
Duchenne muscular dystrophy symptoms, causes, treatment
The Duchenne muscular dystrophy (DMD) is a neuromuscular disease, characterized by the presence of significant muscle weakness, and a generalized and progressive development (World Health Organization, 2012).
It is the most common type of muscular dystrophy in humans (López-Hernández, 2009) and affects 1 in 3,500 children in the world (Duchenne Parent Project, 2012). For the most part, the disease affects men in the early stages of life (World Health Organization, 2012).
There are different types of muscular dystrophy. Symptoms typically begin during childhood. Weakness and loss of muscle mass cause serious difficulties in acquiring or maintaining the ability to walk, breathe, and / or swallow (Mayo Clinic, 2013).
Neuromuscular effects offer a chronic prognosis. In most cases, people with Duchenne muscular dystrophy die in young adulthood, due to the development of secondary pathologies such as heart failure or cardiomyopathies (World Health Organization, 2012).
Article index
- 1 What is Duchenne muscular dystrophy?
- 2 Statistics
- 3 Symptoms
- 4 Evolution of symptoms
- 5 Causes
- 6 Diagnosis
- 7 Treatment
- 8 Forecast
- 9 Current status of the investigation
- 10 Conclusions
- 11 Bibliography
What is Duchenne muscular dystrophy?
Duchenne muscular dystrophy is a disease that affects the individual through progressive muscle weakness and degeneration (Muscular Dystrophy Association, 2016).
Due to a genetic mutation, the absence of a specific protein in people with Duchenne muscular dystrophy will cause the loss of muscle functionality.
Generally, the symptoms usually appear in the lower extremities, spreading to the rest of areas.
Statistics
The World Health Organization (2012) indicates that the incidence of Duchenne muscular dystrophy is estimated at approximately 1 case per 3,300 inhabitants.
Specifically, some research shows that this disease affects 1 in 3,500 male children born alive (López-Hernández, 2009).
In the case of the US, it is not known with certainty how many people in all age ranges suffer from this disease. Some research has estimated that one in 5,600-7,770 male adults between the ages of 5 and 24 have a diagnosis of Duchenne or Becker muscular dystrophy (Centers for Disease Control and Prevention, 2015).
Symptoms
The most characteristic of the disorders that belong to the group of muscular dystrophies is the muscular weakness; However, depending on the type, specific symptoms may appear that will vary depending on the age of onset and the muscle groups affected (Mayo Clinic, 2013).
Normally, the development of Duchnne muscular dystrophy is quite predictable. Parents may observe some quite significant signs, such as difficulty or inability to learn to walk or abnormal increase in calf muscles (pseudohypertrophy) (Duchenne Parent Project, 2012).
Some of the most characteristic symptoms and signs of Duchenne muscular dystrophy that appear early in a child's life are (Mayo Clinic, 2013):
- Recurring falls.
- Difficulty or inability to get up or adopt a specific posture.
- Difficulty or inability to walk, run, or jump.
- Walk on the tip of the well.
- Muscle stiffness and / or pain in large muscle groups.
- Learning difficulties.
Similarly, the Duchenne Parent Projet association (2012) highlights the most common symptoms and clinical manifestations:
- Delayed language and speech acquisition.
- Difficulties and behavior problems.
- Learning difficulties.
- Muscular weakness.
- Contractures and stiffness in joint areas.
- Pseudohypertrophy in the calf muscles.
- Lordosis.
- Cardiac and respiratory muscle weakness.
Evolution of symptoms
All muscle symptoms begin with weakness of the muscles of the pelvic girdle, calves, and various gait disturbances that are significant before 5 years of age (López-Hernández, 2009).
In preschool, children with Duchenne muscular dystrophy may fall frequently or have difficulty walking, climbing steps, and / or running (Duchenne Parent Project, 2012).
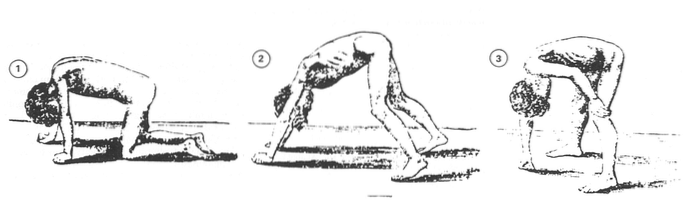
As the disease progresses, at school age, it is quite likely that children use only the tips of their feet to walk. We will be able to observe a rolling and unsafe march that can cause numerous falls. They usually use some strategies to maintain their balance such as pushing their shoulders back or holding onto their own body (Duchenne Parent Project, 2012).
Around 9 years of age, most people with this disease are unable to walk, due to this they begin to develop numerous musculoskeletal deformities -scoliosis, contractures, etc.- (López-Hernández, 2009).
In the adolescent stage, they will present significant difficulties in efficiently executing activities related to the use of the upper extremities, legs or trunk. At this stage they will require support and help of a mechanical nature (Duchenne Parent Project, 2012).
Muscle degeneration and weakness continue to advance until reaching the muscles responsible for respiratory and cardiac function (López-Hernández, 2009). Due to all this, the survival of the patient is seriously compromised, causing death in most cases..
Causes
Various genes have been identified that are involved in the production of proteins that are responsible for protecting muscle fibers against possible damage and injury (Mayo Clinic, 2013).
Specifically, each type of muscular dystrophy occurs as a consequence of a particular genetic mutation. Some of these mutations are inherited; however, in most cases they occur spontaneously during pregnancy (Mayo Clinic, 2013).
In the case of Duchenne muscular dystrophy, the researchers identified a specific gene located on the X chromosome that could present the mutation responsible for this pathology (Muscular Dystrophy Association, 2016).
Thus, in 1987, the protein associated with this gene was identified., dystrophin. Thus, the lack or absence of this protein implies that the muscles are fragile and easily damaged (Muscular Dystrophy Association, 2016).
In addition, a recessive inheritance pattern linked to the X chromosome has been identified, with the carrier being the mother (Muscular Dystrophy Association, 2016). Due to this fact, this type of disease is more frequent in men than in women..
Men have an XY chromosome composition, while women are XX. Therefore, if an X chromosome has a mutation in the DMD gene, it will suffer from Duchenne muscular dystrophy due to the absence of dystrophin production (National Human Genome Research Institute, 2013).
However, in the case of women who have two X chromosomes and therefore two copies of the DMD gene, if one of these is altered, the other will be able to continue producing dystrophin and therefore maintain muscle neuroprotection (National Human Genome Research Institute, 2013).
Diagnosis
In this type of pathologies, different interventions can be carried out to determine its diagnosis (National Human Genome Research Institute, 2013).
The clinical diagnosis can already be made when a child begins to develop progressive muscle weakness. Already at 5 years of age there are obvious symptoms. If an early intervention is not carried out, children will present functional dependence before the age of 13 (National Human Genome Research Institute, 2013).
Apart from observation and clinical examination, some of the following techniques can be used to identify the presence of Duchenne muscular dystrophy (Mayo Clinic, 2013):
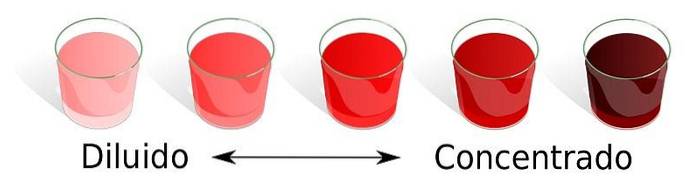
- Enzyme tests- Damaged muscles can release various enzymes, such as creatine kinase (CK). The presence of abnormally high levels suggests the presence of some type of muscle pathology.
- Electomyography: changes in muscle electrical patterns can suggest or confirm the presence of a muscle disease.
- Genetic studies: performed to detect possible genetic mutations that lead to the development of various types of muscular dystrophy.
- Muscle biopsy: the extraction of small portions of muscle tissue are useful for the detection of micro and macroscopic damage in muscle groups.
- Cardiac and respiratory tests: they are essential to detect the possible extension of muscle weakness and atrophy.
Treatment
At present, a cure for Duchenne muscular dystrophy has not been identified (Duchenne Parent Project, 2012).
Despite this, various treatments are used that have proven to be effective both for reducing symptoms and for improving the quality of life of people suffering from this type of pathology (Duchenne Parent Project, 2012).
This disease, due to the clinical progression and the wide variety of symptoms, will require a multidisciplinary and comprehensive intervention performed by a wide variety of specialists: pediatrician, physiotherapist, neurologist, neuropsychologist, occupational therapist, speech therapist, nutritionist, endocrinologist, geneticist, cardiologist , pulmonologist, orthopedist, rehabilitator and surgeon, among others (Duchenne Parent Project, 2012).
In many cases, specialists can recommend pharmacological interventions (Mayo Clinic, 2013):
- CorticosteroidsSome of the drugs in this group can improve muscle strength and control the progression of muscle degeneration (Mayo Clinic, 2013). However, the repeated use of these drugs can cause side effects such as weight gain or bone weakness (Mayo Clinic, 2013).
- Cardiac drugs: angiotensin inhibitors or beta blockers may be beneficial when muscular dystrophy has reached the cardiac muscle groups (Mayo Clinic, 2013).
Not only are drugs useful for intervention in Duchenne muscular dystrophy, there are both therapeutic interventions and care methods that can improve the quality of life of these people (Mayo Clinic, 2013).
Some beneficial interventions are (Duchenne Parent Project, 2012):
- Stretching and muscle movement exercises.
- Aerobic and Strengthening Exercise.
- Mobility methods: canes, walkers, wheelchairs, etc..
- Orthopedic methods: night splints, long leg or hand.
- Respiratory assistance: artificial respiration, non-invasive ventilation, assisted cough, etc..
Forecast
Until relatively few years ago, people with Duchenne muscular dystrophy did not survive much longer after reaching adolescence (Muscular Dystrophy Association, 2016).
The great advances in medical, technical and genetic research have managed both to slow the progression of the disease and to grant a considerable increase in the quality of life to individuals who suffer from it (Muscular Dystrophy Association, 2016). In this way, cardiac and respiratory care is essential for the preservation of vital functions (Muscular Distrophy Association, 2016).
In many cases, they are capable of reaching the post-adolescent stages. More and more cases of Duchenne muscular dystrophy are described in adults in their 30s, including people who survive to 40 and 50 years (Muscular Dystrophy Associatin, 2016).
Actual state of the investigation
Currently, clinical trials and research are oriented towards the development of gene therapies that modify mutations and deficiencies in dystrophin production (Muscular Dystrophy Association, 2016).
Some of the most investigated mechanisms are (López-Hernández, 2009):
- Replacement of the damaged gene.
- Endogenous gene modification (exon skipping and stop codon skipping therapy).
- Overexpression / inhibition of phenotype modifiers.
Conclusions.
Duchenne muscular dystrophy is a severely disabling disease in both children and young adults with a devastating prognosis..
Despite the fact that clinical and experimental research has achieved important advances in the treatment of symptoms, there is still no cure for this type of pathology..
A thorough understanding of the biological and genetic basis is essential in order to find a curative treatment for Duchenne muscular dystrophy..
Bibliography
- CDC. (2016). Centers for Disease Control and Prevention. Retrieved from Muscular Dystrophy: cdc.gov.
- DPP. (2016). What is Duchenne? Obtained from the Association Duchene Parent Project Spain: duchenne-spain.org.
- López-Hernández, L. B., Vázquez-Cárdenas, N. A., & Luna-Padrón, E. (2009). Duchenne muscular dystrophy: topicality and prospects for treatment. Rev Neurol , 49 (7), 369-375.
- Mayo Clinic. (2014). Diseases and Conditions: Muscular dystrophy. Obtained from Mayo Clinic: mayoclinic.org.
- MDA. (2016). Duchenne Muscular Dystrophy (DMD). Obtained from Muscular Dystrophy Association: mda.org.
- NHI. (2013). Learning About Duchenne Muscular Dystrophy. Obtained from National Human Genome Research Institute: genome.gov.
- WHO. (2012). United to fight rare diseases. Obtained from World Health Organization: who.int.
- Image source.


Yet No Comments