
Dystocia types and their characteristics
It is understood by dystocia to all those conditions that prevent labor from evolving naturally until its culmination. Dystocia can be of maternal origin or of final origin, although ultimately they all share a common denominator: the impossibility of the development of a normal labor, which makes obstetric intervention essential to be able to help the birth..
In some cases, dystocia is resolved by procedures known as obstetric instrumentation or, in other words, forceps-assisted delivery; when this is not possible due to the clinical situation, a cesarean delivery should be chosen.

In the past, dystocia was one of the main causes of maternal-fetal death. Fortunately, due to the development of modern obstetric techniques, dystocia are no longer associated with high mortality rates, although they do represent an important cause of maternal-fetal morbidity.
Article index
- 1 Characteristics of normal delivery
- 2 Types of dystocia
- 2.1 -Anatomical disturbances
- 2.2 -Functional disturbances
- 3 Treatment of dystocia
- 4 References
Characteristics of normal delivery
In order to understand why dystocia occurs, it is necessary to be clear about some concepts of normal delivery, otherwise it would be impossible to understand what happens for a delivery to be classified as dystocic.
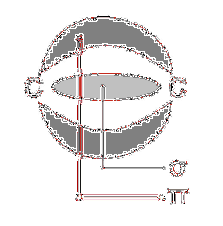
First of all, it is necessary to know that the female bony pelvis (the pelvic skeleton) has minimum transverse and anteroposterior diameters known as the narrows of the birth canal. These means are determined by pelvimetry making it possible to know in advance if it is feasible for the fetus to pass through the birth canal..
Under normal conditions, these diameters should coincide with the dimensions of the fetus's head (the most voluminous part of the body), so that during birth the head can pass through the straits without problems..
When the diameters of the pelvic straits are smaller than normal, the fetus has a larger than average size or an abnormal position, the relationship between the diameters of the mother and those of the fetus is compromised, thus making it impossible for this advance through the canal. of childbirth.
On the other hand, for a baby to be born it is necessary for the mother to have uterine contractions. These contractions known technically as "uterine dynamics" must have an intensity, duration and frequency determined according to each phase of labor; when this does not occur, labor does not progress properly.
Types of dystocia
Dystocia are a wide range of conditions that prevent labor from progressing naturally; They can be both anatomical and functional and depend on either the mother or the fetus.
-Anatomical dystocia
Anatomical dystocia are those conditions in which the diameters of the maternal pelvis and the fetal head (in some cases also the shoulders) do not correspond.
This is usually due to a small pelvis or a large fetus. In either case, the constrictions of the birth canal cannot be naturally overcome by the baby during birth..
Anatomic dystocia can be of maternal or fetal origin.
Dystocia of maternal origin
- Bony pelvic diameters smaller than normal.
- Alterations in the soft tissues of the birth canal (insufficient dilation of the uterine cervix, scars that compromise the compliance of the vaginal wall).
Dystocia of fetal origin
- Very large fetus (macrosomic fetus).
- Hydrocephalus (head is larger than normal).
- Abnormal presentation (improper position during delivery which implies that the fetus' diameters exceed the pelvic diameters).
-Functional dystocia
Functional dystocias are those that occur when all the anatomical elements are adequate, but labor does not progress adequately.
Functional dystocias are associated with the maternal component and have to do with the characteristics of uterine contraction.
For a successful labor to complete, uterine contractions must have a certain rhythm, intensity and duration at each stage of labor. As this progresses, all the elements (rhythm, intensity and duration) increase in intensity until reaching the peak during the last stage of labor (second stage)..
When this does not happen, the contractions are not effective and labor does not progress; This means that despite uterine contractions, they are not effective in progressing the fetus through the birth canal..
Depending on the alteration of uterine dynamics that occurs, functional dystocia can be classified into:
- Alteration of the frequency of contractions.
- Modification of the duration of contractions.
- Alteration of the basal tone of uterine contraction.
Each of these changes can be primary (the rate, tone or duration were never adequate from the onset of labor) or secondary (at first the rate, tone and duration were adequate but as labor progressed they changed to a pattern abnormal and inefficient).
The main characteristics of functional dystocias according to their type are presented below:
Alteration of the frequency of contractions
Typically, in normal labor there should be 3-5 contractions for every 10 minutes of labor. At first the number of contractions is low and as labor progresses they become more frequent, until reaching a frequency of one contraction per minute in the second stage..
We speak of oligosystole when the uterus contracts less than 2 times per 10 minutes, this frequency being insufficient to induce effacement of the cervix and the descent of the fetus through the different planes of the birth canal..
On the other hand, the mother is said to have polysystole when there are more than 5 contractions per 10 minutes. In this case, the frequent contractions end up exhausting the myometrium (muscular tissue of the uterus), reducing the effectiveness of the contractions (secondary decrease in tone and duration), which results in ineffective labor.
Modification of the duration of contractions
Normal contractions last on average 30 seconds.
When uterine contractions last less than 30 seconds and do not exceed 30 mmHg at their maximum peak, the patient is said to have hyposystole; On the other hand, when the contractions last more than 60 seconds with a peak of contraction that exceeds 50 mmHg, it is called hypersystole..
In the first case, the contractions are very brief and with a very low intensity to push the fetus through the birth canal, while in the second, the very frequent and intense contractions end up generating depletion of the myometrial energy, causing it to is not effective and therefore labor does not progress properly.
Altered basal tone of uterine contraction
During labor, the uterus presents a state of continuous contraction divided into two phases; a passive one in which it has a sustained basal tone, and an active one in which the maximum peak of contraction is reached.
The goal of active contraction is to push the fetus through the birth canal while the basal tone gives the myometrium an opportunity to recover but without the fetus rolling back; that is, the basal tone of the contraction is responsible for keeping everything in place.
When the basal tone of uterine contraction is less than 8 mmHg, it is called uterine hypotonia. In this case, the contraction causes the fetus to descend, but due to insufficient basal tone, the baby "returns" when the peak ceases and therefore does not advance through the birth canal..
On the other hand, when the basal tone of the contraction exceeds 12 mmHg, the patient is said to have hypertonia. At first glance, this may not seem like an inconvenience, since the high tone would help to keep the fetus in position and could even lower it a bit more..
However, a very high tone prevents the myometrium from recovering adequately between contractions, therefore the peak of each contraction will be less intense and therefore insufficient to make the fetus progress through the canal..
It is evident that the separation of the components of the uterine dynamics is artificial and its usefulness is only academic, since in reality they are concatenated and interdependent components where the failure of one will generally be associated with a modification of the others..
For example, a patient may have uterine hyperdynamia when hypersystolia and polysitolia are combined..
Treatment of dystocia
The treatment of dystocia will depend to a great extent on the moment in which they appear, the type of dystocia and the available resources.
In general, anatomical dystocia diagnosed in advance are planned for a cesarean delivery, however in cases where labor begins and at some point there is an unexpected disproportion, either a cesarean section can be chosen (the fetus has not progressed beyond second plane of the birth canal) or forceps (dystocia that present in the later stages of labor).
On the other hand, functional dystocia can be treated with some medications that induce and synchronize uterine contractions. One of the most widely used drugs for this purpose is oxytocin, which can be used either to induce labor or to correct functional dystocia on the fly..
However, in cases of fetal distress, hemorrhage or any indication of a major complication of labor, pharmacological measures should be avoided and an emergency cesarean section should be chosen, since generally this type of dystocia does not spontaneously progress to a level where it can resolve the delivery with obstetric instrumentation (forceps).
References
- Neilson, J. P., Lavender, T., Quenby, S., & Wray, S. (2003). Obstructed labor: reducing maternal death and disability during pregnancy. British medical bulletin, 67(1), 191-204.
- Lawson, J. B. (1967). Obstructed labor.
- Dolea, C., & AbouZahr, C. (2003). Global burden of obstructed labor in the year 2000. World Health Organization, 1-17.
- Fasubaa, O. B., Ezechi, O. C., Orji, E. O., Ogunniyi, S. O., Akindele, S. T., Loto, O. M., & Okogbo, F. O. (2002). Delivery of the impacted head of the fetus at caesarean section after prolonged obstructed labor: a randomized comparative study of two methods. Journal of obstetrics and Gynaecology, 22(4), 375-378.
- Chhabra, Deepa Gandhi, Meenakshi Jaiswal, S. (2000). Obstructed labor-a preventable entity. Journal of Obstetrics and Gynaecology, twenty(2), 151-153.
- Cedergren, M. I. (2009). Non-elective caesarean delivery due to ineffective uterine contractility or due to obstructed labor in relation to maternal body mass index. European Journal of Obstetrics & Gynecology and Reproductive Biology, 145(2), 163-166.
- Kwast, B. E. (1992). Obstructed labor: its contribution to maternal mortality. Midwifery, 8(1), 3-7.

Yet No Comments