
Cori disease symptoms, causes, treatments

The Cori's disease is a genetic pathology of a metabolic nature that produces an abnormal and pathological accumulation of glycogen (glucose storage) at the liver, muscle and / or heart level.
This pathology, also known as type III glycogenosis or Cori-Forbes disease, is a rare pathology in the general population that has a wide clinical spectrum.
Regarding the characteristic signs and symptoms of Cori disease, the most frequent are related to hypoglycemia, muscle weakness, generalized growth retardation or hepatomegaly..
On the other hand, at the etiological level, this disease is the product of an autosomal recessive genetic alteration, mainly due to a genetic mutation located on chromosome 1, at location 1q21..
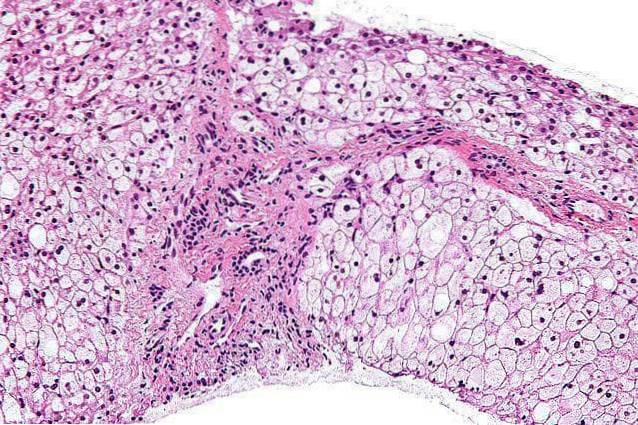
In addition to clinical suspicion, laboratory tests, such as liver biopsy, hymnunohistochemical techniques, among other biochemical tests, are essential in the diagnosis of Cori disease..
Finally, the treatment is based on the control of the medical consequences. The most common is dietary planning to maintain glucose levels in the body.
Type II glycogenesis or Cori's disease was initially described by Sanapper and Van Creveld in 1928. However, it was not until 1956 when Illingworth and his work group described the enzymatic defect that gives rise to this pathology..
Article index
- 1 Features
- 1.1 Glycogen and its functions
- 1.2 Liver
- 1.3 Skeletal muscles
- 2 Causes
- 3 Statistics
- 4 Symptoms
- 4.1 Hypoglycemia
- 4.2 Hyperlipidemia
- 4.3 Muscle hypotonia
- 4.4 Myopathy
- 4.5 Hepatomegaly
- 4.6 Cirrhosis and liver failure
- 4.7 Cardiomyopathy
- 4.8 Stunted growth
- 5 Diagnosis
- 6 Treatment
- 7 References
Characteristics
Cori disease or type III glycogeneosis is a genetic pathology caused by an abnormal accumulation of glucose (sugars) in different organs of the body, through a complex called glycogen.
It is classified within a group of metabolic disorders known collectively as glycogenesis. Although numerous subtypes of glycogenesis have been identified, all of them are due to a disorder in glycogen metabolism.
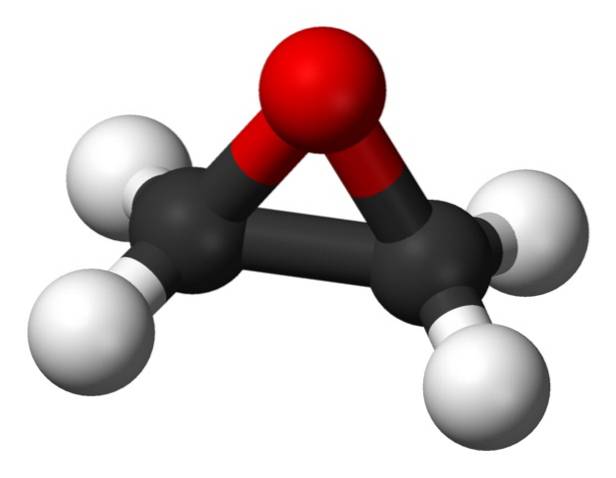
The absence or deficiency of the glucosidated enzyme amyl-1,6 produces an excessive storage of glycogen in the liver, muscles, and in other cases the heart.
Cori disease presents several clinical subtypes (IIIa, IIIb, IIIc and IIId), classified according to specific signs and symptoms:
- Type IIIa and IIIc: mainly affect the liver and muscle structure.
- Type IIIb and IIId: normally only affect liver areas.
Glycogen and its functions
Glycogen is a biochemical compound that is present in our body and whose essential function is the energy reserve. Specifically, it is the way in which glucose is stored in different organs, especially in the muscles and the liver, in addition to other types of glycogen-rich tissues such as cardiac.
In addition, the specific functions of this compound may vary depending on the tissue in which it is located:
Liver
Glucose accesses liver cells through the bloodstream. Thus, after food intake, it is stored in the form of glycogen in different liver areas..
When the level of sugars in the blood is reduced, the stored glycogen releases glucose into the bloodstream and thus the rest of the organs receive the necessary contribution for their efficient functioning.
Skeletal muscles
In the case of the muscular structure, glycogen is used locally to obtain the necessary energy during physical efforts. Therefore, for our body to have the ability to transform glycogen into glucose to obtain energy substrate, it is essential that different enzymes intervene, such as hexicinases.
Thus, in the case of Cori disease, the characteristics of its clinical course are derived from the presence of alterations both in the storage and in the degradation of glycogen, also affecting the enzymes involved in this process.
Causes
Cori disease has a genetic origin, mainly related to different mutations located on chromosome 1, at location 1p21. Genetic alterations will produce a deficient or insufficient activity of the glycogen debranching enzyme.
As a consequence, the affected people will present a marked difficulty to carry out the different biochemical processes of glucose release from glycogen and, therefore, an abnormal accumulation of this and different pathologies related to energy reserves will occur..
In many of the diagnosed cases, it has been possible to identify at least 4 or 5 defective genes related to the clinical characteristics of Cori disease..
Statistics
Cori's disease is a rare genetic pathology, in the case of the United States the prevalence has been estimated at around 1 case per 100,000 people.
Different investigations indicate that it is a disease with a higher frequency in people of Jewish descent, especially in North Africa, reaching approximately 5,400 people..
In addition, in relation to other demographic characteristics, such as sex, a higher frequency associated with the female or male sex has not been identified..
On the other hand, regarding the subtypes of Cori disease, the most common form is IIIa, representing 85% of all cases. This type is usually followed by form IIIb, which represents 15% of those affected by this pathology.
Symptoms
The clinical course of Cori disease is usually variable, depending on the areas that are most affected. However, in most cases they are usually evident during childhood..
Generally, the most common signs and symptoms are related to:
Hypoglycemia
With the term hypoglycemia we refer to the presence of low blood sugar levels, that is, a deficient level of glucose. Normally, the level must be below 70mg / dl to be considered abnormal or pathological.
This medical condition can lead to the development of other complications such as:
- Alteration of the rhythm and heart rate.
- Recurrent headaches.
- Decreased or increased appetite.
- Impaired visual ability, such as blurred or double vision.
- Mood changes: irritability, aggressiveness, anxiety, etc..
- Difficulty getting to sleep.
- Tiredness, weakness, and generalized fatigue.
- Tingling sensations and numbness.
- Heavy sweating.
- Dizziness and loss of consciousness.
Hyperlipidemia
With the term hyperlipidemia we refer to the presence of high levels of lipids, that is, fats in the bloodstream. Normally, it is associated with genetic factors that cause an increase in cholesterol and triglyceride levels in the blood..
At a specific level, this disorder can lead to the development of other types of medical complications, mainly related to:
- Heart complaints, angina pectoris, and other heart-related disorders.
- Stinging and cramping sensation in the lower extremities.
- Problems related to the healing of superficial wounds.
- Symptoms related to strokes: muscle weakness or paralysis, language problems, etc..
Muscle hypotonia
One of the first indicative signs of this pathology is the presence of a marked muscular weakness. Muscle tone is abnormally reduced, thus making it difficult to perform all kinds of activities and motor acts.
Myopathy
The recurrent presence of hypotonia and other alterations related to motor function, leads to the development of myopathies.
With the term myopathy we refer to a wide group of muscular diseases that are characterized by the presence of chronic muscular inflammation and weakness. Therefore, medical complications related to myopathies include:
- Progressive muscle weakness, starting from the proximal structures, that is, the muscles closest to the trunk.
- Tissue damage to muscle fibers.
- Tiredness and fatigue related to motor acts: walking, breathing, swallowing, etc..
- Recurrent muscle pain.
- Increased skin sensitivity.
- Difficulty walking, maintaining posture, speaking, swallowing, etc..
Hepatomegaly
On the one hand, with the term hepatomegaly we refer to the presence of an abnormally large liver. Normally, due to inflammation and / or volumetric increase, the liver tends to invade various areas, reaching the lower areas of the ribs.
Some of the signs and symptoms that hepatomegaly can cause are related to:
- Abdominal pain and bloating.
- Feeling dizzy.
- Recurring nausea and vomiting.
- Jaundice.
- Changes in the color of urine and / or stools.
Cirrhosis and liver failure
Cirrhosis is the term used to refer to the presence of a progressive deterioration of the liver, at a structural and functional level. Specifically, healthy liver tissue becomes scar, preventing blood circulation through its different structures..
In addition to a wide variety of symptoms (nausea, vomiting, weakness, fatigue, persistent abdominal pain, etc.), cirrhosis can lead to the development of significant medical complications:
- Tumor formations.
- Diabetes.
- Hepatic encephalopathy.
- Gallstones.
- Portal hypertension.
- Spenomegaly.
- Jaundice.
- Liver failure.
- Bleeding and bruising.
- Edema and ascites.
Cardiomyopathy
The term cardiomyopathy is used in the medical field to refer to different pathological processes that affect the integrity and functioning of the heart muscle.
Generally, the alterations are related to:
- Poor contraction: the presence of a bad contraction of the heart muscle makes it difficult for blood to flow out of its interior.
- Poor relaxation: the presence of poor relaxation of the heart muscle makes it difficult for blood to enter its interior.
- Poor contraction and relaxation: the presence of abnormalities in both processes hinders the normal and efficient pumping of blood from the heart to other areas and organs of the body.
Stunted growth
The different hepatic, muscular and cardiac symptoms can cause important alterations related to growth.
Normally, affected individuals tend to have a short stature and abnormally reduced growth standards, compared to other people of the same sex and biological age..
Diagnosis
The clinical characteristics of Cori disease are significant during the childhood stage, therefore, in the face of clinical suspicion from the analysis of the medical history and the physical examination, it is essential to perform a metabolic examination.
Through blood examination and biopsy of different tissues, it is necessary to identify the presence of enzyme deficiencies related to glycogen.
Treatment
Although there is no definitive cure for Cori disease, different therapeutic interventions have been designed, some of them described by the Spanish Association of Glucogenesis Patients:
- Treatment of hypoglycemic episodes: increase in carbohydrate dose, nutritional regulation, administration of subcutaneous or venous glucagon, intravenous inclusion of glucose, etc..
- Surgical care: in severe cases of liver cirrhosis, surgical approaches are necessary and, fundamentally, liver transplantation.
- Pharmacotherapy: the administration of drugs is fundamentally related to the treatment of episodes of pain and cardiac alterations.
- Diet care: the regulation of food intake is a fundamental aspect in this and other metabolic diseases. It is necessary to maintain a balanced diet, with a night supply of glucose.
References
- AGSD. (2016). Glycogen Storage Disease Type III. Retrieved from The Associatin for Glucogen Storage Disease UK: https: //www.agsd.org.uk/
- Cosme, A., Montalvo, I., Sánchez, J., Ojeda, E., Torrado, J., Zapata, E.,… Arenas, E. (2005). Type III glycogenosis associated with hepatocellular carcinoma. Gastroenterol Hepatol, 622-5.
- Duke University Health System. (2016). What are the different types of Glycogen Storage Disease? Obtained from Duke Children's.
- FEC. (2016). Cardiomyopathies. Obtained from the Spanish Heart Foundation.
- Froissart, R. (2016). Glycogen storage disease due to glycogen debranching enzyme deficiency. Obtained from Orphanet.
- NORD. (2016). Forbes Disease. Obtained from National Organization for Rare Disorders.
- Tegay, D. (2014). Genetics of Glycogen-Storage Disease Type III. Obtained from Medscape.


Yet No Comments