
Precordial pain characteristics and causes
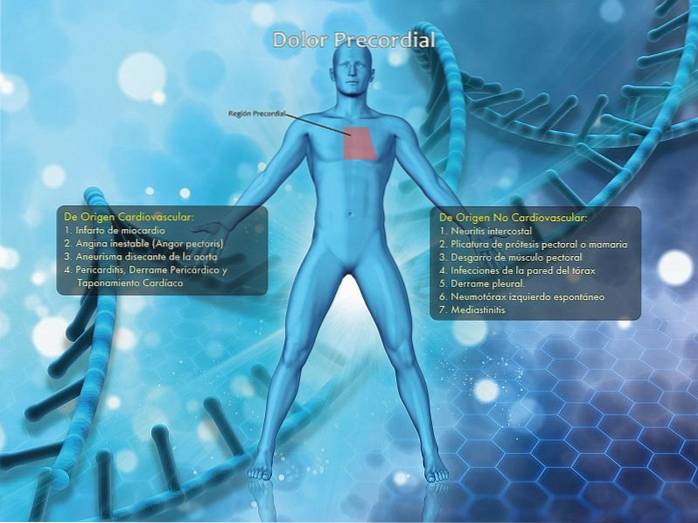
The precordial pain It is a symptom that can be present in many diseases and may or may not have a cardiac origin, hence the importance of knowing how to differentiate it. It is a pain that occurs in the so-called precordial region, an area framed within the anatomical limits that can be seen in the lower image.
It is important to note that in medicine there are two well differentiated basic concepts: signs and symptoms. Sign is a verifiable finding. For example: blood pressure, temperature, heart rate or pulse, a mass in the abdomen, a skin lesion, etc. It is an objective element that can also be found and described by another person.
Symptom is a subjective element, as it depends exclusively on the patient's description. It is the person who reports what they are feeling: heat, cold, pain, absence of sensations, numbness, etc..
In the particular case of chest pain, this is the symptom of a large number of diseases that can have varying degrees of severity. Some mild, such as intercostal neuritis (very painful), or very severe, such as a myocardial infarction (perhaps not so painful) or a dissecting aortic aneurysm (extremely painful and severe).
We will review some of the different causes of chest pain, detailing the symptoms and signs that may accompany them to learn to differentiate them from each other; likewise, some indications in the presence of some of them.
Regarding its causes, we will divide them into causes of cardiovascular origin and of non-cardiovascular origin. Among the causes of cardiovascular origin we find:
- Myocardial infarction
- Unstable angina (angor pectoris)
- Dissecting aneurysm of the aorta
- Pericarditis, pericardial effusion, and cardiac tamponade.
Among the causes of non-cardiovascular origin we find:
- Intercostal neuritis
- Pectoral or breast prosthesis plication
- Pectoral muscle tear
- Chest wall infections
- Pleural effusion.
- Spontaneous left pneumothorax
- Mediastinitis.
Article index
- 1 A.D.L.I.C.I.D.A.E.C.
- 2 Causes of cardiovascular origin
- 2.1 Unstable angina (Angor pectoris)
- 2.2 Dissecting aneurysm of the aorta
- 2.3 Pericardial effusion, pericarditis, and cardiac tamponade
- 3 Non-cardiovascular causes of origin
- 3.1 Intercostal neuritis
- 3.2 Plication of breast or breast prosthesis
- 3.3 Pectoral muscle tear
- 3.4 Chest wall infections
- 3.5 Pleural effusion
- 3.6 Spontaneous left pneumothorax
- 3.7 Mediastinitis
- 4 References
A.D.L.I.C.I.D.A.E.C.
Before describing the different causes of chest pain, it is essential to know a tool used by physicians to assess pain. This allows to quickly establish the origin or cause of pain and thus guide the diagnosis and treatment plan.
It is an acrostic that forms the "word" ADLICIDAEC.
A: Appearance. In what form did the pain appear.
D: Triggers. If there was any previous event (effort, food, etc.).
L: Location. Where is located and delimit the painful area as best as possible.
I: Intensity. Mild, moderate or severe, depending on the patient's criteria.
C: Character. Colic, burning (burning), oppressive (like a weight), boring, etc..
I: Irradiation. If it spreads to a region neighboring the area where it originally started.
D: Duration and frequency. Whether it occurs continuously or with a lull, and how often.
A: Mitigators. If there is position, movement, medicine or other that helps calm him.
E: Exacerbants. If, on the contrary, there is something that increases its intensity and frequency.
C: Concomitants. If in addition to the pain there are any other symptoms present such as nausea, vomiting, burning in an area, fever, etc..
All pain should be described in this way in the most detailed way possible to guide the diagnostic plan, and chest pain is no exception..
For the description of the different causes (which is what is called differential diagnoses) we will adhere to this methodology, which will facilitate the understanding of each one of them..
Causes of cardiovascular origin
Myocardial infarction
The most feared cause of chest pain in the general population. Its origin is established, among others, the existence of obstruction of various degrees and location at the level of the coronary arteries.
When a segment of one of these closes, the region dependent on that blood flow becomes "infarcted" (ischemia occurs, due to the absence of oxygen in the tissue) and the corresponding tissue dies, thus causing pain.
Its onset is sudden, when pain is present (because the most lethal forms are usually painless), located in the precordial region, of variable intensity, but persistent.
It may be oppressive in nature, but is occasionally burning or tearing, and the radiation pattern occupies the left side of the left neck, jaw, shoulder, and arm, and may extend to the upper and medial abdomen (epigastrium).
The duration is variable, and can even be several days of evolution and the person attributes it to stomach "acidity", depending on the extent of the compromised heart tissue..
It has no extenuating or exacerbating factors and may present with nausea, vomiting, hypotension, paleness, and cold sweating. The ever-present symptom of a feeling of imminent death that the person has.
It is rarely related to emotional events as it has been extended by tradition, but it is closely related to stress and a lifestyle oriented to a lot of activity and little rest and sleep.
The treatment of myocardial infarction will depend on the extent of it, the time of diagnosis (how many hours have passed), the compromise in the patient's physical condition and age. But it will always be in a Coronary Care Unit.
The infarcted area will not recover, since it is the death of that tissue that causes the pain. Hence, the full functionality of the heart is compromised..
Unstable angina (Angor pectoris)
By various mechanisms, there is the occlusion or spontaneous closure of one or more of the arteries that supply the heart (coronary arteries), producing sudden onset pain and generally associated with some previous effort (aerobic exercise, climbing stairs or similar).
It is, of course, located in the precordial region and its character is oppressive (feeling of a great weight on the thorax), with intensity that can range from moderate to severe. It will reproduce the same irradiation pattern as myocardial infarction pain, with the exception of the epigastrium.
It can calm down spontaneously or with the administration of drugs known as nitrates sublingually and give up completely, while it will increase its intensity and duration of persisting the triggering stimulus, being able to reach syncope (fainting) product of the same intensity of the pain.
Anginal pain has the peculiarity of not causing a sensation of imminent death, an important fact for the doctor when establishing a differential diagnosis.
Its definitive treatment involves catheterization or bypass of the compromised coronary vessels. Nitrate treatment is only to avoid the appearance of symptoms.
Dissecting aneurysm of the aorta
An aneurysm occurs when the wall of an artery weakens, causing the involved portion to bulge. It can be congenital or have many other causes (infectious, traumatic, etc.).
When it happens in the aorta it is good to remember that this is the largest artery in the body and crosses the thorax and part of the abdomen, along the midline of the body, just in front of the spinal column and on one side of the esophagus..
The installation of the aneurysm is a progressive process, but the pain when the dissection of this vessel occurs simulates a large tear in the posterior part of the sternum that at the beginning can be confused with a large myocardial infarction.
Characteristic of this pain is its sudden onset, with or without an apparent trigger, located just behind the sternum, of very strong intensity and of an oppressive and burning nature..
It radiates to the back, and occupies the area between the two scapulae (shoulder blades), being persistent, without extenuating factors and can be exacerbated when walking. It will rarely radiate to the left neck, shoulder or arm.
It will always be accompanied by hypotension, paleness, cold sweats, great manifestations of pain and a sensation of imminent death..
Its diagnosis is tomographic and constitutes a true cardiovascular surgical emergency that puts life at serious risk..
Pericardial effusion, pericarditis, and cardiac tamponade
The pericardial cavity is also a virtual cavity, like the pleural cavity.
It forms in the middle of the membrane that lines the heart, called the pericardium, and is contained within the mediastinum. It has a certain minimum amount of fluid that lubricates the space and allows the heart to move when beating without friction between the membranes.
The origin of any of these three processes is highly variable: infections of the heart or of the pericardium itself, tuberculosis, tumors, some diseases such as dengue or other similar ones, spontaneous effusions in immunocompromised patients, wounds from knives or firearms, rib fractures, etc.
Pain is not your most relevant symptom, but it can occur. When it does, it is in a very insidious way, with no apparent triggers, that it evidently occupies the pericardial region.
Its intensity is generally mild and of a dull or oppressive character, not irradiated or radiating to the left neck and shoulder, without mitigating factors and can be exacerbated by exertion..
The accompanying signs are those that will give the diagnostic orientation: hypophonic heart sounds (difficult to auscultate due to their low intensity), hypotension, paradoxical pulse, the appearance of some specific waves in the neck vessels that will show fullness and the difficulty respiratory tract that is generally associated.
The differences between one and the other will be given by the quantity and quality of the fluid: pericardial fluid in the case of the effusion, infectious (pus) in the pericarditis and usually blood in the tamponade.
Diagnosis is made by echocardiography (transthoracic or transesophageal) and tomography, but even plain chest radiography can show signs suggestive of these..
Treatment is the urgent drainage of the fluid, depending on its nature: the only pericardiocentesis directed by echo or not in the case of pericardial effusion, the drainage plus antibiotic therapy in the pericarditis (depending on its extension) and surgery in the case tamponade, as the cause of bleeding must be established and corrected.
Non-cardiovascular causes of origin
Intercostal neuritis
Caused by "irritation" or inflammation of any of the intercostal nerves, located just on the inside of the lower edge of each rib. Usually of sudden onset, without apparent triggers, although it is known that most of the time there is an emotional background or stress situation at its origin.
Located most of the time in the area near the nipple in men and the base of the breast in women, and its extension can be delimited because it runs along one of the spaces between two ribs (usually the fourth , fifth or sixth Intercostal space).
Moderate to strong intensity and "burning" or burning character; the person feels that sensation or like a tear. It rarely radiates to the armpit, neck, shoulder, or arm on the same side.
Its duration is variable; days to weeks. It is attenuated in some occasions when the person bends over himself or compresses the painful area, and of course after the administration of analgesics, to reappear when the effect of these ceases.
It is exacerbated or increased in intensity when taking a deep breath or coughing or when the lower border of the rib of the involved nerve is pressed. Very rarely another symptom coexists.
The treatment is aimed at achieving analgesia and muscle relaxation, since the anxiety it causes also increases its intensity; in addition, the administration of B complex vitamins and rest is incorporated.
Pectoral or breast prosthesis plication
Caused by the impingement of any of the muscles of the anterior aspect of the thorax by a breast or pectoral prosthesis that has been displaced.
The description of the pain is very similar to that of intercostal neuritis, with a significant history of the placement of the pectoral prosthesis in men or breast prosthesis in women and generally associated with some previous trauma.
The treatment is also aimed at analgesia and relaxation, but requires surgery for the definitive resolution when repositioning the prosthesis..
Pectoral muscle tear
Relatively common in weightlifting or bodybuilding practitioners. It is the most important antecedent, since its sudden appearance is usually associated with lifting excess weight for the first time.
It is an extremely intense pain, which can knock the person to the ground while bringing their hands to the site of the tear and when it occurs on the left side of the chest it can simulate a "heart attack" for those who are unfamiliar with the matter, given the sensation of depth origin of pain.
Due to its location (generally on one side of the thorax), all the symptoms are very similar to the previous two, as well as the treatment, which in this case will include the prohibition of lifting weight for 3 to 6 months.
Chest wall infections
Chest wall infections are extremely rare and are generally associated with a previous surgical procedure, which constitutes the most important distinctive antecedent.
Its appearance is progressive, insidious; frequently associated with some trauma, and the person can precisely delineate the area involved in most cases.
Its intensity is variable, usually mild to moderate, and of an oppressive nature or producing a sensation of "weight". Likewise, the duration is variable.
It is attenuated with analgesics and rest, or with physical means (local ice), and is exacerbated with movements, especially those that require specific work on the pectoral muscles. It can coexist with fever and general malaise of variable expression, depending on the extent of the infectious process.
Treatment involves the use of antibiotics, in addition to analgesia, relaxation and rest, and there may be a need to hospitalize the patient depending on the extent of the infection and the clinical condition of the person..
Pleural effusion
The pleural cavity is a virtual cavity that is established between the lungs and the thoracic cavity through a membrane (the pleura) that covers them both, similar to the pericardial cavity that we described earlier.
So that there is no friction between both membranes with respiratory movements, the body maintains a certain minimum amount of fluid that lubricates the cavity.
When this fluid exceeds normal, a pleural effusion occurs; fluid builds up at the base of the chest cavity, above the diaphragm, restricting the expandability of the lungs and compromising respiratory function.
This virtual space is subject to the appearance of infections and effusions, and the causes are the same as those mentioned when we speak of pericardial effusion, so the presence or absence of previous pathologies that could be its origin must be established.
The pain will also appear in a very insidious way, settling over several days, being located at the base of the lungs, with variable intensity and of an oppressive nature; It is rarely irradiated and when it does it is usually to the back or abdomen.
The distinctive characteristic sign is the restriction for breathing, and signs of respiratory effort may appear (inter- or subcostal and suprasternal tracing) and the complete abolition of respiratory sounds on auscultation at the level of the effusion..
Treatment involves performing a thoracotomy to place a chest tube and drain the fluid from the effusion, in addition to treating the cause of its origin..
Spontaneous left pneumothorax
A pneumothorax is the presence of free air inside the pleural cavity, outside the lungs, which causes them to collapse and limits respiratory function.
In this case, it can be produced by two mechanisms: trauma (the most frequent, especially in athletes who play soccer or basketball and receive a hit with a ball or the elbow of another player) and, more rarely, the spontaneous rupture of a bull ( concentration of air in an area of the lung, usually of congenital origin).
It is a very spectacular onset because immediately after the event that triggers it, in addition to the pain of strong intensity and burning character, an acute respiratory failure of variable degree immediately occurs that can compromise the life of the person.
It can radiate to the left neck, shoulder and arm, pretending to be of cardiac origin.
Emergency treatment involves drainage of the air contained in the pleural cavity by means of a thoracotomy: placement of a chest tube.
Mediastinitis
Mediastinitis is an infectious process that occurs at the level of the mediastinum, a virtual cavity right in the center of the thorax and occupied by the heart, esophagus, and great vessels..
Its origin is varied: from a fish bone that has crossed the wall of the esophagus to viral or spontaneous infectious processes in a patient with compromised immune system.
The pain is usually insidious onset, without apparent triggers, located in the back of the sternum and of mild to moderate intensity; some qualify it as a “dull” pain, because it is difficult to define.
It can radiate to the area between the two scapulae on the back and be continuous, without extenuating or exacerbating.
Usually it is accompanied by the progressive and rapid deterioration of the patient once the pain settles; fever may or may not be present, depending on the patient's immune competence.
If the diagnosis is not suspected and established (through X-ray and / or Tomography), the outcome is generally fatal..
The treatment is carried out with the patient hospitalized in an Intensive Care Unit, and keeping strict vigilance on its evolution, as it can directly compromise the heart or the great vessels.
Conclution
As we can see, chest pain is not always associated with myocardial infarction and other coronary artery diseases..
Its origin is very diverse and involves, above all, the performance of a correct and exhaustive interrogation with an adequate semiological qualification of the pain.
The physical examination will confirm or rule out initial suspicions, thus establishing a diagnostic plan that includes the performance of specific studies and procedures and, depending on the findings, the treatment plan..
References
- Ilangkovan N, Mickley H, Diederichsen A, et al. Clinical features and prognosis of patients with acute non-specific chest pain in emergency and cardiology departments after the introduction of high-sensitivity troponins: a prospective cohort study BMJ Open 2017; 7: e018636.
- Domínguez-Moreno R, Bahena-López E, Neach-De la Vega D, Venegas-Román A, et al. Management of chest pain. Med Int Mex. 2016 Jul; 32 (4): 461-474.
- María Pérez-Corral, et al. Risk stratification in chest pain in the emergency room. Systematic review. Systematic review. Nure Inv. 2018; 15 (92): 1-11.
- Bañol-Betancur JI, Martínez-Sánchez LM, Rodríguez-Gázquez MA, et al. Characterization of chest pain in patients who consult the Emergency Service of a highly complex health institution, in the period 2014-2015, in Medellín, Colombia. Rev Soc Esp Pain 2017; 24 (6): 288-293.
- Mark H. Ebell. Evaluation of Chest Pain in Primary Care Patients. Am Fam Phys. 2011; 83 (5): 603-605.
- Yépez M. Sara Ninibeth. Prevalence of Precordial Pain Causes in the Teodoro Maldonado Hospital Emergency, Guayaquil, Ecuador. Thesis. May, 2018.
- Konstantinos Boudoulas and Danielle Blais. Acute Coronary Syndrome (ACS): Initial Evaluation and Management. 2018. The Ohio State University Wexner Medical Center.
- Castellano Ramiro, Muntaner Juan, et al. Management of the Patient with Precordial Pain. Argentine Federation of Cardiology. Recovered from: fac.org.ar.



Yet No Comments