
Hyperchloremia symptoms, causes, values, treatment
The hyperchloremia It is defined as the increase in chlorine levels in the blood. It is a rare condition and is associated with metabolic acidosis or hypernatremia, that is, increased sodium in the blood.
There are no specific symptoms associated with hyperchloremia. The symptoms, like the alteration in chloride levels, is usually secondary to other pathological processes, so its treatment is based on the management of the underlying pathologies that originate the disorder..
Chlorine is the most abundant anion in the extracellular fluid and contributes to the electro-neutrality of this compartment, compensating for most of the positive charges provided by the sodium ion..
Chlorine transport is generally passive and follows active sodium transport, such that increases or decreases in sodium cause proportional changes in chlorine.
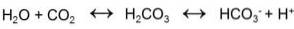
Since bicarbonate is the other important anion in extracellular fluid, chlorine concentration tends to vary inversely with bicarbonate concentration. If bicarbonate goes down, chlorine goes up and vice versa.
Therefore, the increases in plasma sodium that occur with losses of pure water, or with increased sodium intake, are always accompanied by hyperchloremia and the symptoms will depend on the primary cause..
Likewise, alterations in the acid-base balance that occur with a decrease in plasma bicarbonate are accompanied by hyperchloremia, since this anion compensates for the loss of negative charges. The symptoms, in these cases, will be related to the acid-base imbalance.
Article index
- 1 Symptoms
- 1.1 Hyperchloremia associated with hypernatremia
- 1.2 Hyperchloremia associated with metabolic acidosis
- 2 Causes
- 2.1 Metabolic acidosis and hyperchloremia
- 2.2 Hypernatremia and hyperchloremia
- 3 Values
- 4 Treatment
- 5 References
Symptoms
As mentioned above, the symptoms of hyperchloremia are associated with the primary cause of origin. For this reason, we will describe the symptoms related to these causes..
Hyperchloremia associated with hypernatremia
Hyperchloremia associated with hypernatremia can occur by two pathophysiological mechanisms: by loss of pure water or by increased sodium intake.
When there is an excess or deficit of sodium with respect to water, a combination of hormonal, renal and neural mechanisms act synergistically to control the balance. When this balance is insufficient, or fails, a change occurs in the concentration of sodium and concomitantly of chlorine..
If sodium increases or the volume of pure water decreases, a plasma hyperosmolarity occurs that draws water from the cells into the plasma and causes cellular dehydration.
The redistribution of water and cellular and tissue dehydration can lead to seizures and pulmonary edema, which would represent the most severe symptoms.
Hypernatremia and hyperchloremia due to water loss are also associated with fever, dry skin and mucous membranes, thirst, hypotension, tachycardia, low jugular venous pressure, and nervous restlessness..
Hyperchloremia associated with metabolic acidosis
The clinical manifestations of metabolic acidosis involve the neurological, respiratory, cardiovascular, and gastrointestinal systems. Headache and lethargy are early symptoms that can progress to coma in severe acidosis..
In cases of respiratory compensation, breathing becomes rapid and deep, a phenomenon known as the Kussmaul respiration. Other common symptoms include anorexia, nausea, vomiting, diarrhea, and gastrointestinal upset..
Severe acidosis can compromise ventricular function and generate arrhythmias that can be life-threatening..
Causes
The causes of hyperchloremia are related to acid-base and water-electrolyte imbalances, specifically metabolic acidosis and hypernatremia..
Metabolic acidosis and hyperchloremia
Metabolic acidosis is a nosological entity characterized by a decrease in pH due to the accumulation of acidic substances not related to carbonic acid. It can also be related to a decrease in bicarbonate in the extracellular fluid.
This can occur rapidly in lactic acidosis due to circulatory deficit, or more slowly in kidney failure or diabetic ketoacidosis. When changes in blood pH occur, buffer systems try to compensate for the change to keep the pH close to normal..
Respiratory compensation in metabolic acidosis increases CO2 output and thereby reduces blood bicarbonate levels. The kidneys, in turn, can remove excess acid (when the failure is not renal), such as NH4 + and H2PO4-.
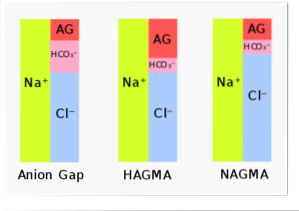
Bicarbonate is part of the balance in plasma between cations and anions. Anion and cation concentrations in plasma are normally equivalent. To measure this relationship, what is known as “anion gap"Or" anion gap ".
The "anion gap”Relates the difference in the summed plasma concentrations of Na + and K + and the summed concentrations of HCO3- and Cl-. In metabolic acidosis, the loss of bicarbonate generates a retention of chlorine to compensate for the loss of anions..
Anion gap = ([Na +] + [K +]) - ([HCO3-] + [Cl-])
This is what causes the hyperchloremia that accompanies metabolic acidosis and is called hyperchloraemic metabolic acidosis..
Hypernatremia and hyperchloremia
In the case of hypernatremia, as already mentioned above, chlorine passively follows sodium in such a way that, when sodium rises (as in hypernatremia), chlorine also rises, causing hyperchloremia..
Hypernatremias can be caused by water loss or by increased sodium intake. The increase in sodium intake may be orally or due to failures in the management of the intravenous supply of hypertonic solutions..
The most frequent causes of increased sodium due to water loss and concomitant increase in chlorine are related to respiratory infections and fever, which increase the respiratory rate and the loss of water through this route..
Diabetes insipidus due to failure of antidiuretic hormone production, diabetes mellitus, polyuria, profuse sweating, and diarrhea cause water losses relative to sodium.
Values
The range of normal values for chlorine in extracellular fluid is between 96 and 105 mEq / L. Values above 110 mEq / L are considered elevated and are referred to as hyperchloremia..
Normal plasma values for sodium are 136 to 145 mEq / L, those for blood bicarbonate are around 24 mEq / L, and plasma potassium is around 3.8 to 5 mEq / L..
Treatment
Treatment consists of treating the primary cause. If the problem is water loss, the cause of the loss should be treated and the lost water replaced.
In the case of acidosis, treatment consists of restoring the acid-base balance and treating the triggering cause; with this, the chlorine will fall back to its normal values.
References
- McCance, K. L., & Huether, S. E. (2002). Pathophysiology-Book: The Biologic Basis for Disease in Adults and Children. Elsevier Health Sciences.
- Hauser, S., Longo, D. L., Jameson, J. L., Kasper, D. L., & Loscalzo, J. (Eds.). (2012). Harrison's principles of internal medicine. McGraw-Hill Companies, Incorporated.
- Ganong WF: Central Regulation of Visceral Function, in Review of Medical Physiology, 25th ed. New York, McGraw-Hill Education, 2016.
- Boniatti, M. M., Cardoso, P. R., Castilho, R. K., & Vieira, S. R. (2011). Is hyperchloremia associated with mortality in critically ill patients? A prospective cohort study. Journal of critical care, 26(2), 175-179.
- Schreiner, G. E., Smith, L. H., & Kyle, L. H. (1953). Renal hyperchloremic acidosis: familial occurrence of nephrocalcinosis with hyperchloremia and low serum bicarbonate. The American journal of medicine, fifteen(1), 122-129.
- Suetrong, B., Pisitsak, C., Boyd, J. H., Russell, J. A., & Walley, K. R. (2016). Hyperchloremia and moderate increase in serum chloride are associated with acute kidney injury in severe sepsis and septic shock patients.. Critical Care, twenty(1), 315.



Yet No Comments