
Entamoeba histolytica morphology, life cycle, symptoms

Entamoeba histolytica it is a parasitic microorganism of the intestine in humans. It can parasitize canids and other vertebrates. It is the causative agent of amoebic dysentery or amoebiasis.
It is an anaerobic organism that can live as a commensal in the large intestine or invade the mucosa causing significant lesions. From the intestine it can infect extrainstestinal liver, lung and even brain tissues. Pathogenic and non-pathogenic strains can exist.
Amoebic dysentery is one of the parasitic diseases with the highest morbidity and mortality in humans in tropical countries. It is considered the third leading cause of death after malaria and schistosomiasis.
Factors such as inadequate faecal waste management systems, potable water supply and inadequate food handling, contribute to the existence of endemic areas in the world..
Article index
- 1 Biological characteristics of Entamoeba histolytica
- 2 Morphology
- 3 Life cycle
- 3.1 E. histolitica has a direct or monoxenic life cycle, that is, it requires a single host for its development. It does not present biological vectors in its life cycle.
- 3.2 It can, however, provide mechanical vectors, such as mouse flies that do not actively participate in their cycle, but only transport infective forms to food and water..
- 3.3 Infection occurs after ingestion of tetra nucleated cysts in contaminated food and water. Because the action of gastric juices digests the cyst wall.
- 3.4 The cysts rupture giving way to the formation of trophozoites. These multiply by binary fission and invade the mucosa of the large intestine, especially the colon, which is the main habitat for their active development..
- 3.5 Some trophozoites can invade the intestinal wall, destroying epithelial cells. They produce lectins that allow them to adhere to intestinal cells and lysis through proteinases. From the intestine they can invade extraintestinal tissues, reaching invade liver, lung and brain tissues.
- 4 Symptoms
- 5 Diagnosis
- 6 Treatment
- 7 Control and prevention
- 8 References
Biological characteristics of Entamoeba histolytica
E. histolytica It presents two parasitic forms: the cyst and the trophozoites. The cyst is the infective form, it does not have locomotion and is resistant in the external environment; trophozoites represent the vegetative form, being mobile and active.
E. histolytica feeds by phagocytosis, that is, it emits pseudopods with which it introduces the small particles that make up its food into its cellular content where it is digested.
The trophozoite and cyst phases are present in its development. Trophozoites are the mobile, amoeboid form. The cyst is the non-active form, resistant to adverse conditions.
Morphology
E. histolytica is morphologically indistinguishable from commensal amoebae E. dispar Y E. moshkovskii. It can be distinguished from E. coli, another species present in humans, because the latter does not emit pseudopods.
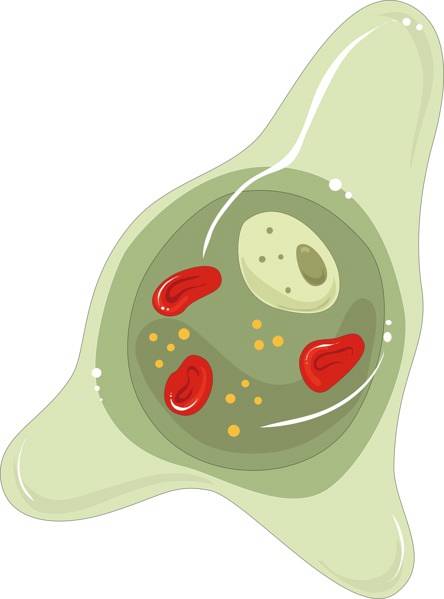
The trophozoite has a central mass called the endoplasm and an outer layer known as the ectoplasm. They have a nucleus with a central karyosome and peripheral chromatin distributed in a regular way.
It has an anterior end that can form pseudopodia and a posterior end that presents a bulb or uroid with a tuft of filopodia for the accumulation of debris. Presents a system consisting of a network of digestive vacuoles and ribosomes.
Trophozoites can be in two forms: magna and minuta. The magna form measures 20 to 30 microns and can emit thick pseudopodia; minute shape measures 19-20 microns and can emit shorter pseudopods.
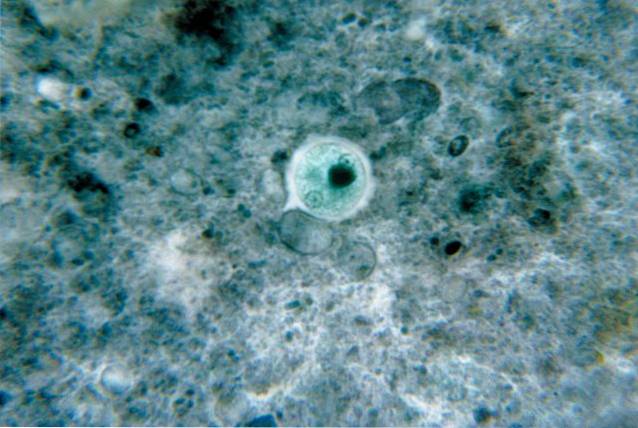
Cysts are round or spherical in shape. Under the microscope they show refractive, it can be seen that the membrane contains one to four nuclei depending on maturity.
Metacysts have a thinner membrane. The nuclei are rod-shaped with rounded ends and glycogen vacuoles. In the cytoplasm you can see the chromatidal bodies, which are glycogen inclusions in the cytoplasm.
Lifecycle
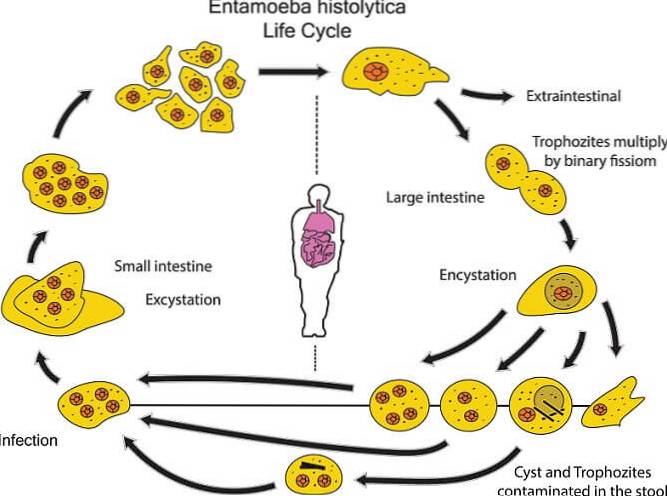
E. histolitica It has a direct or monoxenic life cycle, that is, it requires a single host for its development. It does not present biological vectors in its life cycle.
It can, however, provide mechanical vectors, such as mouse flies that do not actively participate in their cycle, but only transport infective forms to food and water..
Infection occurs after ingestion of tetra nucleated cysts in contaminated food and water. Because the action of gastric juices digests the cyst wall.
The cysts rupture giving way to the formation of trophozoites. These multiply by binary fission and invade the mucosa of the large intestine, especially the colon, which is the main habitat for their active development..
Some trophozoites can invade the intestinal wall, destroying epithelial cells. They produce lectins that allow them to adhere to intestinal cells and lysis through proteinases. From the intestine they can invade extraintestinal tissues, reaching invade liver, lung and brain tissues.
In the large intestine, uninucleated precysts originate, which progressively transform into mature or tetranucleated cysts, which are the infecting forms of the parasite..
The contaminated person excretes both cysts and trophozoites through their feces, which contaminate water and food. With the ingestion of contaminated food a new host begins.
Symptoms
The parasitized person may remain asymptomatic, or present mild or severe symptoms. Mild cases are the most common, representing 90% of them.
Mild symptomatic cases show nausea, diarrhea, weight loss, fever, and abdominal pain. In chronic cases, colic may occur, including ulcers and the presence of blood in the stool..
When extra-intestinal invasion occurs, the most common condition is liver abscess, which causes fever and pain in the upper abdomen..
Diagnosis
Diagnosis is made by examining stool under a light microscope. In the samples, forms of the parasite are identified, in cases positive to amoebiasis. Serial examinations with a minimum of three samples analyzed on successive days are recommended.
The use of PCR or serology with specific antibodies are also useful techniques in diagnosis..
In extraintestinal cases the diagnosis can be made by CT images.
Mucus and blood may occur in the stool depending on the severity of the infection.
Treatment
Metronidazole, paromomycin, and tinidazole delivery have been used. In cases of extraintestinal invasion, such as liver abscesses, surgery has been a technique used.
It is recommended to verify the diagnosis well to avoid false identifications due to the presence of species such as E. dispar Y E. moshkovskii. The misapplication of commonly used drugs leads to the formation of resistant strains.
Control and prevention
In the world, health strategies are focused on the application of measures that seek to interrupt the biological cycle of the parasite, through the participation of the different social actors involved..
In this, the conscious participation of the communities is very important, mainly in areas of epidemiological risk. Among others we can mention:
- Education of the population about amebiasis, its life cycle and the risks of contagion
- Maintenance of adequate sanitary systems for the deposition and treatment of feces.
- Maintenance of adequate supply systems and access to drinking water.
- Availability of infrastructure and accessibility for the population to diagnostic services and care for affected people.
References
- Chacín-Bonilla, L. (2013). Amebiasis: clinical, therapeutic and diagnostic aspects of the infection. Medical Journal of Chile, 141 (5): 609-615.
- Diamond, L.S. & Clark, C.G. (1993). A redescription of Entamoeba histolytica Schaudinn, 1903 (emended Walker, 1911) separating it from Entamoeba dispar Brumpt, 1925. Journal of Eukaryotic Microbiology, 40: 340-344.
- Elsheikha, H.M., Regan, C.S. & Clark, C.G. (2018). Novel Entamoeba Findings in Nonhuman Primates. Trends in Parasitology, 34 (4): 283-294.
- Gómez, J.C., Cortés J.A., Cuervo, S.I. &, López, M.C. (2007). Intestinal amebiasis. Infectio, 11 (1): 36-45.
- Showler, A. & Boggild, A. (2013). Entamoeba histolytica. Canadian Medical Association Journal, 185 (12): 1064.



Yet No Comments