
Bulimia nervosa, factors of personal vulnerability

Bulimia nervosa is characterized by recurrent episodes of uncontrolled bingeing. These episodes of voracious eating are often followed by the use of methods to control weight gain. These weight control methods often achieve in the form of provoked vomiting, excessive exercise, food restrictions, and the use of laxatives and diuretics. Bulimia was first introduced in the DSM-III diagnostic system (APA, 1980) as its own diagnostic category.
For the next 14 years the most appropriate description of bulimia has been debated. The DSM-V diagnostic criteria describe two types of bulimia nervosa, the purgative and non-purgative types. The purgative subtype describes patients who combat binge eating through regular episodes of self-induced vomiting or the abuse of laxatives or diuretics. The non-purgative subtype describes patients who fast or exercise excessively, in order to compensate for episodes of binge-eating behavior, but who do not normally abuse laxatives, diuretics, or who do not use self-induced vomiting to control body weight. In DSM-V, a diagnosis of anorexia nervosa prevails over another of bulimia nervosa.
Contents
- Diagnostic characteristics of bulimia
- Types of bulimia
- Explanatory models
- Personal vulnerability factors
- Intervention in bulimia
- Main therapeutic targets for bulimia
Diagnostic characteristics of bulimia
- Presence of recurrent binges: characterized by food intake in large quantities and in a short period of time, with a feeling of loss of control over eating.
- Inappropriate compensatory behaviors, repeated to avoid gaining weight: excessive use of laxatives, diuretics, enemas, induction of vomiting, exaggerated exercise.
- Binge eating and compensatory behaviors occur at least twice a week for a period of 3 months.
- Self-assessment is excessively influenced by weight and body shape.
- The alteration does not appear exclusively in the course of anorexia nervosa.
Types of bulimia
- Purging type. During bulimia nervosa, the patient vomits, uses laxatives, enemas, or diuretics excessively.
- Non-purgative type. Compensatory behaviors are fasting or vigorous exercise.
Clinical complications occur in 40% of patients, with the suicide attempt being the most common risk of death in these patients, reaching 3%, although less than in anorexia nervosa.
The most frequent somatic alterations occur in the digestive system, the oral cavity being the most affected. They present erosions of the dental enamel, especially the inner face of incisors and canines, due to the acidic pH of the gastric juice and its continuous action on the enamel. The same pathogenesis is the presence of gingivitis, pharyngitis, and cheilitis. Parotid hypertrophy, related to vomiting and causing increased plasma amylase, has occasionally been observed; it is generally symmetrical and painful, disappearing at the end of the process in most cases. Alterations at the level of the esophagus range from the appearance of esophagitis to Mallory-Weiss syndrome. The capacity of the stomach is greatly increased, causing acute gastric dilation with local ischemic phenomena that can lead to gastric perforation. The abuse of laxatives or enemas can cause rectal bleeding, which requires a differential diagnosis with inflammatory bowel disease.

Likewise, cases of acute pancreatitis related to compulsive food intake, cardiac complications, which are not exceptional, have been described, with mitral valve prolapse being the most frequent alteration, although cardiac arrhythmias are also observed. Other frequent complications are poisonings from the abuse of emetics, diuretics and laxatives. However, osteoporosis is rare. It is noteworthy the possibility of the association between bulimia nervosa and diabetes mellitus (IDDM), Garfinkel described in 1987 a prevalence of 6.9% of bulimia in IDDM, since these patients when manipulating insulin doses as a method to eliminate excessive Calorie intake presents risk of ketoacidotic coma and poor control. At present, the importance of investigating an eating disorder in all patients with poorly controlled IDDM is stressed..
Explanatory models
In bulimia nervosa, binges often develop after a period of food restriction, resulting in hunger, a voracious appetite, and energy deprivation. Disruption of such food limitation is often triggered by emotional distress or eating forbidden foods. Laxative behavior decreases the anxiety that results from bingeing. This behavior also produces a decrease in nutrients to the body and can reduce the basic metabolism (Bennett, Williamson and Powers, 1989). A cyclical pattern of food restriction, binge eating, and purging behaviors often develops over time, and cognitive behavior therapy is designed to break this cycle of behaviors. From a cognitive-behavioral perspective, purgative behaviors and dieting are negatively reinforced by reducing anxiety about gaining weight (Williamson, 1990). Binge eating is considered to be sustained by a reduction in negative affect, in addition to the pleasurable effects of eating (Heatherton & Baumeister, 1991). Recently, body image theories of eating disorders have focused more on disturbance of body image as the primary motivation for disturbed eating behavior.
McPherson's (1988) cognitive model of bulimia starts from the basic premise that bulimia is a consequence of certain cognitive distortions derived from beliefs and values about body image and weight. The lack of self-control of the diet that appears in the bulimic patient (and in the anorexics with bulimic problems) would be related to an extreme need for control of these people in certain areas (school performance, body control, etc.). This cognitive vulnerability could be specified in the belief or basic assumption: "Weight and body image are essential for self-worth and social acceptance." With this belief, a series of cognitive distortions would be interrelated, standing out: 1) Dichotomous thinking (Polarization): It divides reality into extreme and opposite categories without intermediate degrees; eg, "Fat versus skinny"; 3) Personalization: Relates the events with their own behavior or as referring to themselves without real basis (eg, in a socially unskilled girl who believes: "They reject me because of my appearance"); 5) Overestimation of body image: they are perceived thicker than they are; 6) Global and generalized self-assessment:
They are globally estimated and valued in comparison to extreme social standards (eg, "If I don't have the body of a model I'm worthless").
The lack of control of the intake and the restriction of the diet that occur in the form of cycles would be related to the previous cognitive distortions. These, in turn, would interact with the biological needs of hunger, generating important conflicts that would give rise to these uncontrols and a return to attempts to control by restricting the diet. In addition, as these people lack better coping strategies, both the need for hunger and other sources of stress (eg, social situations) would act as predictive signs of threat, producing a state of anxiety that would act as a "cognitive distraction" and as " negative reinforcement "reducing anxiety. The mechanism of self-induced vomiting would respond to the same process described.
In summary, the two models presented are based on the importance of the social modeling of body image, personal vulnerability (meanings in relation to weight and social success, with social incompetence), cognitive distortions and the role of reinforcement as coping feedback of some strategies very limited personnel.

Personal vulnerability factors
(1) Perfectionistic attitudes:
(2) Personal meanings about
- Weight / body image
- Perfectionism
- Success / self-worth
- Low tolerance to frustration
(3) Lack of social skills.
Activating situation
(1) Acute or chronic stressors of a social or mental nature.
(2) feelings of hunger
Coping style
(1) Uncontrolled intake
(2) Use of laxatives or vomiting.
Anorexic symptoms and family pressure
(1) Short term: anxiety reduction, feeling of control
(2) Long term: increased discomfort, guilt, dysphoria.
Intervention in bulimia
A series of psychological therapies have been developed for the treatment of nervous anorexia and bulimia. Research on these treatment approaches has been around since the 1970s. Control group studies on such approaches have been carried out mainly with bulimia patients, due to the health risks associated with assigning patients with anorexia to placebo or no treatment groups. Most treatment research has focused on cognitive-behavioral and pharmacological therapies (Williamson, Sebastián, and Varnado, forthcoming). Short-term structured therapy, such as interpersonal therapy, has also been evaluated in recent years.
Rosen (1992) hypothesized that anorexia and bulimia nervosa are manifestations of a general body image disorder similar to what would be body dysmorphic disorder. This distortion of body image can be maintained by the bias of attention to information consistent with the beliefs that one's body figure is not attractive. From this perspective, behavioral changes emerge, such as avoiding wearing provocative dresses, restricting socialization, and avoiding sexual intimacy, stemming from efforts to reduce bodily dysphoria. Based on these cognitive-behavioral approaches, a number of treatment techniques have been tested. These approaches are summarized below. Behavioral and cognitive techniques are written separately. The reader should remember that most studies on CBT have combined a number of these cognitive and behavioral techniques..
Main therapeutic targets for bulimia
The patient's primary goal is the achievement of an idealized weight and body shape. This leads to rigid dieting, which predisposes you to occasional loss of control (binge eating). Given the absolute value they place on thinness, they undertake forms - also extreme - of compensation for such binges, such as self-induced vomiting. In turn, self-induced vomiting facilitates binge eating because the belief in its effectiveness in getting rid of eaten food reduces the natural tendency not to overeat. Excessive worry about weight and shape, particularly the tendency to make self-esteem dependent on them, promotes extreme dieting and thus keeps the whole problem going. Thus, the typical cognitive impairment of BN consists of an overrated set of ideas about weight and figure..
Based on the models previously presented, we can extract common therapeutic objectives for eating disorders:
- Develop realistic attitudes / beliefs about body image and weight;
- Establish a normal weight pattern;
- Reduction of lack of control in the ingestion, vomiting and abuse of laxative;
- Improve general personal functioning: self-acceptance, coping with anxiety and social functioning and,
- Establish motivation for treatment.
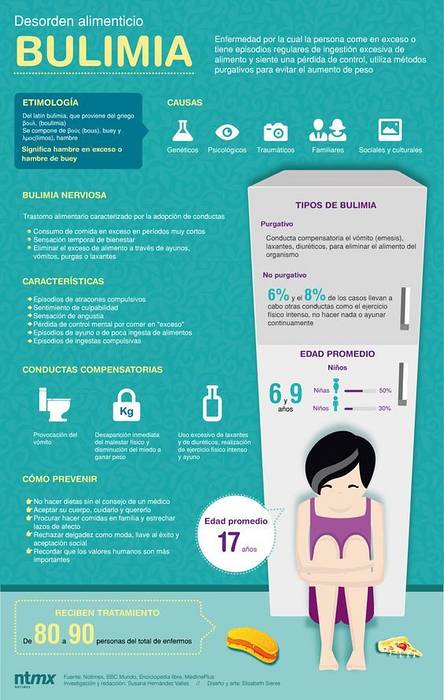
Below you can see an infographic where the key aspects of this disease are explained in summary.



Yet No Comments