
Systemic lupus erythematosus (SLE), symptoms and treatment

Systemic lupus erythematosus (SLE) "is an autoimmune and multisystemic disease characterized by inflammation, affecting a wide variety of body organs, such as the skin, joints, kidneys or lungs, among others." (Greco, Nakajima and Manzi, 2013). Blood vessels are also affected, lupus causes tissue damage in affected organs and generalized inflammation.
Contents
- An autoimmune disease
- Diagnostic criteria: Systemic lupus erythematosus (SLE)
- ACR: 11 Diagnostic Criteria
- Prevalence of systemic lupus erythematosus (SLE)
- Types of lupus
- Treatment for lupus patient
- Psychology, metamorphosis and healing path for lupus patient
- The "lupus" seeking healing steppes
- 11 Tips for a Lupus Patient
- Links
An autoimmune disease
Chronic non-communicable diseases (NCDs) are on the rise worldwide, lupus is one of them, it represents one of the most characteristic autoimmune diseases, the peculiarity of this disease is that it can attack any part of the body, it is not specified to certain systems as occurs in other conditions of this type, that is why it is said to be "systemic".
Our immune system helps us fight different fungi, microbes, parasites, viruses, bacteria, protozoa and other agents from the external and internal environment, however under some specific circumstances the immune system attacks the organism itself, it is "like leading to an enemy inside and not knowing when to attack ”, the immune response acts in the body exacerbating the symptoms of the disease.
The etiology of the disease is multifactorial, recent research has taken into account the genetic component, which is not determining, its etiology is influenced by other factors. It generally appears at the beginning of youth up to the age of forty, manifests a chronic, oscillating course, with periods of exacerbation of symptoms and remission of symptoms (Zhu, Tam & Li, 2011).
The "reverse phenomenon of disease grief" occurs when medications allow the patient to be physically in remission, yet feelings of emotional distress and psychological problems persist. The reactivity can be caused due to certain factors such as ultraviolet (UV) rays, it is necessary for people with lupus to protect themselves from solar photodamage and from fluorescent tubes as well as excessive stress, as they are triggers that reactivate the symptoms characteristic of the condition.
Diagnostic criteria: Systemic lupus erythematosus (SLE)
In each patient, lupus manifests itself in very different ways, very different clinical profiles can be observed that change over time, so the symptoms can be very varied from one individual to another.
It is important to listen to our body and visit the doctor when there is any discomfort and even more so: perform health check-ups or "medical check-ups" periodically, the definitive diagnosis of lupus is often established until months or years later, giving rise to the disease and its complications progress, on the other hand, timely intervention with a multidisciplinary team of health professionals and proper management of the condition, augur good control of symptoms and a better quality of life for the person, as happens with many chronic non-communicable diseases (ECNT).
ACR: 11 Diagnostic Criteria
The American College of Rheumatology (ACR) indicates criteria that serve as a guide to establish the diagnosis of lupus, at least four of them must be manifested to frame the clinical picture:
- Photosensitivity: the patient manifests great sensitivity to ultraviolet (UV) light from sunlight and other artificial sources such as fluorescent lamps, it can cause fatigue, fever, skin rashes, joint pain and in other areas of the body, exposure to these sources can exacerbate lupus symptoms.
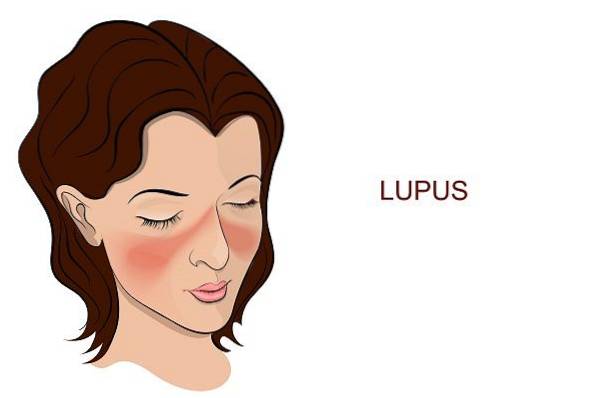
- Malar rash or discoid rash: The first is a butterfly-shaped rash on the cheeks and nose. The second refers to circular lesions or well-defined erythematous scaly patches.
- Mouth or nasal ulcers.
- Serositis: there is inflammation of the serous tissues of the body that surround the lungs (pleura), heart (pericardium), and the inner layer of the abdomen (peritoneum) and internal organs.
- Antinuclear Antibodies (ANA): Non-drug-induced blood test positive.
- Arthritis: Many people with lupus will develop some type of arthritis, so the primary care doctor is usually a rheumatologist.
- Cardiopulmonary problems: Lupus patients may have a predisposition to develop pneumonia, heart problems and pleurisy among others.
- Hematologic disorder: such as anemia.
- Kidney disorder: increased protein or accumulations of red cells in the urine. More than 50% of lupus patients suffer from them.
- Neurological disorders: seizures, psychosis, nerve paralysis and embolisms mainly. When the patient manifests myelitis, care should be taken as soon as possible to avoid paralysis and major complications that often have no turning back.
- Immune disorder
People with lupus can form cholesterol plaques faster than a normal person, show inflammation of blood vessels, and are at higher risk of developing atherosclerosis. Certain neurological dysfunctions can complicate the patient's condition, such as antiphospholipid antibody syndrome (APS), an autoimmune disorder related to lupus, where antibodies mistakenly attack phospholipids, causing blood clots to form in arteries and veins. of the body, which hinders blood flow and damages certain organs of the body.
Other common symptoms are: fever, headache and alopecia, likewise, between 50 and 90% of lupus patients associate fatigue as one of their main symptoms; Fatigue can become chronic, added to other annoying manifestations of the condition, it affects the ability to function in the different areas in which the individual operates.

Lupus is symbolized by the butterfly, because the characteristic malar eruptions resemble a mask of this brightly colored winged lepidopteran. With these symptoms as varied as the colors of butterflies, we can imagine how lupus affects the life of the patient, forcing him to undergo a "metamorphosis" that can involve great emotional suffering, sometimes this process is necessary for the individual to continue with its optimal development; If you suffer from lupus by using adaptive coping strategies and transcending the challenges of your life condition, you can transform yourself into a more beautiful and freer being than you were before despite your condition.
Prevalence of systemic lupus erythematosus (SLE)
Approximately it is estimated that there are between 20 to 150 cases of lupus per 100 thousand inhabitants, more than 5 million people worldwide, it occurs more frequently among women of childbearing age, from 15 to 44 years old mainly, it is estimated that nine out of ten adults with the disease are female and one in 10 lupus patients are men. It currently has a low mortality rate, as advances in science and treatments have improved the quality of life of the patient and there may be good symptomatic control.
Since a large part of the patients with SLE are women, it should be mentioned that the pregnancy of the woman with lupus is considered high risk, so it is necessary that the recommendations of the treating physician be faithfully followed to reduce the impact on the neonate and prevent complications.
Lupus can also be accompanied by fibromyalgia. Many people who suffer from it tend to manifest inflammation and joint pain, it is estimated that patients with rheumatic diseases are three times more susceptible to depressive symptoms than a person who does not suffer from this type of illness, psychological treatments have been shown to provide substantial benefits in the patients who specifically suffer from rheumatic diseases (Lami, Martínez & Sánchez, 2013).
The psychological mechanisms of pain can favor the appearance of depression, the Yates, Morley, Eccleston and Williams (2005) Quality Estimation Scale is an instrument that allows quantitatively evaluating the methodological quality of psychological studies in the field of pain.
Types of lupus
- Systemic lupus erythematosus (SLE): it is very complex because, as its name indicates, it affects several systems and many parts of the body, it is the most representative and frequent type of lupus among the global population..
- Neonatal lupus: is when an infant acquires autoantibodies from his mother with SLE, they can also cross the placenta. Congenital heart block represents the most serious complication, when this is the case, the baby requires the placement of a pacemaker. Symptoms other than this tend to disappear after 6 months.
- Discoid lupus erythomatous (LED): the skin of the lupus patient tends to show high photosensitivity, this type of lupus affects the skin, especially in regions exposed to sunlight and ultraviolet (UV) rays. Red spots occur on both cheeks and the bridge of the nose, giving the shape of a butterfly with open wings.
- Cutaneous lupus erythematosus (CEL) produces sores on parts of the body that are exposed to the sun. The spots can also appear on other parts of the body. It has subtypes according to its chronicity.
- Drug-induced lupus erythomatous (LEIF): has symptoms similar to systemic lupus erimatrosus (SLE), however they disappear after stopping the medications that cause the condition and the recommended treatment.
Treatment for lupus patient
They are focused on strengthening the immune system, seeking hormonal balance, trying to prevent or reduce damage to organs and joints, as well as reducing inflammation and pain.
"Ozone (O3) is a very noble gas that can help to successfully treat the symptomatological manifestations of lupus without causing harmful effects on health, ozone therapy has proven to be highly effective and helps to improve the patient's quality of life".
Lupus can be confusing, as it presents asymptomatic periods, but despite the fact that the patient does not manifest the annoying symptoms of the condition, it is necessary to continue with their treatment, many are focused on ensuring a certain balance in the patient, even at the hormonal level.
The traditional orthodox treatment uses several drugs such as: immunosuppressants, specific BLyS inhibitors, non-steroidal anti-inflammatory drugs (NSAIDs), antimalarials such as hydroxychloroquine and mainly corticosteroids. The intervention of different specialists is often required, depending on the manifestations of the condition they present, generally the primary care physician is a rheumatologist.
Psychology, metamorphosis and healing path for lupus patient
It is true that many times the disease can be cruel, there are days that seem more difficult and longer than others, also that there is no cure for this disease, it can only be tried to control it through treatment, it is natural that the patient experiences uncertainty, fear, anxiety, frustration and sadness, sometimes feeling tired from struggling, through psychological help the perception of somatic symptoms can improve (Navarrete, Peralta, Sabio, Coín et al., 2010), it is possible to influence psychological factors to try greater well-being and achieve a feeling of self-efficacy in the management of the disease by the patient (Mazzoni et al., 2016).
Meszaros, Perl and Faraone (2012) point out that among the patients with lupus more than: 80% had cognitive dysfunction, 39% had depression and 24% had high levels of anxiety; the body image and sexual life of the lupus patient is also often seriously affected (Daleboudt, Broadbent, McQueen & Kaptein, 2013; Jolly et al., 2012).
With lupus, it is necessary to face uncertainty, anxiety, and develop great patience, as well as tolerance for frustration, bearing in mind that many times, no matter how much medical indications are followed, the disease has its own course, sometimes its Progress implies great discomfort for the person, both in physical and psychosocial aspects, forcing the patient to change their rhythm of life. Psychotherapeutic treatment can help reduce the "impression of disease damage".
Monique Vander Elst, psychiatrist and psychotherapist, talks about "mourning for good health", sometimes it is necessary to abandon the illusion that we can control certain things, she says that when we do not let go of that need for control, "it is more likely that a picture appears depressant". It is true that ECNT like lupus can totally transform your life, but it is necessary to embrace the acceptance of the condition, make “peace” with ourselves, in order to continue our development and “tune in” to that new rhythm that life imposed on us..
It is normal to experience fears about the future, especially when you are not sure how the disease will progress over time, but it is not convenient to promote catastrophic thoughts that generate more anxiety and discomfort. It is common for people with lupus to often have feelings of guilt and shame for not being able to do what they were used to, so it is convenient to "let go" the need for control and develop patience ... A lot of patience.
One more challenge is presented when couples, friends and family do not accept the person with their new life condition, when there is lack of support, criticism, abuse and humiliation, you should know that many times this happens out of ignorance, having Unrealistic expectations leads to great disappointments, do not hurt yourself more generating resentment ... Lupus can become a very misunderstood disease, since the genesis of its name it has been stigmatized by the appearance of its symptoms.
Perhaps in a certain part of the "metaphormosis" you will feel desolation, many people you appreciate may be the first to make judgments against you, remember that there is a lot of ignorance about this disease among the population, do not ask others to understand something so complex that you are just beginning to understand yourself. By looking for support groups of people who share your condition, together with the advice of health specialists, you can see yourself greatly benefited and find the understanding you require.
The "lupus" seeking healing steppes
Having periods where the symptoms are not very visible makes the disease and the adjustment more confusing, however, you must be honest with yourself, listen to your body and identify how you feel, remember: “you don't have to do things to please others at the cost of your well-being and your health ”, perhaps you need some time alone to recover, sometimes it is not pleasant to receive visitors or leave feeling so terrible, you also have the right to be alone when you need it, the important thing is not to fall into extremes and try to find balance.
Although it is true that sometimes it is necessary and you have the right to withdraw from situations in which you feel uncomfortable due to your health condition, it is a poor adaptation mechanism to constantly use avoidance-flight behaviors, such as resorting to emotional and social isolation This can increase emotional distress in the patient. When depressive symptoms and symptoms of the disease worsen, this can lead to low self-esteem and suicidal ideation..
Suffering from NCD is a burden for the person who suffers it. The lupus patient is affected mainly at home, as well as in the work and academic aspect if he is studying, since many times they do not find support or understanding in those around him, when this is the case, the patient can generate feelings of guilt and shame, as well as having their sense of self-efficacy diminished.
Sometimes fears arise, one of them may be not knowing if the disease will allow you to be self-sufficient because of your condition. The person may experience lack of motivation, affective blunting, outbursts of aggressiveness, self-reproach and even manifest self-destructive behaviors; The constant fight against the disease can be tiring, however difficult it may seem at times, it is necessary to accept that the disease will be a companion for life, but it is not adaptive to let yourself collapse because of it. Many patients live their pain in silence, they feel misunderstood and alone, remember that you do not have to fight your battles alone, psychologists can accompany you on this path of "metamorphosis" and healing..

Leaving many activities and things you enjoyed, certain job opportunities, as well as the execution of plans can be difficult ... When you have lupus, perhaps your heart calls you to go for a walk but your body forces you to stop for reasons that You still cannot understand, because even when you have put everything on your side the symptoms could manifest themselves, what can you do about this? Try to take advantage of that life time, choose the most functional and adaptive coping strategies, those that can bring you relief or even well-being. If going for a walk is not feasible, perhaps reading a book or playing a board game with your family or friends over a delicious cup of tea is feasible..
Many people who suffer from terrible autoimmune and degenerative diseases, as our diseases progress, they are wreaking serious damage in our lives, the functionality and well-being of the person can be affected in various aspects, sometimes it is necessary to "mourn the person what we were ”, accept that there are plans and goals that are no longer viable, given our new condition, that only means that we will have to make certain“ adjustments ”in terms of our expectations and make some pertinent adaptations ... It is possible to build a new version! of yourself!
Through various investigations it has been observed that lupus patients can improve well-being and biopsychosocial adaptation or the "adjustment" of their life condition through: cognitive-behavioral therapy (CBT), mindfulness training, relaxation and breathing, applying the Mindfulness-Based Stress Reduction (MBSR for its acronym in English; Yeganeh and Hajializadeh, 2015) program, benefit from written emotional expression, psychoeducation, as well as group psychotherapy.
In the subjects with SLE who received cognitive behavioral therapy (CBT), improvements were observed in terms of the management of: anxiety, stress, depression, anger, interpersonal relationships, perception of body image, disease management, fatigue and even on the pain management. As can be seen, the use of these tools can help the person to carry out their beautiful transformation, perhaps our NCDs are forcing us to slow down through life, look more “inward”, to take care of ourselves, love and respect our body, perhaps they force us to release loads, to travel free through this life like butterflies, which although they seem to be fragile due to their condition, show great strength when facing the vagaries of time and the conditions that fate puts in front of them.
Nowadays, many people think that when someone expresses their discomfort they are being "negative", remember that regarding your health you have responsibilities and rights. Like every human being you are susceptible to feeling bad, sometimes it is necessary to cry and look through the pain to transcend it.
It is counterproductive to believe that by repeating a thousand times that "you are fine" you will be cured without making the pertinent adjustments in your lifestyle, that is repression and denial of the problem, they represent bad adaptation mechanisms, it is not convenient to repress your emotions, in Change is a good strategy to work on managing them, a statistically significant and clinically relevant change is shown by patients who work with themselves in that beautiful "metamorphosis" of being.
A sign of personal growth is to identify and recognize that we feel bad, it denotes strength to ask for help in an assertive way, there will be times when you may not be able to alone, it is essential to know how to ask for help. The people around you cannot guess your needs, they too may be tired and facing their own challenges. Remember that "you earn more with honey than with gall".
11 Tips for a Lupus Patient
- Stick to medical recommendations, even when you are going through a remission stage, stopping your treatment could involve complications that can be prevented.
- Avoid unprotected exposure to ultraviolet (UV) rays from solar sources and fluorescent lamps.
- Keeping blood pressure under control.
- Carry out treatment for therapeutic objectives "treat to target" with your team of health professionals.
- Ozone therapy to treat and control the manifestation of symptoms without the harmful side effects.
- Work on "letting go" feelings of guilt, shame, and resentment..
- When you generate catastrophic or anxiety-laden thoughts, stop your thinking and practice a relaxation technique of your choice..
- Avoid dysfunctional coping styles, such as isolation, and strengthen your support networks.
- Carry out a therapeutic process of your choice, especially if you are facing a “metamorphosis” and you feel that you cannot do it alone, psychologists can accompany you in that transformation and healing process..
- Manage optimal levels of stress, remember that distress is an identified trigger of lupus symptoms.
- Faced with small changes in your metamorphosis process, training in coping strategies and managing emotions can be very useful in adjusting your life condition..
Links
- https://www.lupusresearch.org/en-espanol/acerca-del-lupus/que-es-el-lupus/#collapse101
- https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0718-48082016000300001
- https://www.lupus.be/spip.php?rubrique57



Yet No Comments