get sick from different conditions, this is called comorbidity.
Comorbidity complicates understanding of hypochondriasis
Among mental patients, the concept of comorbidity has been applied to several notions,
- the first: it refers to other diseases, psychiatric symptoms that are associated with the initial illness,
- the second meaning: -by the way, less used refers to systemic problems, which are associated or added to the original psychiatric problem,
- Perhaps it is worth mentioning a third possibility: that which refers to the mental symptoms or syndromes with which a systemic condition manifests itself, which sometimes happens even as the first manifestation of the disease (Ramiro; cited in De la Fuente and Heinze, 2015).
It is interesting to observe these approaches with respect to the comorbidity of hypochondriasis, because at the base of this disorder, there are different symptoms reported by the patients: they include different types of fears that can lead to phobias, anxiety, anguish and even depression. In addition to feeling physical and social pain through rejection in their daily interactions.

And, the signs that medical personnel can capture are almost always very few, since generally the studies that are carried out on the patient do not correspond to their severity. In addition to having other diseases: heart, gastrointestinal and respiratory, for example.
This condition leads us to another paradox: the patient reports symptoms of serious alterations and the specialist cannot corroborate them with his studies at the same level of severity. So who should we believe?.
And, more questions arise: Does the patient lie and have a social or personal benefit with it? Are the instruments currently available in science not reaching the level of precision to detect what the patient reports as serious? Are we looking in the wrong places, as specialists? Or do we still not understand mental illnesses, despite the advances in technology, neurosciences and the theoretical approaches that we have until today??
Generally, someone who suffers from hypochondriasis also has other psychosocial conditions:
- We are emotional, hormonal and contextual beings, rather than rational. Fear is one of the most primitive emotions that alerts us to danger and allows us to survive. A person with fear has the brain amygdala working all the time and all his contextual reality interprets it in an exaggerated way. When a person suffers an emotional abduction, they totally lose control of their rational acts, it is useless as a strategy that they give you advice at that moment or ask you to calm down.
If the fears are real or imaginary, the brain experiences them as the same reality and in the case of hypochondriacs they appear in that context (real and / or imaginary). Although in a generic way we all face different types of fears, in the comorbidity of hypochondriacs they are a mixture of them:
- Fear of death thanatophobia: possibly one of the greatest fears we have as human beings.
- Fear of getting sick or nosophobia: it is normal to feel discomfort due to having some symptoms when being sick, but this becomes a constant, centralistic and catastrophic concern in this case,
- Fear of pain algofobia: pain is part of the signals that the body sends us to inform us that something is not right, but when it becomes a constant worry, it loses its ability to alert us to a disease,
- Fear of dependence or soteriophobia: as people we are social beings, living in isolation would be against nature, but living completely attached to someone does not allow us to live a healthy life, if there is someone to accompany us, here it is a condition where the person can fend for herself, but can't do it,
- Anxiety Disorders: Specific phobias (of blood or wounds, using public toilets, needles or injections, dentists or hospitals and certain diseases) and also obsessive compulsive disorder,
- Mood Disorders: depression, accompanied by low self-esteem.
In summary, they present obsessive thinking related to their physical and mental health, where different types of fears that activate the brain amygdala and the impossibility of the prefrontal cortex take control and calm the situation are mixed in their comorbidity. In addition to distrusting doctors, medicines, their measuring instruments and medicines.
The perception of the patient's state of health can be further aggravated when some other medical illness also enters the clinical picture.
Clinical symptoms observed in other sources:
- Have this condition for at least 6 months.
- Traumatic events in childhood Sexual abuse or exposure to events related to death.
- High sensitivity in body stimuli (Halguin & Krauss, 2004).
Clinical symptoms seen in people who are hypochondriacal and do NOT show up on DSM-IV:
- Get tested constantly.
- Bring medication for personal use or in case it is required in a supposed emergency.
- Believing that you have the symptoms of a disease when you hear it, see it, and receive the information from some sensory stimulus (seen, hearing, touch, taste, or smell).
- Being afraid or worried about a serious or life-threatening illness.
- Interpreting one's own symptom or sign with a negative attitude, as if it were a specialist doctor.
- Be an expert in the diagnosis of various diseases, rather than a doctor, based on your own research or experience.
- It is a person who is constantly informed or documented about diseases and regularly visits doctors to tell them the diagnosis he has.
- He presents negative thoughts, feelings and beliefs about his state of health, this attitude is centralistic (the subject of his illness or some disease) and catastrophic (always with a fatal outcome).
- They get upset if doctors contradict them in their diagnoses or assessments of their health.
- You can really get sick, but in general your conditions are imaginary or psychosomatic. However, thought creates reality, that is, if your brain believes that they are sick, they are actually sick..
- Their disease condition is mediated by a "nocevo" thought, and that consistent and constant thought causes the disease, even if they have nothing..
- The presence of a single self-perceived symptom can trigger an entire clinical picture in its own interpretation.
- Your vital signs are constantly checked.
- They feel rejected and misunderstood by others.
- There are those who avoid going to a professional for fear of actually discovering a disease.
- They are people who think they know more than doctors.
The DSM-V solution to hypochondriasis
A very elegant and absurd solution, we can find it in the latest edition of the DSM-V, they simply eliminated the disorder and in my point of view without understanding it as you can read right away.
Hypochondriasis has been eliminated as a disorder, in the new version of DSM-V published in May 2013, in part because the name is perceived as pejorative and also is not conducive to an effective therapeutic relationship (Lara; cited in De la source and Heinze, 2015).
The neurophysiological origin of fears
However, this radical measure does not eliminate the condition of a patient experiencing a mixture of fears and an over-excitement of the brain amygdala. I think the experts who made this decision need to investigate more about the context of the patients and many other things such as the expectations of a behavior (the good or the bad thing that I think: the brain makes it a reality). For example, the expectation of happiness generates happiness and the expectation of fear generates fear and various reactions (physiological, psychological, behavioral and social) among these discomforts is anticipated anxiety. Then then, if we have anticipated anxiety due to fear of something or someone, we could lose control, as happens with phobias, which are irrational fears and experienced by people with hypochondriasis. It is not about labeling a patient, but about knowing how a disorder operates.
One more example of a non-hypochondriac brain, but with negative decrees in its head, we find in people who have received chemotherapies. According to the National Cancer Institute, about 29 percent of patients who undergo chemotherapy when exposed to smells and images that remind them of chemo treatments suffer from a disorder called anticipatory nausea (Dispenza, 2016). And, this brings us to other more intricate and interesting terrain, but it can also spell a light at the end of the road for disorders like hypochondriasis. For the brain, in the sensory imprint it can activate the fear reactions just by imagining the stressful situation, which produced anxiety and fear up to the point of phobia.
If we neutralize this imprint, necessarily the brain amygdala will have to be less active and the negative attitude towards the patient's health could change.
Any activity, thought, feeling, action or imagination is mediated by the brain. You need 20% of everything we consume.
There is evidence that the prefrontal cortex can regulate the behavior of the amygdala and all our behaviors (planning, reason, cognition, decision-making, memory) are mediated by emotions (Redes, 2014).
Scientists have discovered that as humans evolved, another part of the brain called the cerebral cortex became involved in the fear process. The part of the brain that makes us most human is the cortex. If the amygdala is the first floor, the cortex is the second floor of the brain, it is the thin and rough outer layer that is divided into four groups of lobes. The frontal lobes correspond to the area that is just above our eyes and are the newest rooms of the brain, as humans evolved the frontal lobes became the place where conscious rational thoughts are processed, it is where we solve our problems. The frontal lobes are very interesting because they are the conductor of the brain, they synchronize all the activity. Scientists took a big step in the investigation of fear, when they discovered that information from our senses circulates to the amygdala, almost twice as fast as it does to the frontal lobes, the difference in speed between brain signals assumes that unless we know Reacting instinctively to a potential threat, we will be paralyzed with fear, while we wait for the frontal lobes to come up with the appropriate response. When fear and panic appear, we do not know! to do?. The brain is frozen, like a deer with the headlights of a car. The amygdala receives the signals of fear very quickly, but sometimes it is wrong. The situation can tell you right away, it is not a scary situation, there is no danger, these fast signals from the amygdala can be controlled gradually (Discovery, 2017).
Three characteristics about the brain, considering that when used to the fullest you can feel tired
- 1) Your brain feels the pain of others as if it were its own. Feel the same pain when something happens to you or a loved one. The same neurons fire when you feel hopeless, and the same happens when someone you care about feels bad.
- 2) For your brain the things you imagine are real, the same nerve endings are activated in your brain regardless of what you are experiencing; it is real or imaginary. If you dream that you have a spider on your leg, you will feel the same fear as if it really happened.
- 3) The brain cannot distinguish between physical and emotional pain. The pain of a broken heart hurts just like a thorn in your finger. It doesn't matter if your heart is broken or if you break a bone, they both hurt the same. (Dr. Sood, 2016).
Consequences of being a hypochondriac
The family being a system is affected by having one or more members with this condition.
The hypochondriac can be mistreated by the doctor and the people around him, obviously including the family.
Treatment
In paradox, controlled exposure to fear weakens the neural networks of the amygdala, as occurs with systematic desensitization therapy..
Starting with the treatment of successive approximations. The objective is to make the brain amygdala, leave the automatic control of potential dangerous situations and take it the prefrontal cortex, the site from which the brightest thoughts come and from where the internal negotiation of lowering the intensity of emotions is exercised..
When you get used to facing fear in this controlled therapy, you have a better training of the prefrontal cortex, so that it knows how to react in the everyday world when they appear and only the patient is found.
The US Army, to train its special forces and overcome extreme fear, carries out self-therapy based on four points:
- Set your goals,
- Mental rehearsal,
- Self-talk or self-motivation and
- Excitation control (Discovery, 2017).
One more proposal, non-drug, is the use of technological psychotherapy, through the use of technology called: pulsed low-frequency electromagnetic field. The electromagnetic field bed is used, as if it were the old therapy couch. The electromagnetic field through electromagnetic pulsations, balances the electrical charges of the over-activated brain amygdala, thereby achieving a state of relaxation for the patient that helps to achieve changes at the cognitive level. Thus, a better negotiation with the prefrontal cortex is established to achieve self-control of the patient's attitude.
The objective is for the patient to achieve a positive attitude towards their state of health, towards the environment that surrounds them and towards life itself.
References
APA (2010) APA Concise Dictionary of Psychology, Editorial el Manual Moderno, Mexico.
De la Fuente J. R. & Heinze G. (2015) Mental health and psychological medicine, Mc Graw Hil and National Autonomous University of Mexico, Mexico.
Dispenza J. (2016) The placebo is you, Ediciones Urano, Mexico.
Halguin R. & Krauss S. (2004) Psychology of abnormality (Clinical Perspectives on psychological disorders), Mc Graw Hill, Mexico.
Morales, J.F. (1994). Attitudes. In J.F. Morales, Social Psychology (pages 495-621). Madrid: Mcgraw-Hill.



Yet No Comments