
Fournier's Gangrene Symptoms, Types, Causes, Treatments
The Fournier gangrene It is an intense and destructive soft tissue infection that involves the perineal and genital areas. The rapid progression of the infection and its ability to affect various tissues to produce necrosis, is the main characteristic of this pathology. The extension to the abdomen or thighs is possible due to the intensity of the picture.
This gangrene is considered a type of necrotizing fasciitis, a bacterial infection that progresses rapidly and invades deep planes - even the fascia that covers the muscles - until it destroys them. The rapid progression of the infection and a high risk of mortality make it a medical emergency..
This infection is named after the doctor who first described it. In 1883 the French venereologist Jean-Alfred Fournier observed the presence of necrotizing fasciitis in the genitalia of young men. The finding was very rare, being attributed to the simultaneous action of several bacterial agents.
The causes of this pathology are diverse and depend on the association of several factors. Age, immunosuppression, and chronic diseases such as diabetes are some predisposing factors for necrotizing fasciitis..
Fournier's gangrene is a very rare condition. It is estimated that its prevalence is 0.02% with respect to other pathologies. It is more common in men and the age group most affected are the elderly, from 60 years of age. Trauma and immunosuppression conditions are determining factors for its appearance in young people.
Article index
- 1 Symptoms
- 1.1 General symptoms
- 1.2 Symptom stages
- 2 Kinds
- 3 Causes
- 3.1 Predisposing factors
- 3.2 Direct causes
- 4 Treatment
- 4.1 Stabilize the patient
- 4.2 Infection control
- 4.3 Surgery
- 5 References
Symptoms
The most significant clinical characteristic of Fournier's gangrene is the rapid evolution and aggressiveness of the disease. Initially it presents as an infectious perineal soft tissue picture. Subsequently, the progression is rapid, presenting tissue death -or necrosis- in a short period of time.
Localized pain is a symptom present from the beginning of the disease. Symptoms and associated clinical signs are malaise, fever, and local swelling with redness, edema, and heat. Pain intensity is often disproportionate to clinical signs of inflammation.
General symptoms
- Nonspecific discomfort.
- Fever.
- Pain, the initial symptom, which may disappear as necrosis progresses and destroys sensory nerves.
- Inflammation, expressed as edema, redness, and local heat.
- Massive destruction of superficial and deep tissues or gangrene. This is caused by bacterial infection of tissues. One consequence is the obstruction of the small-caliber arteries - obliterative endarteritis - which increases tissue necrosis..
- Signs of shock The infection can become generalized, producing hypotension, tachycardia, oliguria, dehydration, neurological alteration and coma..
Symptom stages
- A few days earlier, nonspecific symptoms such as weakness, mild, diffuse pain, and fever may occur. These initial symptoms provide no indication of the infection causing them..
- Increased sensitivity in the perineal, genital, or perianal region is followed shortly by severe pain. The first signs of inflammation and edema appear on the skin, associated with the painful condition. Burning and itching may occur in the affected area.
- In a matter of hours or a few days, the local inflammation and pain become more intense. Response to initial treatment with analgesics and antibiotics is poor.
- Appearance of the first trophic changes in skin. It turns dark and lackluster. Crackling may be felt to the touch, due to the accumulation of gases under the epidermis. Rubbing on the skin makes it come off easily, due to epidermolysis. Pain may go away due to tissue death.
- Establishment of gangrene. The first signs of tissue destruction are followed by devitalized areas, with the presence of abscesses or purulent discharge. The infection spreads under the skin to subcutaneous cellular tissue, muscle fascia, and even muscle. Tissue necrosis due to bacterial activity produces a characteristic foul odor.
- The depth that the infection reaches can cause the passage of germs into the bloodstream. In this case, bacteremia and sepsis occur. Septic shock is a consequence of sepsis and produces hemodynamic instability expressed in tachycardia and hypotension. Shock is the cause of death if infection is not controlled.
Types
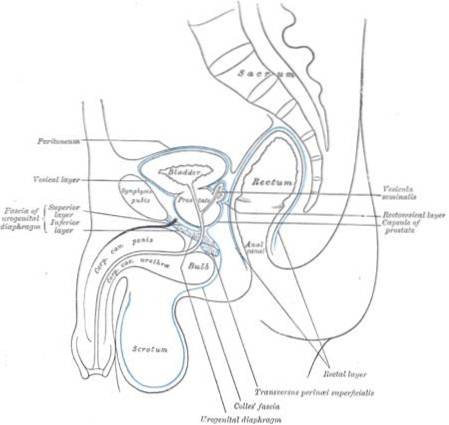
Fournier's gangrene is a form of necrotizing fasciitis that is predominantly located in the perineal area; that is, the space between the genital and anal region.
The perineal fascia or Colles fascia is the most affected; however, it can extend to the fascia of Dartos of the scrotum or to the fascia of Scarpa abdominal.
Although the clinical form may begin at a specific point, it may continue to spread to adjacent areas. The spread of the infection is due to its aggressiveness. According to its point of origin, three types of gangrene can be identified:
- Perineal area or region.
- Urogenital region.
- Perianal or anorectal.
Causes
There is a relationship between the immunological status of the patient and the pathogenicity of the bacteria that cause the infection. An immunosuppressed individual will have a greater susceptibility and few defenses against bacterial infections. The chances of developing Fournier's gangrene are very high in these cases..
While the causes are the direct mechanisms of infection and gangrene, predisposing factors will contribute to its appearance and development..
Predisposing factors
- Diabetes.
- HIV infection.
- Renal insufficiency.
- Liver failure.
- Long-term steroid treatment.
- Cancer, chemotherapy, or radiation therapy.
- Alcoholism.
- Morbid obesity.
- Advanced age.
- Repeated trauma to the perineal or genital area.
Direct causes
- Anorectal infectious processes: abscesses, fissures, fistulas.
- Genitourinary infections.
- Pyoderma or skin infections, such as cellulitis or abscesses.
- Deep burns in the perineal, anorectal, or genital area.
- Severe trauma to the perineal or genital area.
- Complicated surgeries both in the genito-urinary tract and in the anal or rectal region.
- Cancer in nearby areas.
- Complicated laparotomies.
- Intra-abdominal or pelvic infections.
It is important to bear in mind that in susceptible individuals, any inflammatory or infectious process in the perineal, genital or anal areas can cause Fournier's gangrene..
Treatment
Due to the severity of the clinical picture, immediate action will determine the survival of the patient. The therapeutic management of Fournier's gangrene should be multidisciplinary, depending on the cause. The surgeons will be directly responsible, with the support of internists, intensivists and infectologists.
The severity and rapid progression of the symptoms of this disease warrant treatment following three lines of action: stabilize the patient, control the infection, and perform surgical and reconstructive cleaning..
Stabilize the patient
Treatment will be specifically aimed at compensating the general condition of the patient, especially if he presents sepsis or signs of shock:
- Endovenous hydration.
- Parenteral nutrition.
- Treatment of the underlying disease.
Infection control
The use of combined antibiotics is necessary, due to the presence of various types of bacteria. Triple antibiotic therapy will aim to provide broad antimicrobial coverage to the patient. Although treatment guidelines vary, three types of antibiotics are combined:
- For gram positive germs: piperazilin / tazobactam or ciprofloxacin.
- Coverage against gram negative germs: aminoglycosides such as amikacin.
- Anaerobic germs: clindamycin or metronidazole.
Surgery
Surgical treatment is the most important. This will have the objective of cleaning the affected areas by removing the necrotic tissue.
This procedure may require more than one intervention. In a second stage, the damaged tissue will be repaired to perform anatomical and functional reconstruction..
References
- Country, V.M. (2018). Fournier gangrene. Recovered from emedicine.medscape.com
- Nall, R. (2018). What causes Fournier's gangrene? Recovered from medicalnewstoday.com
- Pendick, D. (2017). Everything you should known about Fournier's gangrene. Recovered from healthline.com
- Cancino, C .; Avendaño, R .; Poblete, C .; Guerra, K. (2010). Fournier's gangrene. Recovered from mingaonline.uach.cl
- Webmd (2017). What is Fournier's gangrene ?. Recovered from webmd.com
- Schulz, S.A. (2017). Necrotizing fasciitis. Recovered from emedicine.medscape.com



Yet No Comments