
Purple disease symptoms, causes, treatment
The purple disease, Also known as idiopathic thrombocytopenic purpura, it is a pathology of autoimmune origin characterized by the presence of a platelet alteration. It is usually classified within hematological disorders.
It is defined clinically by the presence of episodes of mucosal and cutaneous bleeding, menorrhagia, persistent bleeding due to trauma, petechiae, purpura, bruising, gingivorrhagia, ecchymosis, etc..
The origin of thrombocytopenic purpura is found in an autoimmune process that generates various antibodies against platelets and their production at the medullary level. Given the clinical suspicion, it is essential to perform various laboratory tests to confirm the diagnosis: hemogram, blood coagulation analysis, tissue biopsy, bone marrow aspiration, etc..
At present there are various therapeutic approaches for the treatment of purpura disease: plasma exchanges, administration of glucocorticoids, antiplatelet agents, splenectomy, etc..
Article index
- 1 History
- 2 Characteristics of purple disease
- 3 Statistics
- 4 Symptoms
- 4.1 Cutaneous and mucosal bleeding
- 4.2 Ecchymosis
- 4.3 Petechiae
- 4.4 Purple
- 4.5 Gingivoregia
- 4.6 Menorrhagia
- 4.7 Epistaxis
- 4.8 Other complications
- 5 Causes
- 6 Diagnosis
- 7 Treatment
- 8 References
Story
Idiopathic thrombocytopenic purpura was initially described by the German medical specialist Paul Gottlieb Werlhof in the year 1735. Due to this, in the initial moments it was known as Werlhof's disease..
Later, Paul Kznelson in 1916 published the first report in which he referred to a successful therapeutic approach for thrombocytopenic purpura, splenectomy..
As early as 1951, a group of researchers formed by Willaim, Harrington and Holigsworth associated the characteristics of this pathology with a disorder of autoimmune origin..
Characteristics of purple disease
Idopathic thrombocytopenic purpura is an autoimmune disease characterized by the presence of platelet penia, which usually appears during adolescence. It is a pathology whose basic clinical course leads to the development of bruises and bruises, sudden or excessive bleeding, among other signs.
At a specific level, this pathology is defined as a type of thrombocytopenia, that is, an abnormal and pathological decrease in blood platelet levels..
Platelets are cells that are part of our blood material. Its essential function is the formation of clots and the repair of blood vessels that are injured and / or damaged..
These cells are specialized in maintaining the structure and integrity of the blood vessels in our body and, in addition, help prevent and control bleeding through the acceleration of clotting..
In optimal conditions, it is expected that we have platelet levels of 150,000 to 400,000 / mc. However, less than 150,000 can lead to significant medical complications related to bleeding and blood clotting..
Thrombocytopenia or thrombocytopenia can appear due to various factors:
- The bone marrow does not make enough platelets.
- Platelets are destroyed in the bloodstream.
- Platelets are destroyed in organs such as the liver and spleen.
In the case of idiopathic thrombocytopenic purpura, the absence of platelets is associated with the development of pathological autoimmune processes.
Statistics
Statistical analyzes indicate that thrombocytopenic purpura has an incidence of 1 case per 25,600-50,000 inhabitants in the general population each year.
In the United States, the incidence of this pathology is usually around 3.3 cases per 100,000 inhabitants in adulthood each year. For its part, the prevalence reaches 9.5 cases per 100,000 people.
It can affect anyone, although it has a prevalence ratio of 1.3; 1, being more frequent in the female sex. This disease can also appear in any age group, however, it is more common for its initial manifestations to appear in childhood..
Approximately 40% of diagnosed cases correspond to patients less than 10 years of age. The prevalence being very high in the age group from 2 to 4 years.
In the pediatric population, thrombocytopenic purpura has an annual incidence of about 5.3 cases per 100,000 children. In the case of males, two age peaks have been identified. It especially affects those under 18 years of age and the elderly.
Symptoms
Thrombocytopenic purpura is a pathology that is mainly related to clinical manifestations of a hemorrhagic nature.
Although in some cases low platelet levels present as an asymptomatic medical condition, some of the signs and symptoms most associated with idiopathic thrombocytopenic purpura include:
Cutaneous and mucosal bleeding
Recurrent and spontaneous bleeding is one of the cardinal signs of this pathology.
People with idiopathic thrombocytopenic purpura are at serious risk of spontaneous bleeding and bruising. Although it can appear in any area, this symptom is more associated with bleeding from the gums or nose.
Blood material can also be seen in waste, such as urine.
In the most serious cases where the platelet count is minimal, the affected people are at risk of suffering fatal bleeding (gastrointestinal, internal, intracranial bleeding, etc.).
Ecchymosis
In the medical field, ecchymosis is the term that is usually used to refer to the presence of bruises, commonly known as bruises. These lesions are defined as an accumulation of blood material at the skin level..
The etiological causes of bleeding under the skin are widely heterogeneous: injuries and trauma, immune disorders, allergic reactions, medical treatments, skin aging, etc..
They can take various presentations or clinical forms, from defined and localized bruises to large affected skin areas.
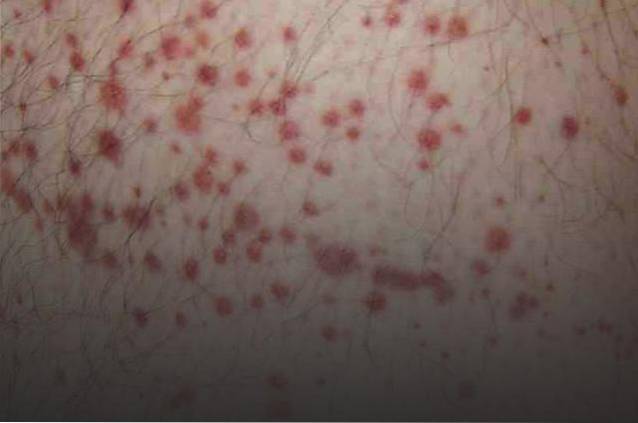
Petechiae
Petechiae are a type of disorder related to subcutaneous bleeding. Visually, they are usually identified as a reddish stain, similar to blood. They usually reach an extension of a few millimeters and on a few occasions of centimeters.
Its appearance is due to the escape of a reduced amount of blood from a capillary or blood vessel located under the superficial layers of the skin..
This type of medical finding, along with others, are usually indicators of serious pathologies. They can indicate a vasculitis, thrombopenia, infectious process, etc..
Purple
It is a skin disorder characterized by the appearance of purple lesions in different locations of the skin or in the mucous areas of the body..
Like the previous ones, they are due to blood leaks under the superficial layers of the skin. It usually has an approximate extension of about 4 to 10 mm.
When the purpura reaches an amplitude greater than 4 mm they are called petechiae and if it exceeds one centimeter it is called ecchymosis.
Gingivorregia
This term is used to refer to bleeding episodes that appear suddenly in the gums, at the oral level.
Although it is usually a very frequent medical condition in those frequent in emergency medical services, on some occasions it can be related to serious pathologies, such as carcinomas.
Menorrhagia
Blood clotting abnormalities and bleeding episodes can also disrupt menstrual cycles. In women affected by idiopathic thrombocytopenic purpura, it is possible to observe menstrual periods defined by heavy and / or long-lasting bleeding.
It is a pathology that requires treatment and medical intervention as it can cause various complications such as anemia or episodes of acute pain.
Epistaxis
Epistaxis is the medical term used to refer to nosebleeds.
Other complications
In addition to the signs and symptoms described above, other more serious manifestations may appear that put the survival of the affected people at risk..
The most common are massive internal bleeding or central nervous system bleeding..
Causes
In most of those affected, thrombocytopenic purpura is associated with autoimmune disorders that cause a destruction of platelets.
Ongoing investigations have not yet been able to identify the etiological cause of this immune process, which is why it is often referred to as an idiopathic disorder.
In other people, the clinical course of thrombocytopenia purpura may be associated with some risk factors:
- Sex: it is a pathology about three times more common in women than in men.
- Infectious processes: Especially in children, an infectious process of viral origin is usually identified prior to the development of purpura. The most common are mumps, measles or respiratory infections.
- Pregnancy: it is possible that due to pregnancy there is a significant decrease in the level of platelets.
Diagnosis
In the face of suspicious clinical signs and symptoms, an analysis of the family and individual medical history and a complete clinical examination is necessary..
Laboratory tests will be essential: hemogram, blood coagulation analysis, tissue biopsy, spinal aspirate, etc..
Treatment
The most common therapeutic approaches in thrombocytopenic purpura include:
- Administration of corticosteroids: some types of corticosteroids such as prednisone can increase platelet levels by suppressing the activity of the immune system.
- Administration of intravenous immunoglobulins: it is used as an emergency treatment in cases of severe bleeding or a surgical procedure to rapidly increase the levels of platelets in the blood.
- Administration of thrombopoietin receptor agonists- some drugs like romiplostmi or eltrombopag help prevent bleeding and bruising.
- Administration of immunuspressants: inhibit the activity of the immune system to increase platelet levels. Some of the most common are rituximab, cyclophosphamine or azathioprine.
- Antibiotics: its use is restricted to cases in which it is possible to identify an etiological cause associated with infectious processes.
- Surgery: In some patients, specialists recommend removal of the spleen to improve symptoms or increase the platelet count..
References
- Donahue, M. (2016). Idiopathic Thrombocytopenic Purpura (ITP). Obtained from HealthLine.
- EBMT. (2016). Immune Thrombocytopenia. EBMT.
- Godeau, B. (2009). Immune thrombocytopenic purpura. Obtained from Orphanet: Immune thrombocytopenic purpura.
- ITP Foundation. (2016). What is ITP? Obtained from ITP Foundation.
- Martin Arnau, B., Turrado Rodriguez, V., Tartaglia, E., Bollo Rodríguez, J., Tarragona, E., & Trias Folch, M. (2016). Impact of preoperative platelet count . Cir. Esp.
- Mayo Clinic. (2016). Idiopathic thrombocytopenic purpura (ITP). Obtained from Mayo Clinic.
- NORD. (2016). Immune Thrombocytopenia. Obtained from National Organization for Rare Disorders.
- Raynard Ortiz, M., Jamart, V., Cabray, C., Borras, R., & Mailan, J. (2009). Anesthetic management in pregnant women affected by idiopathic thrombocytopenic purpura. Rev. Esp. Anestesiol. Reanim.
- Ruiz-Martínez, M., Sanchez-Jiménez, P., Bonilla-Aguilar, I., Martínez Müller, R., González-Fernández, G., & Martínez-Clemente, I. (2006). Care plan for a patient with idiopathic thrombocytopenic purpura. Nursing.
- UMMC. (2016). Idiopathic thrombocytopenic purpura. Obtained from University of Maryland Medical Center.



Yet No Comments