
Clinical record characteristics, components, importance, example

The medical records It is a legal and confidential document in which the data of a patient are recorded, data necessary to establish diagnoses, prescribe medical treatment and plan nursing care if necessary.
In some health centers and depending on the countries, the clinical record is considered equivalent to the patient's medical record. When they are considered different, the file includes the medical history.
Proper handling of the information included in said file gives legal protection to the patient, the health professionals involved in patient care, and the institution. It is very useful to support teaching programs, for clinical and statistical studies, among others..
The clinical record is the history of the state of health of a patient, it is a written instrument that contains antecedents, paraclinical examinations, laboratory tests, diagnoses, prognoses, treatments, responses of the patient to said treatments.
The data necessary for the health team are recorded in it. Includes all progress notes, interconsultations, references, episodes of hospitalization, surgeries, etc., that is, it contains a chronological record of the patient's health status.
The clinical file is generally opened when the patient goes to a medical institution, public or private, to request some type of medical attention. In some countries that have public care services, regulations are established to record and organize medical records..
In some health institutions, for external consultations, the medical file is not opened on the day of the consultation but on the days prior to the consultation, so that all the patient's personal data can be obtained and the number of identification to the file. Currently many institutions use digitized records.
Article index
- 1 Characteristics of the clinical record
- 2 Components
- 2.1 Clinical history
- 3 Importance
- 4 Example of clinical record
- 5 References
Characteristics of the clinical record
It is a confidential document, the information contained therein must be handled with discretion and in accordance with the codes of medical deontology. The clinical record belongs to the institution or to the provider of the medical service. However, the patient has rights to the information for the protection of their health.
All medical records must contain accurate patient identification information. All the note sheets or reports of the file must be identified with the name of the patient, the date and time of each procedure and the full name and autograph or digital signature of the person who prepared it..
It must be a true reflection of the course of the patient's illness and its data cannot be altered or falsified. The language must be precise, technical and, as far as possible, it must not include abbreviations or acronyms, it must have legible handwriting without amendments or studs and be kept in good condition.
In certain countries there are regulations for the management of clinical records and public and private institutions are obliged to keep clinical records for a minimum period of five years after the last registered consultation..
In summary, the general characteristics of the clinical record can be listed:
-Well identified.
-Confidential.
-Insurance (Only authorized health personnel will have access).
-Available (when required).
-Untransferable.
-Readable.
-Truthful.
-It must have accuracy and precision in its contents.
-Be prepared with technical rigor.
-Full.
-It must include the Identity of all practitioners or health personnel involved in patient care and medical management. Full name, handwritten or digital signature and Professional ID.
Components (edit)

-Front sheet: data for the identification of the health center, including the type, name and address. Name, sex, age and address of the patient's room and other data that may be necessary, especially those required by health regulations.
-Complete medical history.
-Evolution Notes.
-Laboratory and cabinet results.
-Registration form.
-In case of hospitalization: admission note, progress notes and discharge note, initial emergency note if the patient has been admitted by the emergency service, observation notes, pre-operative notes and post-operative notes, if applicable.
-Reference note and / or transfer.
-Consultations and referrals.
-Social worksheets.
Other documents: informed consent. Nursing sheet. Medical indication sheet.
Medical history
The clinical history must be filled out by the treating physician and consists of:
-Interrogation: identification card, family history and hereditary conditions, pathological personal history (including addictions, if any), and non-pathological, illness or any current illness (including smoking, drinking alcohol and others) and interrogation by body systems and devices.
-Physical exploration. You must have at least: habits (sportsmen, sedentary, etc.), vital signs (pulse, body temperature, blood pressure, heart rate and respiratory rate), data of the head, neck, chest, abdomen, limbs (upper and lower) and genitalia.
-Results of previous and current studies.
-Treatments or therapies previously used and their results.
-Diagnostics.
-Treatment and medical indications; in the case of drugs, indicating at least: dose, route and periodicity.
-Evolution notes, which must be written by the attending physician at each outpatient consultation.
Importance
The clinical record is the document that is prepared as a result of the doctor-patient interview, as well as the log of each hospitalized patient. Each file stores the ordered clinical data, of each clinical case that arrives at the hospital or of each patient who enters an office. It is the basis for assistance, teaching and research in medicine.
It is not just another role in the institutional bureaucracy, or a mere administrative procedure, the importance of the clinical file transcends the doctor-patient relationship. For the patient, having a file means trust, it also denotes that attention is paid to him.
For the treating physician, it is the database that provides elements for diagnosis and treatment, includes data for study programs, research or treatment for specific cases.
For the physician-in-training, the clinical record is his valuable learning tool. In clinical sessions, the record is the fundamental axis that relates theory to practice
For the nurse, the clinical record is an instrument of communication with the treating physicians, it includes the observations and the result of continuous surveillance that are usually decisive for therapeutic management.
It is the database of clinical research, allows computing morbidity and mortality data and implementing epidemiological surveillance and health education systems, among others..
If the clinical record is electronic, several advantages are obtained, such as storage space. The information is immediately available, both for the treating physician and for any consultation of authorized personnel. In addition, orders to pharmacy, laboratory and medical examinations can be issued immediately in the interconnected systems.
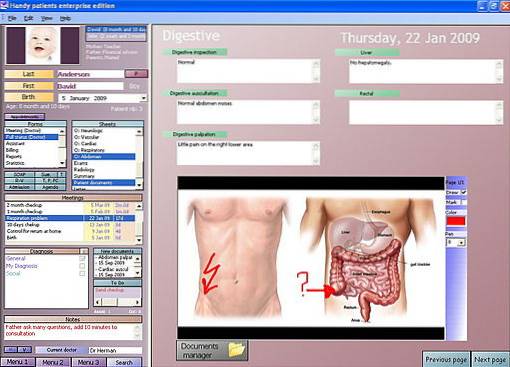
Example of clinical record
Below is an example of a format of part of an electronic medical record developed by the company “Handy Patients Enterprise”, of Swiss origin and implemented in many European and American countries.
References
- Edwards, J. C., Brannan, J. R., Burgess, L., Plauche, W. C., & Marier, R. L. (1987). Case presentation format and clinical reasoning: a strategy for teaching medical students. Medical teacher, 9(3), 285-292.
- Kurtz, S., Silverman, J., Benson, J., & Draper, J. (2003). Marrying content and process in clinical method teaching: enhancing the Calgary-Cambridge guides. Academic Medicine, 78(8), 802-809.
- Manual of the electronic clinical record, M. D. E. C. (2011). General Directorate of Health Information. Ministry of Health, Mexico.
- Merino Casas, M. J., Ruiz Zavala, J. H., Romero, A. D., Martínez Franco, A. I., Martínez González, A. A., Varela, T. V.,… & Jurado Núñez, A. G. (2016). Perception of the Usefulness of the Electronic Medical Record in a National Institute of Health. CONAMED Magazine, twenty-one(4).
- Spitzer, R. L., Williams, J. B., Gibbon, M., & First, M. B. (1992). The structured clinical interview for DSM-III-R (SCID): I: history, rationale, and description. Archives of general psychiatry, 49(8), 624-629.
- Varela, D. E. (2017). Perception of patients and officials on the implementation of the electronic medical record of the Ministry of Health of Panama.
- Waitzkin, H. (1984). Doctor-patient communication: clinical implications of social scientific research. Jama, 252(17), 2441-2446.



Yet No Comments