
Hypothalamic-pituitary-ovary axis structure and functions
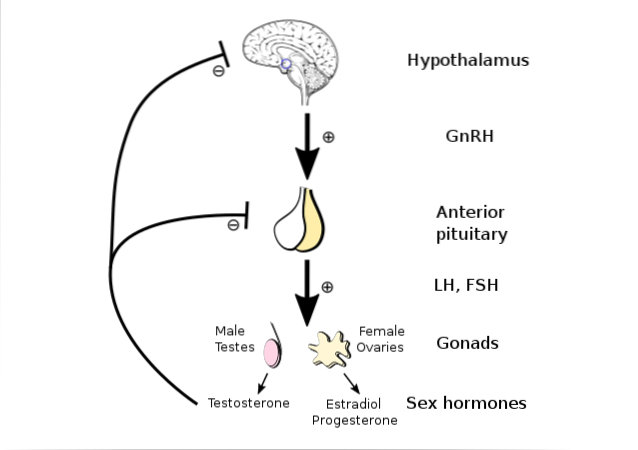
The hypothalamic-pituitary-ovarian axis It is one of the several similar hierarchical organizations that the body has to regulate the activity of some endocrine glands, whose secretion products are essential hormones for the proper development of certain bodily functions.
Although other similar organizations are also described as hypothalamic-pituitary-peripheral gland axes (adrenal or thyroid), their similarity is only in organization, since the hypothalamic, pituitary and peripheral gland cells, as well as the chemicals involved, are different.
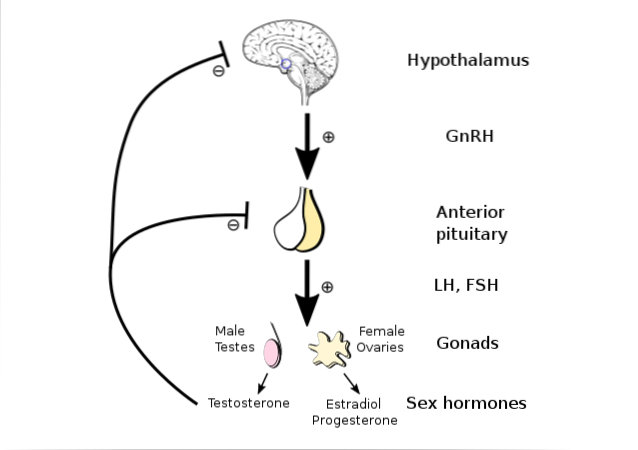
They are hierarchical organizations because they have three levels: an upper one represented by a group of neurons of the central nervous system at the hypothalamic level, an intermediate one at the level of the pituitary gland and a lower or peripheral one in the gland in question, where the elements would be found. regulated endocrines.
Communication between the different levels is of a chemical nature. Hypothalamic neurons synthesize and release substances in the hypothalamic-pituitary portal system that reach the pituitary and promote the release of hormones that in turn favor the peripheral release of specific hormones.
Article index
- 1 Structure
- 1.1 The “hypothalamus” component
- 1.2 "Pituitary" component
- 1.3 "Ovary" component
- 2 Functions
- 2.1 - The ovarian cycle
- 2.2 - The menstrual cycle or uterine cycle
- 3 References
Structure
Component "hypothalamus"
It is the upper level of the axis and is represented by a set of neurons at the level of the infundibular nucleus of the mediobasal hypothalamus and the preoptic region of the anterior hypothalamus. These neurons synthesize gonadotropin-releasing hormone, or GnRH, for its acronym in English..
The gonadotropin hormone is a decapeptide released by "hypothalamic" axons at the level of the median eminence. From there it diffuses into the blood and reaches the hypothalamic-pituitary portal system to the adenohypophysis, where it exerts its effect on the gonadotropin-producing cells..
The hypothalamic secretion of gonadotropins is not continuous, but occurs in the form of pulses that last between 5 and 20 minutes and repeat every 1 or 2 hours. Its secretion increases, by increasing the frequency of the pulses. Its continuous release has no effect on the release of gonadotropins.
Component "pituitary"
These are two special and differentiated cell groupings of the adenohypophysis, which each produce a different hormone. Both hormones are collectively called "pituitary gonadotropins" because they modify gonadal activity..
Gonadotropic hormones include follicle-stimulating hormone, or FSH, and luteinizing hormone, or LH. Both are small glycoproteins with a molecular weight of around 30 kDa, and they are released into the blood in the pituitary sector of the hypothalamic-pituitary portal system..
Cyclical fluctuations in the pituitary release of FSH and luteinizing hormone are responsible for the processes that occur during cyclical follicular maturation and the variations in ovarian hormonal secretions that produce the different changes that occur during the female sexual cycle..
Component "ovary"
These are the last component of the shaft. These are the two gonads of the female reproductive system and are located in the pelvic cavity, on each side of the uterus and near the fallopian tubes, included in the peritoneal ligaments that connect the uterus to the pelvic wall.
They include cells whose progressive maturation can reach the end and end up producing an egg that, when released, penetrates a tube and is fertilized by a sperm, would reach the status of a zygote for the production of a new being..
If fertilization does not occur, the released egg dies, the changes produced in preparation for pregnancy return, and the maturation cycle repeats, giving another egg a chance, and so on throughout the female fertile life span from puberty. until menopause.
Features
The main function of the hypothalamic-pituitary-ovary axis is to cyclically promote the maturation of the female ovum in the ovary, its release into the tubes at the time of ovulation and its ability to be eventually fertilized..
This process of maturation at the ovarian level is also accompanied by the preparation of the female organism for pregnancy, which implies a series of modifications such as those that occur at the level of the uterus and make it suitable for the implantation and nutrition of the fertilized ovum..
The axis works through cyclical changes in hormonal secretory activity at different levels. Changes in activity at a higher level have an impact on changes in activity at the next level and changes at the lower level are fed back by modifying the activity of the higher ones..
Although the activity changes in the axis are coordinated and result from sequential processes that are part of a single cycle that could be called the “female sexual cycle”, 2 cycles controlled by the function of the axis can be differentiated: an ovarian cycle and a menstrual cycle or uterine.
- The ovarian cycle
This includes, as its name suggests, all the changes that occur in the ovary during the female sexual cycle, and that are in some way promoted by changes in the secretions of pituitary gonadotropins (FSH and LH) in response to hypothalamic gonadotropin..
Menstruation is a uterine bleeding process that is described within the menstrual cycle, and that is taken as a starting point for both this cycle and the ovarian cycle..
On the first day of menstruation, the ovarian cycle begins, which will last 28 days, lasts until the new menstruation and is divided into two phases that span 14 days each: a follicular phase and a luteal phase; separated by day 14, at which time ovulation occurs.
Follicular phase
At the beginning of this phase, a small increase in FSH secretion begins to occur, whose levels were very low during the last day of the previous cycle. This hormone promotes the initiation of maturation of a group of primordial follicles each containing an oocyte or egg cell..
During this phase, only one of the developing follicles becomes dominant and reaches the appropriate maturity, becoming a De Graaf follicle that has granular cells (which produce estrogens) and thecal cells (which produce progesterone), and within which is the egg that will be released.
Around day 12 of the cycle, estrogen production increases considerably and promotes the release of luteinizing hormone and FSH at the pituitary level. The intense release (spike) of luteinizing hormone then promotes ovulation and the end of the follicular phase.
Luteal phase
It begins immediately after ovulation and is so called because the rest of the follicle that released the ovum remains in the ovary and acquires a yellowish color for which it is called the corpus luteum. It continues to produce estrogens and begins to produce large amounts of progesterone..
If within 8 to 10 days no signal reaches the corpus luteum that the released egg has been fertilized and successfully implanted, this structure rapidly degenerates and stops producing estrogens and progesterone, and the effects produced by these hormones return.
During the luteal phase, the estrogens and progesterone produced, together with another substance called inhibin and also produced by the granulosa cells, keep the production of FSH and luteinizing hormone by the pituitary inhibited, probably making the pituitary insensitive to the gonadotropin action.
When the production of sex hormones is suppressed by the degeneration of the corpus luteum, the inhibition they exerted on the pituitary disappears, FSH levels rise a little again and a new cycle begins..
- The menstrual cycle or uterine cycle
Its onset marks it, like that of the ovarian, the first day of menstruation. Its duration is identical (28 days) to that of the ovarian cycle, since its characteristics depend on the variations in sex hormones that occur during the latter.
Three distinct phases are recognized during the menstrual cycle: menstruation, the proliferative phase, and the secretory phase..
Menstruation
This is actually the final phase of a sexual cycle, but it is taken as the initial phase of the next cycle because it coincides with the beginning of the ovarian cycle and because it is obviously an easily identifiable sign. Its duration is on average about 4 or 5 days.
Menstruation is the result of the process of bleeding and "peeling" and elimination of all endometrial tissue accumulated during the previous ovarian cycle. It is produced by the atrophy and involution of the corpus luteum, which does not produce more estrogens and progesterone to support endometrial growth.
Proliferative phase
It begins immediately after the end of menstruation, when the ovarian cycle has already begun and the granular cells of the developing follicle have started a new production of estrogens that drive the proliferation of the structures of the endometrial mucosa..
Under the effect of estrogens, the uterine mucosa thickens progressively and increases its vascularity, a process that lasts until the time of ovulation and therefore lasts between 10 and 12 days..
Secretory phase
It begins after ovulation, when the corpus luteum has already formed and its thecal cells have begun to produce progesterone, a hormone that adds its action to that of estrogens, which continue to be produced, and that promotes the accumulation of glandular nutritive material.
The result of the proliferative and secretory phases is the modification of the uterine mucosa so that it acquires the appropriate conditions that allow it to serve as a seat for a fertilized egg that, when implanted properly, grows and develops as an embryo.
References
- Ganong WF: Reproductive Development & Function of the Female Reproductive System, 25th ed. New York, McGraw-Hill Education, 2016.
- Guyton AC, Hall JE: Female Physiology before Pregnancy and Female Hormones, in Textbook of Medical Physiology , 13th ed, AC Guyton, JE Hall (eds). Philadelphia, Elsevier Inc., 2016.
- Rieger L, Kämmerer U, Singer D: Sexualfunctionen, Schwangerschaft und Geburt, In: Physiologie, 6th ed; R Klinke et al (eds). Stuttgart, Georg Thieme Verlag, 2010.
- Werny FM, Schlatt S: Reproduction, in Physiologie des Menschen mit Pathophysiologie, 31th ed, RF Schmidt et al (eds). Heidelberg, Springer Medizin Verlag, 2010.
- Widmaier EP, Raph H and Strang KT: Female Reproductive Physiology, in Vander's Human Physiology: The Mechanisms of Body Function, 13th ed; EP Windmaier et al (eds). New York, McGraw-Hill, 2014.



Yet No Comments