
Fibrocystic Mastopathy Symptoms, Causes and Treatment
The fibrocystic mastopathy it is a chronic and non-malignant condition of the breasts, characterized by the presence of hardened areas scattered throughout the breasts with interspersed cystic lesions. It is the most common benign disease of the breasts and is caused by the compact proliferation of connective tissue.
Also known as fibrocystic disease or condition, it is the main reason for consulting the mastologist. It is estimated that 50% of adult women have clinical symptoms of fibrocystic mastopathy and up to 90% of the histological studies performed on the breast tissue of women over 40 years of age report the presence of this pathology.
Most patients go to the doctor when they feel the presence of a palpable mass in the breast. The symptoms, apart from the aforementioned breast hardening, is not so florid. Certain tests and technical studies are carried out to reach a definitive diagnosis and rule out the much dreaded breast cancer.
Treatment is not always surgical, even when that is the general idea. There are therapeutic alternatives: from pharmacological formulas to naturopathic drugs. The most appropriate choice in terms of treatment will be made in conjunction with the patient and the treating physician..
Article index
- 1 Symptoms
- 1.1 Palpable masses
- 1.2 Pain
- 1.3 Volume increase
- 1.4 Other symptoms
- 2 Causes
- 3 Diagnosis
- 3.1 Mammography
- 3.2 Ultrasound
- 3.3 Magnetic resonance
- 3.4 Fine needle puncture
- 4 Treatment
- 4.1 Medical treatment
- 4.2 Surgical treatment
- 5 References
Symptoms
Palpable masses
The main symptom of fibrocystic mastopathy is palpation of a solid mass in one or both breasts. Most women who regularly perform breast self-examination may find localized hardening with lesions of different sizes and consistencies..
The characteristics of these masses can vary according to cyclical behavior. The hormonal load has a direct effect on these, causing changes in their size, texture and sensitivity. According to the report of most of the patients, the symptoms worsens in the premenstrual stages.
The location of the nodules or cysts is variable, but there is a certain predilection for the upper and outer quadrants. Although one-sidedness is possible, most often both breasts are affected. Sometimes dense plaques are palpable instead of nodules and numerous irregularities are felt to the touch.
Pain
It is the second cardinal symptom of fibrocystic disease. Although spontaneous pain is not usually present, palpation of the affected breasts does cause significant discomfort.
This symptom is also cyclical, and as the masses change in the premenstrual period, the pain is also exacerbated at that time.
Some patients describe greater tenderness in the breasts and not pain specifically. Any manipulation, friction or trauma is more annoying in patients with fibrocystic mastopathy than in healthy ones.
Volume increase
The "swelling" of the breasts is the third most common and important symptom of fibrocystic disease. Like the previous two, it has a tendency to be accentuated immediately before and during menstruation. The skin of the inflamed breasts is more sensitive, has greater turgor and shine as in swollen tissues.
Other symptoms
The presence of greenish or brown discharge through the nipple is an infrequent but worrisome finding of this pathology.
The color of this discharge is very important to differentiate it from that that appears with cancer, which is rather reddish or bloody. It almost never has a bad odor, which would be another red flag.
Some patients report pain and swelling in the axillary area. It is common that in this area there are remnants of breast tissue and that therefore these symptoms may appear in relation to the menstrual cycle.
An interesting phenomenon is that some patients with fibrocystic mastopathy who underwent augmentation mammoplasty show decreased symptoms of the disease.
Apparently, the compression exerted by the prostheses on the breast tissue causes it to atrophy and, therefore, the nodules and cysts disappear.
Causes
Despite being a well-studied disease, the formal causes of the condition are still unknown. However, most authors and researchers agree that hormones play a fundamental role in the genesis of fibrocystic mastopathy, especially estrogen, progesterone, and prolactin..
This theory is reinforced by the fact that postmenopausal women show a decrease in symptoms and even speak of a cure.
Even more so when those patients who, for other medical reasons, start hormone replacement therapy, report the reappearance of symptoms and many times with greater intensity.
Hormones act directly on breast cells, making them grow and multiply; this effect is normal.
The problem is that after years of hormonal stimulation, cysts and nodules with areas of dense fibrotic tissue begin to appear. Hence, the age of onset of the disease is after 30 years.
Diagnosis
In addition to the physical examination, which is very guiding, the definitive diagnosis is made through paraclinical techniques, including the following:
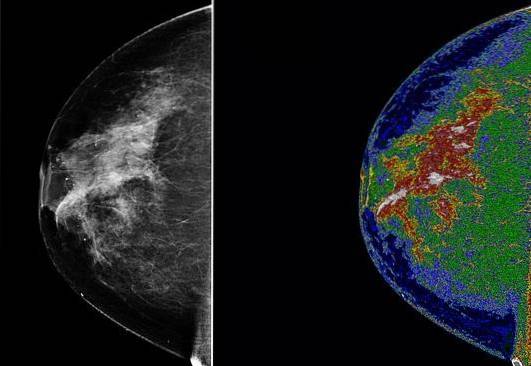
Mammography
It is the study par excellence to diagnose breast pathologies. It allows to identify small lesions that cannot be detected through manual palpation.
Its main drawback is pain, since the breast is subjected to significant compression by two plates that close on themselves.
Ultrasound
It is usually the initial study when breast disease is suspected because it is easy to perform and not painful. Captures voluminous cystic lesions without problems, but has a problem with smaller lesions and fibrotic tissue, which can be confused with the normal breast.
Magnetic resonance
It is not of choice for the diagnosis of fibrocystic changes in the breast, but it is very useful to differentiate malignant from benign lesions..
It also serves to detect multifocal and multicentric lesions, which cannot be evaluated with mammography or ultrasound..
Fine needle puncture
Although the puncture itself is only the sampling procedure, it is also understood as the histological studies that are performed..
The information provided by this test allows a definitive diagnosis to be made by knowing the specific characteristics of the cells present there, and it is vital to differentiate this condition from cancer..
Treatment
There are two complementary therapeutic trends: medical treatment and surgical treatment..
Medical treatment
Over-the-counter pain relievers and anti-inflammatories are indicated immediately; Ibuprofen and acetaminophen are the most widely used. Oral contraceptives, by regulating hormonal load, are also helpful as part of treatment. Vitamin E and supplements with soy and iodine have shown interesting results, but without clear scientific support.
Diet changes are recommended, trying to eliminate caffeine and xanthines, reducing fatty foods and increasing foods rich in essential fatty acids. The intake of abundant fluids is positive to preserve the hydration of the breast tissue and reduce the formation of fibrosis.
Surgical treatment
Cyst drainage through external needle puncture is less invasive and aggressive, but not very efficient. The cysts can refill and require new punctures. In addition, the procedure is not so simple in inexperienced hands, requiring the support of tomographic or ultrasound equipment..
Surgical resection of cysts is unusual and is only performed when the cysts are very painful, deforming, or suspected of malignancy. Surgery is never considered as initial treatment unless one of the three previously mentioned conditions is met..
References
- Cafasso, Jacquelyn (2016). Fibrocystic Breast Disease. Recovered from: healthline.com
- Mayo Clinic Staff (2017). Fibrocystic breasts. Recovered from: mayoclinic.org
- Maychet Sangma, Mima B .; Panda, Kishori and Dasiah, Simon (2013). A Clinico-Pathological Study on Benign Breast Diseases. Journal of Clinical & Diagnostic Research, 7 (3): 503-506.
- Santen, Richard J. (2017). Benign Breast Disease in Women. Recovered from: endotext.org
- Wikipedia (last edition 2018). Fibrocystic breast changes. Recovered from: en.wikipedia.org
- Gallo Vallejo, J. L. and collaborators (2013). Fibrocystic mastopathy. Controversial aspects. Clinic and Research in Gynecology and Obstetrics, 40 (6): 269-276.

Yet No Comments