
Hyperammonemia symptoms, causes, types, treatments

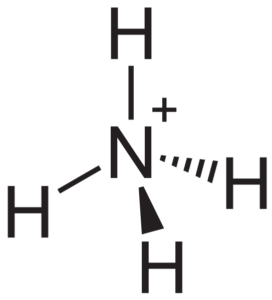
The hyperammonemia is the acute or chronic increase in ammonium ion (NH4 +) or ammonia (NH3) in the blood. It is a very dangerous acquired or congenital metabolic disorder that can result in brain damage and death of the patient.
Ammonium is a nitrogenous substance, a toxic product generated in the catabolism (destruction) of proteins and that is eliminated with its previous conversion into urea, which is less toxic and is eliminated in the urine through the kidney.
For the formation of urea, the metabolic pathway involves the sequential participation of a series of enzymes, some in the mitochondria and others in the cytosol or cytoplasm of liver cells. The process is called the "urea cycle" or "Krebs-Henseleit cycle".
The failure of any of the enzymes involved in the urea cycle results in the increase or accumulation of ammonia in the blood, consequently generating the toxic effects produced by ammonia or ammonia, such as hepatic encephalopathy. In addition, liver failure can affect the urea cycle and cause hyperammonemia..
Under normal conditions the rate of ammonia production and removal is tightly regulated, so that ammonium levels are very low and below toxic ranges. Very small amounts of ammonia in the blood are potentially toxic to the brain.
Article index
- 1 Symptoms of hyperammonemia
- 2 Causes
- 2.1 - Synthesis of urea
- 3 Types
- 4 Treatments
- 5 References
Symptoms of hyperammonemia
The symptoms related to hyperammonemia consist of vomiting, diarrhea, general malaise, refusal to consume protein, loss of appetite (anorexia), drowsiness, lethargy, language disturbances, mood changes, intermittent ataxia, mental retardation and in acute cases severe coma and death.
This symptomatology is independent of the origin of the hyperammonemia. Newborns with these problems of congenital origin can be normal at birth, but the symptoms appear a few days after having ingested food rich in protein (breast milk).
Neonates do not want to eat, vomit, have tachypnea and lethargy that rapidly progresses to a deep coma. In older children, acute hyperammonemia manifests with vomiting, anorexia, and neurological disorders such as irritability, agitation, mental confusion, and ataxia..
These clinical manifestations may alternate with periods of lethargy and drowsiness until they progress to coma and, if left untreated, cause seizures and death..
Causes
The causes of hyperammonemia are due to a failure of urea metabolism, so the urea cycle must be known to understand the pathophysiological mechanisms that generate hyperammonemia.
The urea cycle requires the sequential activation of a series of enzymes. Five enzymes are involved in this process: carbomoylphosphate synthetase, ornithine transcarbamoylase, argininosuccinate synthetase, argininosynthetase, and arginase..
- Synthesis of urea
The initiation of urea synthesis requires ammonia (NH3), carbon dioxide (CO2) provided by bicarbonate and ATP (adenosine triphosphate).
The origin of ammonia derives from the nitrogen of amino acids degraded by transamination and by oxidative deamination. The first two reactions of urea synthesis occur in the mitochondria of liver cells, the other three occur in the cytoplasm.
-CO2 + NH3 + ATP + N-acetylglutamate, by action of the enzyme carbamoyl phosphate synthetase, forms carbamoyl phosphate
-Carbamoyl phosphate + L-ornithine, by action of the enzyme ornithine transcarbamylase, forms L-citrulline
-L-citrulline in the cytoplasm, by action of argininosuccinate synthetase and with L-aspartate as substrate, forms argininosuccinate.
-Argininosuccinate, due to the effect of argininosynthetase, releases fumarate and produces L-arginine.
-L-arginine, together with a water molecule and by the effect of arginase, releases a urea molecule and produces L-ornithine, which will be available to re-enter the second reaction of the cycle within the mitochondria.
The glutamine synthetase is an enzyme that fixes ammonia in the form of glutamine. As the tissues constantly produce ammonia, it is rapidly removed by the liver, which converts it into glutamate, then into glutamine, and then into urea..
Any deficit in any of the enzymes involved in the urea cycle will cause a retrograde accumulation of the missing reaction substrates and a consequent accumulation of ammonia..
Intestinal bacteria also produce ammonia and this passes into the bloodstream and from there to the liver, where it enters the urea cycle..
In patients with liver cirrhosis, certain anastomoses can form in the portal system, which allow part of the ammonia from the digestive system to pass directly into the general circulation without first passing through the liver, being one of the causes of hyperammonemia in addition to insufficiency liver.
Types
Because urea synthesis converts toxic ammonia to urea, defects in urea synthesis lead to hyperammonemia and ammonia poisoning. These poisonings are more severe when the defect occurs in the first two steps of the urea metabolic cycle..
Hyperammonemias are classified into several types according to the corresponding enzyme failure. These types of hyperammonemias are called congenital or hereditary. In addition, there are hyperammonemias that are grouped as "secondary", where another pathology is capable of altering the metabolism of urea.
The primary or congenital are:
- Type I: due to deficiency of cabamoyl phosphate synthetase I
- Type II: due to ornithine transcarbamoylase deficiency. It is an inherited disorder linked to the X chromosome that is accompanied by high levels of glutamine in blood, cerebrospinal fluid and urine.
- Citrullinemia: a recessive inherited disease due to lack of activity of argininosuccinate synthetase.
- Argininosuccinic aciduria: It is inherited in a recessive way and is characterized by an increase of argininosuccinate in blood, cerebrospinal fluid and urine. There is a deficiency of argininosuccinase. The disease has a late onset after two years and causes death at an early age.
- Hyperargininemia: characterized by low levels of erythrocyte argininase and accumulation of arginine in blood and cerebrospinal fluid.
Secondary hyperammonemias are mainly due to liver failure that slows or reduces urea metabolism, so ammonia accumulates and hyperammonemia occurs..
Treatments
Acute hyperammonemia must be treated quickly in order to reduce ammonia levels and prevent brain damage. Calories, adequate fluids, and minimal but sufficient amounts of amino acids must be provided to avoid destruction of endogenous proteins..
It is supplied intravenously with electrolytes, fluids and lipids as sources of calories and minimal amounts of preferably essential amino acids. By slightly improving the general condition of the patient, feeding by nasogastric tube can be administered, especially when it comes to infants..
As ammonia is not easily eliminated by the kidney, the goal of treatment is to generate compounds that have a high renal clearance (clearance). To form these conjugated compounds that are eliminated by the kidney, sodium benzoate or phenylacetate can be administered..
In some cases, the use of arginine promotes the formation of urea, as long as the patient does not have an arginase deficiency. Arginine supplements the urea cycle with ornithine and N-acetylglutamate.
Patients, then, should be on diets with restricted protein intake, which should be provided in small portions..
References
- Behrman, R., Kliegman, R., & Arwin, A. (2009). Nelson Textbook of Pediatrics 16 ed. W.
- Carrillo Esper, R., Iriondo, M. F. N., & García, R. S. (2008). Ammonium and hyperammonemia. Its clinical significance. South Medical, fifteen(3), 209-213.
- Fauci, A. S., Kasper, D. L., Hauser, S. L., Jameson, J. L., & Loscalzo, J. (2012). Harrison's principles of internal medicine (Vol. 2012). D. L. Longo (Ed.). New York: Mcgraw-hill
- Mathews, C. K., Van Holde, K. E., & Ahern, K. G. (2000). Biochemistry, ed. San Francisco: BenjaminlCummings.
- McCance, K. L., & Huether, S. E. (2018). Pathophysiology-Ebook: the biologic basis for disease in adults and children. Elsevier Health Sciences.
- Murray, R. K., Granner, D. K., Mayes, P. A., & Rodwell, V. W. (2014). Harper's illustrated biochemistry. Mcgraw-hill.

Yet No Comments