
Maternal Fetal Isoimmunization Pathophysiology, Treatment

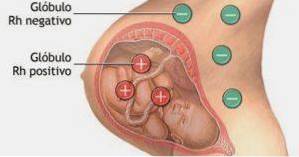
The maternal fetal isoimmunization It is the pathophysiological process of pregnancy that consists of the maternal production of antibodies towards the fetus -which is considered an antigen- with an RH factor different from that of the mother, being previously sensitized.
This last characteristic is very important, since it generates the difference between the terms of isoimmunization and incompatibility. It will depend solely on the blood incompatibility between mother and father: if the father is homozygous for the D antigen with respect to the mother, 100% of the children will inherit said antigen from the father.
If, on the other hand, the father is heterozygous with respect to the D antigen absent in the mother, the probability of the children inheriting these antigens is 50%. It is a severe maternal-fetal incompatibility, which mainly affects fetal viability.
Article index
- 1 Difference between isoimmunization and incompatibility
- 2 Pathophysiology
- 3 Diagnosis
- 4 Complications
- 5 Treatment
- 6 References
Difference between isoimmunization and incompatibility
Incompatibility refers to the antigen-antibody response produced between the mother and the fetus when the hemotypes are different: for example, mother A, father B; or Rh- mother, Rh + father, but without passage of red blood cells into the maternal circulation, that is, without sensitization.
On the other hand, in isoimmunization there is already a contact between the different non-compatible hemotypes, which produces a sensitization in the mother and, therefore, memory antibodies (IgG) are formed in response to the antigen present in the red blood cells of the fetus. mainly the D antigen.
When there is incompatibility in a first pregnancy, the mother can be sensitized. For this reason, in incompatibility, hemolytic disease of the newborn is rarely established, only in 0.42% of cases..
This is because in the first pregnancy, acute phase IgM antibodies are formed, which due to their high molecular weight do not cross the placental membrane..
Only 1 ml of fetal blood is required to pass through the placental membrane to initiate an immune response. Lower amounts can boost secondary immunity.
Once the woman is sensitized, the maternal immune system is capable of producing large amounts of anti-Rh antibody to small amounts of fetal blood..
Pathophysiology
Maternal isoimmunization to fetal red blood cell membrane factors or antigens results in a condition called hemolytic disease of the newborn.
This isoimmunization occurs mainly by two mechanisms of antigenic stimulation: incompatible blood injection or transfusion and heterospecific pregnancy. There may also be isoimmunization in the case of organ transplants.
Isoimmunization can occur at the time of delivery, with the performance of amniocentesis and even in the case of abortions of incompatible products.
10% of mothers can be isoimmunized after the first pregnancy, 30% after the second and 50% after the third.
Then, when a quantity of fetal blood crosses the placental membrane and enters the circulation to mix with the maternal blood, the maternal immune system recognizes these new red cells as antigens and begins the production of anti-Rh IgG antibodies to “destroy” the fetal red cells..
These antibodies also have the ability to cross the placental membrane and cause hemolysis of fetal erythrocytes, and even continue to produce hemolysis in the neonatal period. For this reason it is called hemolytic disease of the newborn.
Anti-D antibodies predispose D-positive red blood cells (from the fetus) to early destruction in the spleen, and it has been shown that when the amount of antibodies is excessive there is also liver destruction.
When the antibodies have been formed and the patient presents positive titers - regardless of the degree of the titration - the mother is considered to be isoimmunized.
Diagnosis
All pregnant women should undergo blood typing, in order to determine the ABO group and the Rh factor.
According to the result, if the maternal Rh factor is negative, the indirect Coombs test should be performed, in order to determine the presence of circulating antibodies in the maternal blood..
The Coombs test is a hematological and immunological test, which is also known as the antiglobulin test, which consists of obtaining a blood sample by venipuncture to determine if there is the presence of antibodies against the antigens of the red blood cells..
In the mother, the indirect Coombs test is performed, which will detect the presence in the maternal blood of circulating IgG antibodies directed at membrane antigens from other red blood cells..
In the fetus, the direct Coombs test is performed, which allows to identify the presence of said IgG anti-erythrocyte antibodies on the surface of fetal red blood cells..
Complications
The most frequent and dangerous complication of isoimmunization is hemolytic disease of the newborn, which causes hemolysis of erythrocytes with consequent complications for the baby..
In relation to the speed and magnitude of hemolysis, the fetus will be anemic. The severity of the condition of the intrauterine fetus will depend on the severity of said anemia..
Severe anemia leads to the establishment of a pathological entity known as hydrops fetalis or hydrops fetalis, which is characterized by severe edema secondary to the massive leakage of fluids into the organs and tissues of the fetus..
This anemia results in the intensification of erythropoiesis as a compensatory mechanism, both in the bone marrow and in the liver, adding to the picture medullary hyperplasia and evident hepatosplenomegaly.
Hepatomegaly accompanied by hyperbilirubinemia -product of the excessive release of bilirubin by massive hemolysis- produces severe jaundice that can be deposited in the brain.
This disease entity is called kernicterus, which is characterized by brain damage, seizures, and even death from bilirubin deposits in the brain..
Treatment
The treatment of isoimmunization is directed towards the prophylaxis of complications and can be initiated both in utero and in the newborn.
For intrauterine treatment, treatment is direct intrauterine transfusion of Rh- factor blood, with the aim of correcting anemia, hyperbilirubinemia and minimizing hemolysis.
For postpartum treatment, exchange transfusion is the method of choice. It consists of exchanging the newborn's blood for Rh- blood; that is, there is a replacement of the newborn's blood by one that does not present the antigen on its surface.
The exchange transfusion seeks to correct hyperbilirubinemia, reducing hemolysis in order to avoid the risk of kernicterus. Phototherapy can also be used to treat jaundice and prevent severe hyperbilirubinemia..
As prophylactic treatment, for maternal isoimmunization Rho D immunoglobulin (known as RhoGAM) is indicated, intramuscularly.
It is indicated in Rh- women with Rh + partners in the first weeks of pregnancy, before their immune system begins to produce anti-Rh antibodies..
With this vaccine, maternal sensitization is avoided by injecting 300 mg of immunoglobulin Rho D, which allows the neutralization of approximately 30 ml of blood from the fetus. It can also be indicated postpartum or post-abortion in Rh mothers-.
References
- Francisco Uranga. Practical Obstetrics. 5th Edition. Editorial Intermédica. Obstetric immunohematology. P. 825-844.
- Jorge Hernández Cruz. Sapiens Medicus. Incompatibility vs isoimmunization. Recovered from: sapiensmedicus.org
- Hector Baptista. Usefulness of direct antiglobulin test in neonatal screening. (2007) Recovered from: scielo.org.mx
- Dharmendra J. Nimavat. Pediatric Hydrops Fetalis. Jul 25. 2017. Medscape. Recovered from: emedicine.medscape.com
- Baptista GHA, Trueba GR, Santamaría HC. Clinically important blood groups, outside the ABO and Rh systems. Mexico: Editorial Prado; 2006. pp. 145-159



Yet No Comments