
Stages glycogenolysis, glucose fate, regulation, diseases

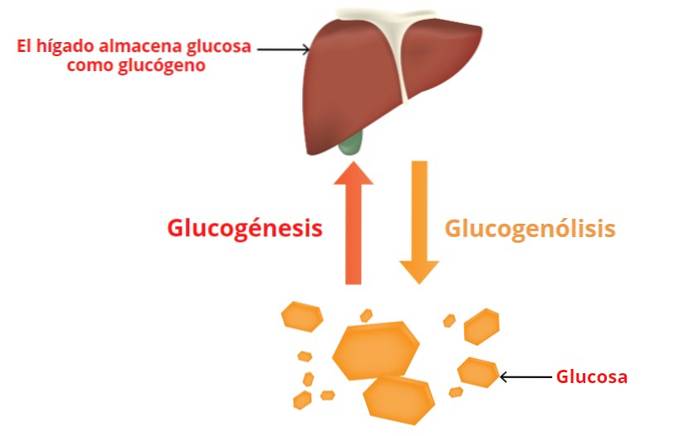
The glycogenolysis It is the process of lysis or breakdown of glycogen. It is a catabolic (destruction) -type enzymatic pathway that involves the breakdown of glycogen and the release of glucose-6-phosphate.
Glycogen is a substance that is used as a store of glucose. It is found in the cytoplasm of cells and is especially abundant in liver and muscle cells of animals..
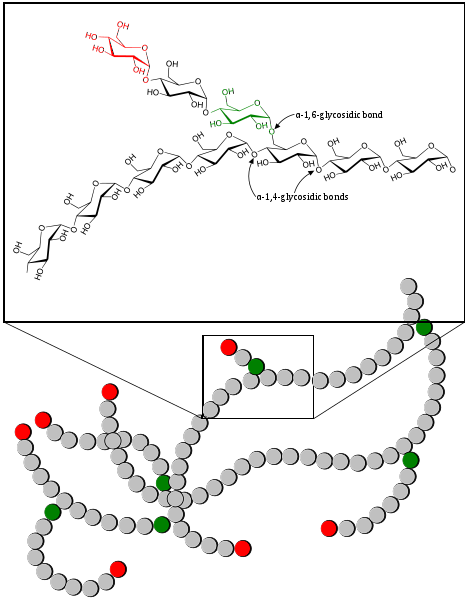
It is a molecule that some authors define as a "glucose tree", since it has a branched structure. It is a homopolymer composed of repeating units of glucose residues, which are joined together through α-1,4 and α-1,6 bonds..
When glucose is needed, it can be obtained from several sources: by glycogenolysis, from glucose circulating in the blood or from the mechanisms of glucose production through non-glycosidic substances. The latter mechanism is called gluconeogenesis and occurs mainly in the liver and kidney..
Article index
- 1 Where does glucose come from and where does it go??
- 2 Stages of glycogenolysis
- 2.1 Phase 1: release of glucose 1-phosphate residues
- 2.2 Phase 2: removing the branches
- 3 Glucose destination
- 4 Regulation
- 4.1 - Regulation of glycogenolysis in the liver
- 4.2 - Regulation of glycogenolysis in muscle
- 5 Diseases related to glycogen storage
- 5.1 Von Gierke's disease
- 5.2 McArdle disease
- 5.3 Hers disease
- 6 References
Where does glucose come from and where is it going??
- Blood glucose comes from the digestive system and the almost exclusive supply processes of the liver.
- When glycogenolysis occurs in the muscle, the released glucose enters the metabolic processes that are aimed at the production of ATP (cellular energy).
- In the liver, glucose from glycogenolysis passes into the blood, concomitantly producing an increase in blood glucose (blood glucose concentration).
Stages of glycogenolysis
Glycogenolysis is a process that cannot be considered as the reverse of glycogen synthesis or glycogenesis, it is a different pathway.
Phase 1: release of glucose 1-phosphate residues
The breakdown of glycogen begins with the action of a specific enzyme called glycogen phosphorylase, which is responsible for "breaking" the α-1,4 bonds of glycogen, releasing glucose 1-phosphate. The mechanism of cleavage is a phosphorolysis.
Thanks to this enzyme, the glycosidic residues of the outermost glycogen chains are split, until there are about four glucose residues on each side of each branch..
In glycogen, glucose molecules are linked by α-1,4 bonds, but at the branching sites the bonds are of the α-1,6 type.
Phase 2: removing the branches
When four glucose residues remain near the branch points, an enzyme, α-1,4 → α-1,4 glucan transferase, transfers a trisaccharide unit from one branch to another, exposing branch point 1 → 6.
The debranching enzyme, specifically amyl 1 → 6 glucosidase, hydrolyzes the α-1,6 bonds. In this way, by the sequential action of these three enzymes (phosphorylase, glucan transferase and debranching enzyme), the complete cleavage of glycogen occurs..
Glucose 1-phosphate from glycogen is transformed into glucose 6-phosphate through a reversible reaction catalyzed by phosphoglucomutase. In this reaction, the phosphate of carbon 1 "changes" to carbon 6 by the effect of this enzyme and this is how glycogenolysis ends..
Glucose destination
In the liver there is an enzyme called glucose 6-phosphatase that removes the phosphate from carbon 6 of glucose and converts it into “free” glucose, which is transported through cell walls and passes into the blood.
The muscle cannot supply glucose to the bloodstream, since it does not have this enzyme and the phosphorylated glucose is "trapped" inside the muscle cells..
Glucose 6-phosphate in muscle enters glycolysis, a catabolic process for the production of ATP (adenosine triphosphate), especially important during anaerobic muscle contraction.
Regulation
Glycogen metabolism is regulated by balancing the activity of two enzymes; one that is used for synthesis, which is glycogen-synthetase and another that is used for cleavage, which is glycogen-phosphorylase.
The balance in the activity of these enzymes will stimulate the synthesis or the breakdown of glycogen. The regulatory mechanisms occur through substrates and through a complex hormonal system that involves, in the liver, at least four hormones:
- the adrenaline
- norepinephrine
- glucagon and
- insulin
- Regulation of glycogenolysis in the liver
Hormones can act through a second messenger, which can be cAMP or calcium ions..
CAMP activates glycogen phosphorylase and, at the same time, inactivates glycogen synthetase. For this reason it increases catabolism and decreases or inhibits glycogen synthesis (anabolism)..
Adrenaline and noradrenaline
Epinephrine and norepinephrine, acting through β-adrenergic receptors, and glucagon, acting through specific receptors, increase cAMP levels in liver cells. This increase in cAMP activates glycogen phosphorylase and glycogen catabolism begins..
Epinephrine and norepinephrine also stimulate glycogenolysis by a mechanism independent of cAMP and through α1-adrenergic receptors. This mechanism stimulates the mobilization of calcium from the mitochondria..
Insulin
Insulin increases the activity of an enzyme called phosphodiesterase, responsible for destroying cAMP. As a consequence of the effect of insulin in the liver, cAMP levels decrease, thus reducing phosphorylase activity and increasing synthetase activity..
The balance of this hormonal activity is what determines the "direction" of glycogen metabolism..
- Regulation of glycogenolysis in muscle

Glycogenolysis in muscle increases immediately after the onset of muscle contraction. Calcium is the intermediate that synchronizes phosphorylase activation with contraction.
Calcium activates a phosphorylase kinase that, in turn, activates muscle glycogen-phosphorylase or myophosphorylase, this enzyme is different from the one found in the liver, but has the same function.
Insulin increases glucose 6-phosphate levels within muscle cells by promoting the entry of glucose from the bloodstream. Increasing glucose 6-phosphate stimulates the dephosphorylation of glycogen-synthetase and its consequent activation.
The net result is an increase in muscle glycogenesis and a decrease or inhibition of glycogenolysis..
Diseases related to glycogen storage
Hereditary insufficiency of some specific enzymes necessary for the hepatic and muscular metabolisms of glycogen is one of the causes of glycogen storage diseases.
These diseases are collectively named glycogenosis. Depending on the enzymatic failure present, they are listed by types I to VIII and are added as they are discovered.
Some glycogenosis are fatal very early in life, here are some examples.
The enzymatic failures present in glycogenosis generate an increase or excessive accumulation of glycogen, mainly in the liver, muscle and / or kidney. However, there are glycogenosis that cause this effect on erythrocytes or lysosomes.
Von Gierke disease
Type I glycogenosis is called Von Gierke disease and is associated with a deficiency of glucose 6-phosphatase, which increases the glycogen load in hepatocytes and renal tubular cells. The patient has hypoglycemia, ketosis, lactacidemia, and hyperlipidemia.
McArdle disease
In type V glycogenosis or McArdle's disease, there is a deficiency of muscle glycogen phosphorylase, which translates into a failure of muscle glycogenolysis. Consequently there is poor exercise tolerance, low blood lactate levels after exercise, and very high glycogen levels within muscle cells..
Hers disease
In type VI glycogenosis or Hers disease, the deficit is in the liver enzyme glycogen phosphorylase. In these cases there is an increase in liver glycogen with a tendency to hypoglycemia.
References
- Blanco, A., & Blanco, G. (2017). Chapter 14-Carbohydrate metabolism. Medical Biochemistry; Blanco, A., Blanco, G., Eds, 283-323.
- Ha, C. E., & Bhagavan, N. V. (2011). Essentials of medical biochemistry: with clinical cases. Academic Press.
- Jones, K. M. (1990). Biochemistry: by J. David Rawn, Neil Patterson Publications, (1105 pages) ISBN 0 89278 405 9.
- Murray, R. K., Granner, D. K., Mayes, P. A., & Rodwell, V. W. (2014). Harper's illustrated biochemistry. Mcgraw-hill.
- Paredes-Flores MA, Mohiuddin SS. Biochemistry, Glycogenolysis. [Updated 2020 Feb 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: ncbi.nlm.nih.gov



Yet No Comments