
Hyaline degeneration types, diagnosis and treatment
To understand the concept of hyaline degeneration we must first know what the ground substance is. The extracellular matrix or fundamental substance is the basic element from which a certain type of organ or tissue is generated. Despite its lack of "life" of its own, it is affected by everything that alters the cell itself.
This fundamental substance provides the ideal environment for the cell for its normal functioning. Some researchers believe that this matrix comes from the same cell, which prepares the surrounding environment in the best possible way, not only to work better but to favor its multiplication and development..
The extracellular matrix can also be altered. There are several diseases that affect the fundamental substance, which are also considered cellular pathologies.
Among the best known of these conditions are amyloidosis, fibrinoid degeneration, myxoid degeneration, and the current topic, hyaline degeneration.
Article index
- 1 Definition
- 2 Kinds
- 2.1 Hyaline degeneration of connective tissue
- 2.2 Hyaline vascular degeneration
- 3 Diagnosis
- 4 Treatment
- 5 References
Definition
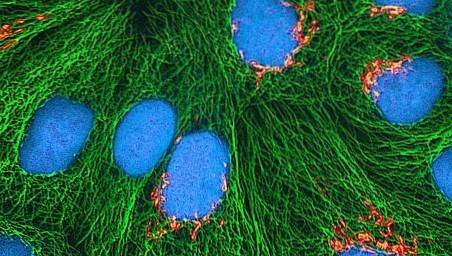
The hyaline portion of the ground substance represents its continent. Its name comes from the Latin Hyalus which means glass, due to the vitreous and homogeneous appearance that the surroundings of the cell have. The composition of the hyaline substance is basically water and proteins, although it has small amounts of ions and glycans.
Conceptually, hyaline degeneration is damage to the extracellular hyaline substance. The structures most affected by this phenomenon are reticular fibers, collagen fibers and basement membranes. These are distributed throughout the body, so hyaline degeneration can alter any organ or tissue.
Not all hyaline degeneration processes are considered pathological. Atresia of the ovarian follicles and the corpus luteum, which occur when the ovum is not fertilized, are considered normal and necessary events in female sexual physiology. Something similar occurs with the degradation of scar tissue and certain inflammations.
Types
Hyaline degeneration exists in multiple tissues, but it is classified into two broad categories, namely:
Hyaline degeneration of connective tissue
It is the most common and studied. It occurs after inflammatory processes that affect the serosae, during the stage in which fibrin is organized.
It is common in autoimmune and rheumatological diseases and after trauma or injury. This type is also the one that characterizes the aforementioned normal involution of the corpus luteum..
The best-known examples of hyaline degeneration of connective tissue at the visceral level are lesions in the serosa of the spleen and in the pleura around the lungs asbestos.
On these surfaces, smooth, whitish, homogeneous, very thin but firm plates are formed. In the medical literature it is described as porcelain pleura or caramel spleen.
When hyaline degeneration affects collagen fibers, cartilage is damaged and cartilage ossification occurs. This phenomenon occurs frequently in the menisci of the knees and is a common reason for consultation in traumatology. Basement membrane damage affects the kidneys, testicles, and bronchi.
Hyaline lattice degeneration can affect the eye. Although it is a rare pathological entity, Salzmann's Degeneration, also known as climatic droplet keratopathy or spheroidal degeneration of the cornea, seems to have its origin in the hyaline degeneration of the corneal fibers, causing opacity and visual disturbances..
Vascular hyaline degeneration
Hyaline degeneration of the arteries and arterioles has been a known condition for more than a century. It is necessary to remember that these blood vessels that carry oxygenated blood have an important muscular wall. In the intima, one of the layers of the vascular wall, and between the muscle fibers, remains of plasma proteins are deposited.
The precipitation of protein debris at these levels causes thickening of the vascular wall and atrophy of muscle fibers. Observed under the microscope, these vessels show a characteristic thickening ring with a very narrow luminal diameter and absence of nuclei in their cells..
Hyaline vascular degeneration is common in the elderly, diabetics, and nephropaths, especially those with severe and difficult-to-manage hypertension.
In fact, some authors affirm that hyaline vascular degeneration is one of the many causes of microangiopathy and nephropathy typical of diabetes.
Diagnosis
Arriving at the diagnosis of any alteration of the fundamental substance, especially of hyaline degeneration, is not easy at all.
In fact, it is a rule-of-thumb diagnosis. It is often confused with storage diseases such as sarcoidosis and amyloidosis itself, or with rheumatoid arthritis, lupus, infections and even cancer.
When in doubt, the definitive diagnosis will be given by histological studies. The fundamental difference lies in the coloration of the tissue and the damaged areas. Degenerated hyaline tissue will always stain eosinophilic with Hematoxylin-Eosin or red if Van Gieson is used.

The evaluation of the tissue shows some indemnity of the cell but with surrounding lesions. This does not mean that the observed cell does not present damage, but that it is predominantly located on the periphery of it. In hyaline degeneration, there will always be the presence of homogeneous extracellular bands or plaques of protein content.
Ttreatment
Hyaline degeneration is a pathophysiological condition that can alter multiple organs and tissues. Depending on the affected system and the symptoms, the corresponding diagnostic and therapeutic strategies will be decided. But hyaline degeneration does not have its own or specific treatment. The management will be decided according to the clinic.
Joint and eye damage can be resolved with surgery. As the knees are the most affected by the degeneration of collagen fibers, arthroscopies are frequently performed. Eye surgery to remove the opacity is quick and easy. In both cases there is a high risk of recurrence.
The caramel spleen is very fragile and can break on contact. Splenectomy is of choice if there is a risk of splenic eruption. The pleura of asbestosis may require surgery as well, although medical steroid treatment is preferred initially. In genital pathology, male or female, surgery is the choice.
Renal failure mediated by hyaline vascular degeneration, especially in diabetics, is irreversible. These types of patients are managed with antihypertensive and diuretic drugs at first, but usually end up in hemodialysis or kidney transplantation..
References
- Catholic University of Chile (s. F.). Extracellular Matrix Alterations. General Pathology Manual, Retrieved from: publicationsmedicina.uc.cl
- Acuña, Ezequiel and Peña, Claudio (2011). General Pathology, Extracellular Degenerations. Recovered from: ezzesblack.wordpress.com
- Codesido, Pablo (2016). Degenerative meniscus and internal knee overload. Recovered from: drpablocodesido.com
- Frising, M. et al. (2003). Is hyaline degeneration of the cornea a precursor of Salzmann's corneal degeneration? British Journal of Ophthalmology, 87 (7): 922-923.
- Murase, Eiko et al. (1999). Uterine Leiomyomas: Histopathologic Features, MR Imaging Findings, Differential Diagnosis, and Treatment. Radiographics, 19 (5).
- Bryant, S. J. (1967). Hyaline droplet formation in the renal epithelium of patients with haemoglobinuria. Journal of Clinical Pathology, 20 (6): 854-856.



Yet No Comments