
Heinz bodies characteristics, formation, coloration, pathologies
The Heinz bodies They are granulations or pathological inclusions that appear on the periphery of red blood cells or erythrocytes. They are formed by the denaturation of hemoglobin under certain abnormal conditions. Denatured hemoglobin precipitates and accumulates on the erythrocyte membrane.
Hemoglobin precipitation can have several causes, however the main one is due to a deficiency or dysfunction of the enzyme glucose - 6-phosphate dehydrogenase. This enzyme is essential in the derivation pathway of hexose-monophosphate.
This pathway is necessary for the maintenance of the erythrocyte, specifically it is responsible for producing reduced NAPH molecules. This in turn acts by reducing glutathione, a necessary condition to protect hemoglobin from the action of peroxides (oxidative stress)..
Enzyme deficiency can be due to genetic defects or mutations. There are many anomalous variants, among them are the Mediterranean, Asian and African. Other causes include unstable hemoglobinopathies and drug-induced hemolytic anemias..
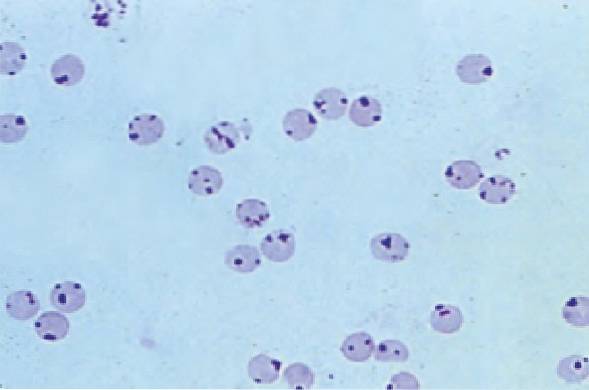
Heinz bodies are visible when special stains are used, since the usual stains of blood smears do not stain them.
With special staining, Heinz bodies appear purple or violet and measure 1 to 2 microns. The most widely used basic dye is bright cresyl blue, but cresyl violet can also be used..
Article index
- 1 Features
- 2 Why are Heinz bodies formed??
- 2.1 ATP
- 2.2 NAPH
- 2.3 GSH
- 2.4 2,3-DPG
- 2.5 Power generation routes
- 3 Staining of Heinz bodies
- 3.1 Technique
- 4 Pathologies in which Heinz bodies are observed
- 4.1 -Deficiency of glucose -6-phosphate-dehydrogenase
- 4.2 -Unstable hemoglobinopathies
- 4.3 -Hemolytic anemia due to drug
- 4.4 -Talasemias
- 5 Disposal of Heinz bodies
- 6 References
Characteristics
Heinz bodies are seen as tiny purple round inclusions located toward the periphery of the red cell membrane. These are usually stiff. They usually appear in both young and mature erythrocytes.
There may be one to several Heinz bodies within the same red blood cell..
Excentrocytes can also be seen in smears from patients with glucose-6-phosphate dehydrogenase deficiency. Excentrocytes are erythrocytes that have an abnormally eccentric paleness, that is, it is not central. These cells are known as bitten cells..
Why are Heinz bodies formed?
To understand why Heinz bodies are formed, it is necessary to explain that the erythrocyte is a cell that does not have a nucleus and neither do certain organelles such as mitochondria; for this reason they are unable to synthesize protein and lipids. They are also unable to use oxidative metabolism.
However, the erythrocyte for its survival only needs to generate 4 fundamental elements, which are: adenosine triphosphate (ATP), reduced nicotinamide dinocleotide (NAPH), reduced glutathione (GSH) and 2,3-diphosphoglycerate (2,3-DPG).
ATP
The red blood cell uses ATP to maintain the lipids of its membrane and thus preserve its flexibility, in addition to maintaining the proper functioning of the transmembrane proton pumps, thus regulating the flux of sodium and potassium.
NAPH
NAPH is used to reduce iron from hemoglobin and reduce glutathione.
GSH
For its part, GSH is crucial for the protection of hemoglobin, since it prevents its denaturation by the oxidative action of peroxides.
2,3-DPG
Finally, 2,3-DPG is important so that hemoglobin can release oxygen in the various tissues. As well as it is responsible for maintaining the physiological deformity of the erythrocyte, which is vital for the red blood cell to pass through the smallest vessels.
Power generation routes
All of these molecules are formed through various metabolic pathways of energy generation. These are: the Embden-Meyerhof glycolytic pathway, the Luebering-Rapaport pathway, and the hexose-monophosphate shunt pathway..
The first route generates 75% of the energy that the erythrocyte needs. In it ATP molecules are produced. A failure in this pathway would generate short-lived red blood cells or early death (hemolytic syndrome).
The second route is to accumulate 2.3 DPG in the red cells; this is necessary to increase the affinity of hemoglobin for oxygen.
In the third, the necessary NAPH is generated to produce a sufficient amount of GSH, this in turn is essential to keep hemoglobin in good condition. A deficiency in this pathway leads to denaturation of hemoglobin. Once denatured, it precipitates and forms the Heinz bodies.
The main failure in this pathway is due to the deficiency of the enzyme glucose-6-phosphate-dehydrogenase (G6PD).
Heinz body coloring
Two types of dyes can be used to show Heinz bodies: bright cresyl blue and cresyl violet..
Prepare a 0.5% dye solution with saline and filter. Any of the aforementioned.
Technique
In a test tube place a drop of blood with anticoagulant. Then add 4 drops of food coloring and mix.
-Incubate at room temperature for approximately 10 minutes..
-With the mixture, you can make fresh spreads or suspensions. Observe under a microscope and count red blood cells that have Heinz bodies. To report the percentage of erythrocytes with Heinz bodies, 1000 red blood cells are observed and the following formula is applied.
% of GR with Heinz bodies = (number of GR with Heinz bodies / 1000) X 100
Pathologies in which Heinz bodies are observed
-Glucose -6-phosphate dehydrogenase deficiency
It is a congenital enzyme disease with acute hemolysis. It affects more than 400 million people in the world. In Spain only around 0.1 - 1.5% of the population can be affected. It is an inherited disease linked to the X chromosome.
The enzyme can be produced abnormally. There are anomalous variants such as Mediterranean, Asian and African.
If the enzyme does not perform its normal function, NAPHs are not produced. Without NAPH, glutathione molecules cannot be reduced and therefore the erythrocyte is not able to protect hemoglobin from oxidative stress..
In this scenario, hemoglobin remains unprotected and denatures in the presence of oxidizing agents, then precipitates and accumulates in the form of conglomerates at the membrane level. This causes rigidity in the cell and causes lysis of the red blood cell..
Some conditions can stimulate hemolytic anemia, such as exposure to oxidizing agents, suffering from certain infections, or eating fresh beans (fabismus).
Symptoms
In general, this congenital disease manifests itself by seizures that are self-limited. Symptoms when intravascular hemolytic crisis occurs are: abdominal or lumbar pain, general malaise, dark urine. The crisis can appear after suffering an infection, by ingesting fava beans or by taking medications.
-Unstable hemoglobinopathies
Some hemoglobinopathies can present with the appearance of Heinz bodies in the membrane of erythrocytes. This may be due to the presence of unstable hemoglobins that are easily denatured..
For example, in hemoglobin H disease, hypochromic microcytic anemia occurs with the presence of Heinz bodies..
-Drug-related hemolytic anemias
In patients with a deficiency of the enzyme glucose-6-phosphate dehydrogenase, hemolytic crises can occur with the consumption of certain medications, such as:
-Antiparasitics: Antimalarials
-Antibiotics: nalidixic acid, sulfonamides, nitrofurantoin, chloramphenicol, sulfones, among others.
-Thalassemias
Hereditary disease that causes anemia due to an abnormality in the synthesis of one or more of the hemoglobin chains. For example, alpha-thalassemia and beta-thalassemias.
In both conditions there is an excess of one of the chains. These tend to precipitate and form Heinz bodies, which accelerates the elimination of this red blood cell..
Elimination of Heinz bodies
Macrophages in the spleen have a function called ginning or pitting, which is responsible for eliminating Heinz bodies from erythrocytes, as well as other types of inclusions.
References
- Manual of special hematology techniques. Autonomous University of Yucatan. 2012.Available at: cir.uady.mx/sg.
- Sánchez P, Sánchez A, Moraleda JM (2017). Hematology Undergraduate. 4th Edition. Virgen de la Arrixaca University Clinical Hospital. Murcia. Professor of Medicine. University of Murcia.
- Malcorra J. Hemoglobinopathies and Thalassemias. BSCP Can Ped 2001; 25 (2): 265-277. Available at: scptfe.com portal
- Grinspan S. The study of the peripheral blood smear. Medical Rev Hondur, 1985; 53: 282-290. Available at: bvs.hn/RMH/pdf
- Erramouspe B, Eandi J. Conventional techniques applied to the diagnosis of hemoglobinopathies. Acta bioquím. clin. latinoam. 2017; 51 (3): 325-332. Available at: scielo.org.



Yet No Comments