
Vascular dementia symptoms, causes, types and treatments
The vascular dementia (DV) It can be defined as an alteration of memory that occurs accompanied by a dysfunction in one or more of the following cognitive areas: language, praxis, executive function, orientation, etc. It is severe enough to affect the patient's daily activities.
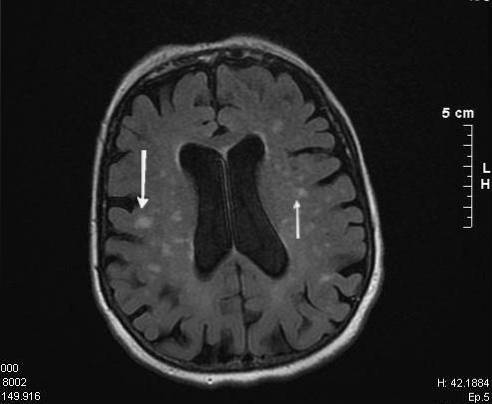
This type of disorder appears as a consequence of brain damage due to multiple vascular accidents or focal lesions in the blood vessels that supply blood to the brain (National Institute of Neurological Disorders and Stroke, 2015).
Vascular dementia is the second leading cause of dementia in Western countries, after Alzheimer's disease. In addition, it constitutes a potentially preventable type of dementia (Álvarez-Daúco et al., 2005).
Normally, vascular dementia and vascular cognitive impairment arise as a result of different risk factors both for this pathology and for the suffering of cerebrovascular accidents; These include joint fibrillation, hypertension, diabetes, high cholesterol and / or amyloid angiopathy, among others (National Institute of Neurological Disorders and Stroke, 2015).
Article index
- 1 Statistics of vascular dementia
- 2 Definition and concept
- 3 Clinical characteristics
- 4 Types of vascular dementia
- 4.1 Mixed dementia
- 5 Diagnosis
- 5.1 Characteristics for the diagnosis of probable DV
- 5.2 Clinical characteristics consistent with the diagnosis of DV
- 5.3 Characteristics that make the diagnosis of DV uncertain
- 6 Causes and risk factors
- 7 Treatment
- 8 References
Vascular dementia statistics
After Alzheimer's disease (AD), vascular dementia is the second leading cause of dementia.
Different statistical studies have shown that the incidence of vascular dementia (VD) in Europe was approximately 16/1000 at 65 years and 54/1000 at 90 years, constituting around 20% of the total of all cases of dementia (Bernal and Roman, 2011).
In the United States, it is estimated that approximately 4 million people have dementia symptoms and it has been predicted that this figure may reach 16 million people due to population aging, within which between 20-25% of cases (approximately 3, 5 million people) will have dementia of vascular origin (Bernal and Roman, 2011).
The age of onset of this disorder is between 50-59 years in approximately 45% of cases, while 39% are between 60 and 69 years of age (Ramos-Estébanez et al., 2000).
This fact is mainly due to the increase in the prevalence in these age ranges of two or more chronic diseases such as hypertension, diabetes, heart disease or osteoarthritis (Formiga et al., 2008).
Regarding gender, vascular dementia is more common in men, unlike Alzheimer's dementia, which is more common in women (Bernal and Roman, 2011).
Although most cases of vascular dementia are usually pure, around 12% of cases present a component of Alzheimer's disease to a greater or lesser extent, increasing the prevalence of vascular dementia by around 35-40% (Bernal and Roman , 2011).
Definition and concept
The exponential growth in life expectancy in recent decades has led to an increase in diseases related to aging. Currently, dementia is a major health problem in developed countries, since its incidence does not stop increasing (Bernal and Roman, 2011).
Under the term vascular dementia (VD), a not very homogeneous group of disorders have been classically included in which vascular factors play an important role in the subsequent development of cognitive impairment (CD) (Álvarez-Daúco et al., 2005).
In the scientific literature referring to the area of vascular dementia, we can find a multitude of terms associated with this clinical entity, some of them being erroneously used as synonyms; among them we can find: multi-infarct dementia, arteriosclerotic dementia, dementia due to leukoaraiosis, Binswaswagner's disease, vascular cognitive impairment, etc. (Bernal and Roman, 2011).
Vascular dementia is defined as that which is a consequence of cerebral vascular lesions, hemorrhagic, ischemic or hypo / hyperperfusion (Bernal and Roman, 2011).
The different etiological conditions will cause different cerebral vascular cerebral lesions that will vary in number, extension and location affecting both cortical and subcortical regions, especially cholinergic (Bernal and Roman, 2011).
Vascular lesions can damage corticosubcortical structures or can be restricted to the white matter and basal ganglia, causing damage to specific circuits or interrupting connections between networks that can be essential to support different cognitive and / or behavioral functions (Bernal and Roman, 2011).
Clinical features
The symptoms and signs of this pathology, together with the clinical course, can be highly variable from one patient to another, depending on the cause of the lesions and especially on the location of these (Jodar Vicente, 2013).
In most cases, the onset of vascular dementia usually presents a sudden and abrupt onset that follows a staggered course. Many family members observe periods of stabilization, followed by “outbreaks” or more pronounced cognitive losses (Jodar Vicente, 2013).
Normally, the most common complaint from family members and even the patient himself is “feeling that they are not the same”. It can refer to apathy, depression, apathy, isolation and social inhibition or changes in personality (Bernal and Roman, 2011).
In addition, it is possible to observe focal neurological alterations that will affect sensitivity and motor skills. A gait deficit, inability to carry out basic activities of daily life (bathing, using the telephone, dressing, going to the bathroom, eating, etc.), clumsiness in the production of language, etc. may appear. In addition, it is also possible to observe incontinence or urinary urgency.
The patients will also present alterations in the cognitive sphere. They may present a decreased level of attention, slower processing speed, deficit in the ability to plan and execute actions and activities, confusion, disorientation, as well as a significant alteration of immediate memory..
Types of vascular dementia
There is wide heterogeneity in the classification of types of vascular dementia. However, the review of the body of knowledge about vascular dementias allows us to differentiate several types:
Cortical vascular dementia or multi-infarct
It occurs as a consequence of multiple focal lesions in the cortical blood vessels. It is usually caused by the presence of emboli, thrombi, cerebral hypoperfusion, or strokes.
In most cases, it is possible that multiple infarcts are restricted to one cerebral hemisphere, therefore the deficits will be associated with the predominant cognitive functions in this (National Institute of Neurological Disorders and Stroke, 2015).
Subchorical vascular dementia or Binswanger's disease
It occurs as a consequence of injuries to the blood vessels and nerve fibers that make up the white matter. The symptoms that occur are related to an alteration of the subcortical circuits involved in short-term memory, organization, mood, attention, decision-making, or behavior (National Institute of Neurological Disorders and Stroke, 2015).
Mixed dementia
Different clinical studies, generally post-mortem, have shown cases in which there is a parallel occurrence of both vascular etiologies and those related to Alzheimer's disease (National Institute of Neurological Disorders and Stroke, 2015).
Diagnosis
The presence of vascular dementia is determined by the presence of vascular lesions. In addition, you must meet the criterion of having no other explainable cause.
In this way, the Neuroepidemiology Branch of the National Institute of Neurological Disorders and Stroke and the Association Internationale pour la Recherche et I'Enseignement en Neurosciences propose that the diagnosis of vascular dementia should be supported under different criteria (Bernal and Roman, 2011):
Features for the diagnosis of probable DV
- Dementia.
- Cerebrovascular disease.
- Abrupt or progressive fluctuating decline in cognitive functions.
Clinical characteristics consistent with the diagnosis of DV
- Early presence of memory disturbances.
- History of postural instability frequent falls.
- Early presence of urinary urgency or polyuria not explained by urological injury.
- Pseudobulbar palsy.
- Behavioral and personality changes.
Characteristics that make the diagnosis of DV uncertain
- Early onset of memory disturbances and progressive worsening of this and other cognitive functions in the absence of concordant focal lesions on neuroimaging.
- Absence of focal neurological signs other than cognitive alterations.
- Absence of cerebrovascular disease on brain CT or MRI.
Causes and risk factors
The fundamental cause of vascular dementia is strokes. With the term cerebrovascular accident (CVD) we refer to any alteration that occurs temporarily or permanently, in one or several areas of our brain as a consequence of a disorder in the cerebral blood supply (Martínez-Vila et al., 2011 ).
In addition, a cerebrovascular accident may occur as a consequence of both ischemic processes (refers to the interruption of the blood supply to the brain as a consequence of a blockage of a blood vessel) and hemorrhagic processes (when the blood accesses the intra or extra tissue cerebral).
Regarding risk factors, the suffering of vascular dementia is associated with all the factors concomitant with cerebrovascular accidents. Thus, already in the first studies on VD, a marked influence of hypertension, heart failure, atrial fibrillation, diabetes, smoking, sedentary lifestyle, alcoholism, sleep apnea-hypopnea syndromes, hypercholesterolemia, age, low socioeconomic level was observed, etc. (Bernal and Roman, 2011).
On the other hand, it is also possible that people who are subjected to high magnitude surgeries (cardiac, carotid surgeries, hip replacements), with states of cerebral hypoperfusion, chronic hypoxemia, exposure to pollutants or chronic infections, autoimmune diseases and vasculitis , they are patients with a high risk of presenting vascular dementia due to cumulative vascular damage (Bernal and Roman, 2011).
Treatment
There is currently no specific treatment that will reverse the damage caused by a stroke. Treatment typically tries to focus on preventing future strokes through managing risky medical conditions..
On the other hand, in the therapeutic intervention of cognitive impairment, specific stimulation programs for dementia will be useful, such as programs for the development and maintenance of specific cognitive functions.
In addition, multidisciplinary rehabilitation programs that combine both medical, neuropsychological, occupational, and psychological intervention will also be essential..
The best approach to this type of pathology is to start with the control of risk factors and therefore their prevention. It is essential to lead a healthy lifestyle, eat a balanced diet, exercise, avoid alcohol and / or tobacco consumption and also maintain a healthy weight.
References
- Álvarez-Saúco, M., Moltó-Jordá, J., Morera-Guitart, J., Frutos-Alegría, M., & Matías-Guíu Guía, J. (2005). Update on the diagnosis of vascular dementia. Rev Neurol, 41(8), 484-492.
- Bernal Pacheco, O., & Roman Campos, G. (2011). An approach to vascular dementia.
- Formiga, F., Fort, I., Robles, M., Riu, S., Rodríguez, D., & Sabartes, O. (2008). Differential aspects of comorbidity in elderly patients with Alzheimer's dementia or vascular dementia. Rev Neurol, 46(2), 72-76.
- Jodar Vicente, M. (2013). Neuropsychology of dementia. In M. Jodar Vicente, D. Redolar Ripoll, J. Blázquez Alisente, B. González Rodríguez, E. Muñoz Marrón, J. Periañez, & R. Viejo Sobera, Neuropsychology (pp. 407-446). Barcelona: UOC.
- NHI. (2015). Binswanger's Disease. Retrieved from National Institute of Neurological Disorders and Stroke: ninds.nih.gov
- NHI. (2015). Multi-Infact Dementia. Retrieved from National Institute of Neurological Disorders and Stroke: ninds.nih.gov
- NIH. (2015). The Dementia. Retrieved from National Institute of Neurologial Disorders and Stroke: ninds.nih.gov
- Ramos-Estebánez, C., & Rebollo Álvarez-Amandi, M. (2000). Binswanger's disease. Rev Neurol, 31(1), 53-58.



Yet No Comments