
Formation of urine processes involved

The urine formation is the term that synthesizes and illustrates the complex set of processes carried out by the renal parenchyma in fulfilling its functions and thereby contributing to the maintenance of body homeostasis.
The concept of homeostasis includes the conservation, within certain limits and through a dynamic balance, of the values of a series of physiological variables that are essential for the preservation of life and the harmonious, efficient and interdependent development of vital processes..
The kidney participates in homeostasis by preserving the volume and composition of body fluids, which includes hydroelectrolyte, acid-base and osmolar balances, as well as the disposal of end products of endogenous metabolism and exogenous substances that enter.
To do this, the kidney must eliminate excess water and deposit in it the excess of those useful and normal components of body fluids, and all of the foreign substances and waste products of metabolism. That is the formation of urine.
Processes involved
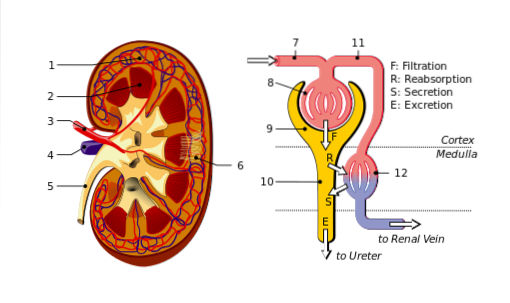
Kidney function involves processing the blood to extract the water and solutes that must be excreted from it. For this, the kidney must have an adequate blood supply through its vascular system and must process it along a specialized system of tubules called nephrons..
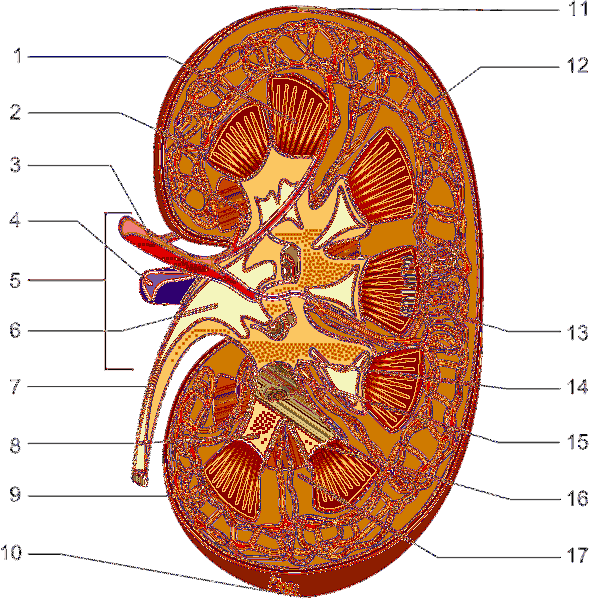
A nephron, of which there are a million per kidney, begins in a glomerulus and continues with a tubule that joins, along with others, to some channels called collectors, which are structures where kidney function ends and that lead to the minor calyces, (urinary tract start).

Urine is the final result of three kidney processes that operate on the blood plasma and that end with the excretion of a volume of liquid in which all the waste substances are dissolved..
These processes are: (1) glomerular filtration, (2) tubular reabsorption, and (3) tubular secretion..
- Glomerular filtration
Renal function begins in the glomeruli. In them, the processing of the blood begins, facilitated by the close contact between the blood capillaries and the initial sector of the nephrons..
Urine formation begins when part of the plasma leaks into the glomeruli and passes into the tubules..
Glomerular filtration is a pressure-driven mechanical process. This filtrate is plasma with its substances in solution, except for proteins. It is also called primary urine, and as it circulates through the tubules it is transformed and acquiring the characteristics of the final urine.
Some variables are related to this process. The FSR is the volume of blood that flows through the kidneys per minute (1100 ml / min); the RPF is the renal plasma flow per minute (670 ml / min) and the GFR is the volume of plasma that is filtered in the glomeruli per minute (125 ml / min).
Just as the volume of plasma that is filtered is considered, the amounts of the substances in that filtrate must be considered. The filtered charge (CF) of a substance “X” is the mass of it that is filtered per unit of time. It is calculated by multiplying the VFG by the plasma concentration of substance "X".
The magnitude of filtration and kidney work is better appreciated if instead of considering the values in terms of minutes we do it in terms of days.
Thus, the daily GFR is 180 l / day in which the filtered loads of many substances go, for example 2.5 kg / day of sodium chloride (salt, NaCl) and 1 kg / day of glucose.
- Tubular reabsorption
If the filtrate at the level of the glomeruli remained in the tubules until the end of its journey, it would end up being eliminated as urine. Which is absurd and impossible to sustain since it would imply losing, among other things, 180 liters of water, one kilogram of glucose and 2.5 kilograms of salt.
One of the great tasks of the kidney therefore involves bringing most of the water and filtered substances back into circulation, and leaving in the tubules, to eliminate as urine, only a minimum liquid volume and the amounts to be excreted of the different substances.
The reabsorption processes involve the participation of epithelial transport systems that carry the filtered substances from the lumen of the tubules to the liquid that surrounds them, so that from there they return to the circulation again entering the surrounding capillaries..
The magnitude of the reabsorption is normally very high for water and for those substances that must be conserved. Water is 99% reabsorbed; glucose and amino acids in their entirety; Na, Cl and bicarbonate 99%; urea must be excreted and 50% is reabsorbed.
Many of the reabsorption processes are adjustable and can increase or decrease in intensity, with which the kidney has mechanisms to modify the composition of the urine, regulate the excretion of filtered products and maintain its values within normal limits.
- Tubular discharge
Tubular secretion is a set of processes by which the renal tubules extract substances from the blood found in the peritubular capillary network (around the tubules), and pour them into the previously filtered tubular fluid.
This adds additional substance to the filtrate and improves excretion..
Important secretions are those of H +, ammonium and bicarbonate, which contribute to the preservation of the acid-base balance, and those of many endogenous or exogenous substances whose presence is not well seen in the body and must be eliminated.
The regulation of many of the secretion processes, by varying their intensity, also varies in the same sense the excretion of the substances involved..
- Final urine
The fluid that enters the smaller calyces from the final portion of the collecting tubes (papillary ducts) no longer undergoes further modifications, and is conducted from there as urine and along the ureters to the urinary bladder, where it is stored until elimination. end through the urethra.
This urine is produced daily in a volume (between 0.5 and 2 liters per day) and with an osmolar composition (between 1200 and 100 mosmol / l) that depend on the daily intake of fluids and solutes. It is normally transparent and light amber in color..
The concentration of each of the substances that compose it is the result of the relative proportions in which each of them was subjected to the previously mentioned filtration, reabsorption and secretion processes..
References
- Ganong, W. F. (2003). Renal function and micturition. Review of Medical Physiology. 21st ed. New York, NY: Lange Medical Books / McGraw Hill, 702-732.
- Guyton, A. C., & Hall, J. E. (2016). The Urinary System: Functional Anatomy and Urine Formation by The Kidneys. Guyton, AC, and Hall, JE, Textbook of Medical Physiology, 13th ed., Elsevier Saunders Inc., Philadelphia, 325.
- Heckmann, M., Lang, F., & Schmidt, R. F. (Eds.). (2010). Physiologie des Menschen: mit Pathophysiologie. Springer.
- Klinke, R., Pape, H. C., Kurtz, A., & Silbernagl, S. (2009). Physiology. Georg Thieme Verlag.
- Vander, A. J., Sherman, J. H., & Luciano, D. S. (1998). Human physiology: the mechanisms of body function (No. 612 V228h). New York, US: McGraw-Hill, 1990.



Yet No Comments