
Temporal lobe epilepsy symptoms, causes, treatment

The temporal lobe epilepsy It is a type of epilepsy that originates in the temporal lobes of the brain, important areas in memory, language, and emotional processing. When seizures occur, disturbances in these functions may appear.
Some of the manifestations of this type of epilepsy are strange feelings such as fear or euphoria, déjà vu, hallucinations or dissociation. After a crisis, memory problems can appear, and even aphasia.
This type of epilepsy is one of the most frequent and, at the same time, complex. It seems to cover 40% of all epilepsy cases, although these figures seem to vary in different studies.
The term "temporal lobe epilepsy" was officially established in 1985 by the International League Against Epilepsy (ILAE). It was used to define a condition that stands out for the appearance of recurrent seizures originating from the medial or lateral temporal lobe. However, it was already mentioned by the neurologist John Hughlings Jackson in 1881.
Article index
- 1 Features
- 2 Prevalence of temporal lobe epilepsy
- 3 Causes
- 3.1 Hippocampal sclerosis
- 3.2 Injuries, infections or heart attacks
- 3.3 Others
- 4 Symptoms
- 4.1 Auras
- 4.2 Autonomic symptoms
- 4.3 Psychic symptoms
- 4.4 Symptoms in loss of consciousness
- 4.5 After the epileptic seizure
- 5 Types of temporal lobe epilepsy
- 5.1 Medial temporal lobe epilepsy
- 5.2 Neocortical temporal lobe epilepsy
- 6 Diagnosis
- 7 Treatment
- 7.1 Antiepileptic drugs
- 7.2 Vagus nerve stimulation
- 7.3 Surgical intervention
- 8 Patient prognosis
- 9 References
Characteristics
Temporal lobe epilepsy is a type of partial epilepsy, that is, it affects a specific area of the brain (as opposed to generalized epilepsy, which involves the brain as a whole).
Associated seizures can be simple partial, in which the person is conscious; or complex partials when there is a loss of consciousness.
Generally, the birth, delivery, and development of people with temporal lobe epilepsy is normal. It usually appears at the end of the first decade of life or the beginning of the second, after an early brain injury or fever.
Most patients respond to treatment with the appropriate antiepileptic drugs. However, about a third of patients do not improve with these drugs, and they may experience memory and mood disturbances..
For these cases, surgical intervention accompanied by neuropsychological rehabilitation may be useful..
Prevalence of temporal lobe epilepsy
According to Téllez Zenteno and Ladino (2013), there are few data on the incidence of this type of epilepsy. According to a study published in 1975, temporal lobe epilepsy appears in 1.7 per 1000 people.
Among patients with partial type epilepsy (involving only a limited area of the brain), between 60% and 80% have temporal lobe epilepsy.
Regarding population studies, in one published in 1992 it was observed that it affected 27% of patients with epilepsy. While, in another, they indicated a prevalence of 66% of epilepsies.
No differences have been found between men and women regarding the frequency of this type of epilepsy, although it is known that epileptic seizures are more likely when women are menstruating.
Causes
In some cases of epilepsy, the lesions can be identified with magnetic resonance imaging or histopathological studies. However, in other cases, no observable abnormality may be identified, making diagnosis and treatment difficult..
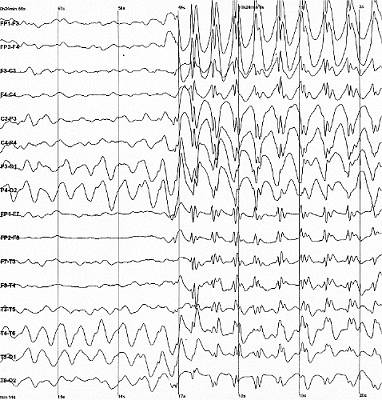
What happens in the brain when an epileptic seizure occurs? It seems that, during the sleep and wake cycles, the electrical activity of the cells of our brain varies.
When the electrical activity of a group of neurons is altered, an epileptic seizure can appear. In temporal lobe epilepsy, this abnormal activity is found in one of the temporal lobes.

Temporal lobe epilepsy can be familial or have a sporadic onset. The causes seem to be mainly:
Hippocampal sclerosis
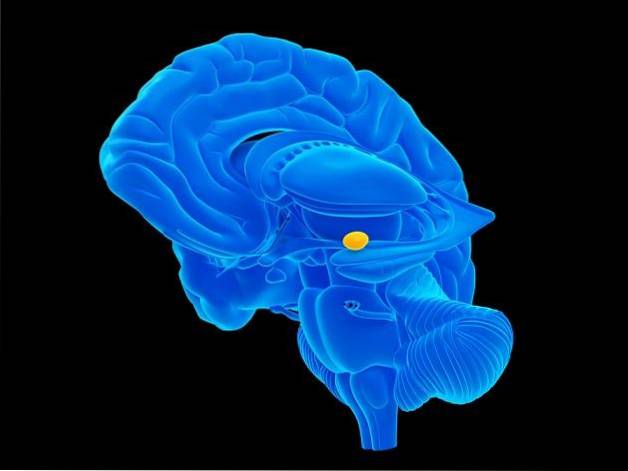
It is the loss of a certain group of neurons in the hippocampus, a very important area located in the temporal lobe. Specifically, they occur in neuronal nuclei called CA4, CA3 and CA1.
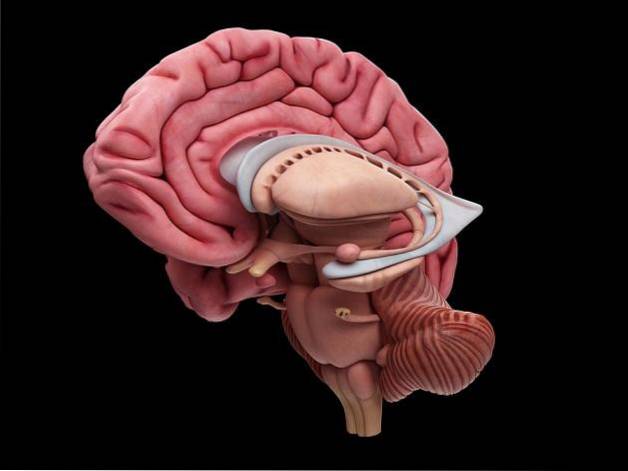
How does this loss occur? Apparently, it could be due to a genetic predisposition, or perinatal hypoxia (lack of oxygen in the brain that occurs during birth). That would cause an injury to the hippocampus that facilitates febrile crises in childhood.
Also in some research it has been suggested that it could be due to a poor development of the hippocampus together with some subsequent injury (infection or trauma).
Injuries, infections, or heart attacks
Traumatic brain injuries in childhood, infections such as meningitis or encephalitis, strokes, or genetic syndromes can facilitate the onset of epilepsy..
The most common risk factor is having had a seizure caused by a high fever in the past. In fact, two thirds of patients with this type of epilepsy have had febrile seizures without infection before the onset of seizures.
These crises are characterized by being longer than normal, about 15 minutes or more. They are also distinguished by causing obvious neurological abnormalities such as strange positions or weakness in any limb.
Other
- Low-grade brain tumors affecting the temporal lobe.
- Congenital malformations of the blood vessels of the brain.
- Glyotic lesions, that is, those that cause scarring or gliosis of the hippocampus.
Symptoms
The most common symptoms of temporal lobe epilepsy are auras and memory deficits..
Auras
Auras appear in 80% of temporal lobe seizures. They consist of strange sensations that function as an alarm, indicating the onset of a seizure..
The aura is a partial or focal attack that does not impair the patient's consciousness, and has different manifestations. For example, perceiving smells, tastes, experiencing visual hallucinations or perceptual illusions. The sensation of vertigo is also included in this group.
Patients can see the objects around them smaller than normal (micropsia) or magnified (macropsia), or, perceive distortions in the shape and distance of the elements in the environment.
Olfactory auras appear to be indicative of a possible temporal lobe tumor.
Autonomic symptoms
Such as changes in heart rate, goose bumps, or increased sweating. Gastrointestinal complaints or "butterflies in the stomach" are also common..
Psychic symptoms
Like déjà vu (feeling that you have already experienced the same situation), or jamais vu (the opposite, that is, you do not recognize something you have already experienced).
In addition to depersonalization (being detached from oneself), a feeling of unreality, or a sudden appearance of fear or anxiety. These last two symptoms are associated with seizures derived from the cerebral amygdala.
There are cases in which some patients have observed their own body from the outside, as if they had “come out” of it..
Symptoms in loss of consciousness
On the other hand, when the epileptic seizures associated with the temporal lobe are complex (with loss of consciousness) they can last from 30 seconds to 2 minutes. The symptoms that may appear are:
- Dilated pupils and gaze.
- Inability to respond to stimuli.
- Repeated chewing or swallowing, as well as lip smacking.
- Strange and repetitive movements of the fingers.
These symptoms can evolve into generalized tonic-clonic seizures. They are the most typical of epilepsy, and are characterized by strong body rigidity followed by uncontrolled rhythmic movements.
After the epileptic seizure
After experiencing a temporal lobe seizure, symptoms such as:
- Confusion and trouble speaking.
- Amnesia, that is, trouble remembering what happened during the crisis. The patient may not know what has happened and may not be aware that they have had an attack.
- Excessive drowsiness.
Types of temporal lobe epilepsy
There are two main types of temporal lobe epilepsy
Medial temporal lobe epilepsy
It is the one that involves the medial or internal structures of the temporal lobe and is the most common subtype. In fact, they account for 80% of all temporal lobe epilepsies..
It normally affects the hippocampus or the structures that are close to it. It is usually caused by hippocampal sclerosis, and it is resistant to drugs.
Neocortical temporal lobe epilepsy
It is the one that covers the outermost part of the temporal lobe. They are associated with complex hallucinations such as music, voices or screams and with alterations in language.
Diagnosis
Professionals can make an approximate diagnosis through the symptoms that patients describe.
However, to make a reliable and accurate diagnosis, magnetic resonance imaging (MRI) brain examinations are used to observe if there are abnormalities that may be associated with temporal lobe epilepsy..
It is also essential to perform an EEG, which measures the electrical activity of the brain. Thanks to this, it will be possible to detect where the altered electrical activity is located.
Treatment
Antiepileptic drugs
The vast majority of patients (between 47 and 60%) who present with focal seizures in the temporal lobe respond to treatment with antiepileptic drugs.
Some of the newer and less secondary symptoms and interactions with other substances are: oxcarbazepine, gabapentin, topiramate, pregabalin, vigabatrin, etc..
It is important to note that pregnant women cannot take this type of medication as it increases the risk of malformations in the fetus. However, there are patients who do not respond to this type of medication and who may manifest memory problems, and a significant deterioration in the quality of life.
In addition, it can also happen that the side effects of these drugs are too bothersome. Some of the most common are dizziness, fatigue, or weight gain..
Vagus nerve stimulation
An alternative to drugs and surgery is vagus nerve stimulation, which is valid for patients older than 12 years. It involves implanting a stimulator device in the chest, placing an electrode on the left vagus nerve in the neck..
This device, with a high-frequency pacing rate, appears to produce a 25-28% reduction in seizures during the first 3 months. This percentage increases to 40% each year that takes.
As secondary symptoms, cough, hoarseness, paresthesia, dysphagia (swallowing difficulties) or dyspnea (breathing problems) may appear; but only if the device is switched on.
Interestingly, the exact mechanism by which vagus nerve stimulation exerts this effect is unknown..
Surgical intervention
Surgical methods may be chosen if the epilepsy is severe, does not resolve with any other treatment and the brain region causing the problem is well located.
Currently, if the cause is hippocampal sclerosis, this can be detected with MRI and resolved by surgery. The electroencephalogram would also denote altered electrical activity in that area.
There are two types of surgical intervention depending on the location of the origin of the epilepsy: anterior temporal lobectomy and tonsil hypocampectomy..
After this type of intervention, it has been found that 70% of the patients have been seizure-free, without significant subsequent complications. Even in a study in which they performed tonsil hypocampectomies, the percentage of good results was 92%.
Patient prognosis
Compared with the general population, patients with temporal lobe epilepsy have higher levels of morbidity and mortality. This may be linked to the higher accident rate these individuals have when entering a crisis and losing consciousness..
On the other hand, these patients have a 50 times greater risk of suffering sudden death, due to “sudden unexpected death in epilepsy”. A risk factor for this is the presence of generalized tonic-clonic seizures..
However, with surgery, this risk of death would decrease, making mortality comparable to that of the general population. A good indicator of improvement in the patient is the absence of epileptic seizures 2 years after the surgical intervention is performed..
Patients with temporal lobe epilepsy can also suffer from memory and mood problems (affective disorders, suicidal tendencies ...). This hinders their quality of life, many patients choosing to isolate themselves.
Therefore, it is important that patients with epilepsy attend neuropsychological clinics. Thus, it would be sought to maintain the cognitive abilities, emotions and functionality of the person in their day to day as much as possible.
References
- Acharya, V., Acharya, J., & Lüders, H. (1998). Olfactory epileptic auras. Neurology, 51 (1), 56-61.
- Cornejo Ochoa, J.W. and Toro Pérez, M.E. (2011). Epilepsies of the temporal lobe. Cuban League Against Epilepsy.
- Téllez-Zenteno, J. F., & Ladino, L. D. (2013). Temporary epilepsy: clinical, diagnostic and treatment aspects. Rev Neurol, 56 (4), 229-242.
- Temporal Lobe Epilepsy. (s.f.). Retrieved on December 30, 2016, from the Epilepsy Foundation: epilepsy.com.
- Temporal Lobe Epilepsy. (April 29, 2014). Retrieved from Medscape: emedicine.medscape.com.
- Temporary lobe seizure. (June 25, 2014). Retrieved from MayoClinic: mayoclinic.org.



Yet No Comments