
Mycosis types and treatments
The mycosis they encompass all infections caused by pathogenic fungi in humans. Contact with such a microbial agent will develop host disease due to its pathogenicity. A mycosis is, then, the effect caused by a fungus in the tissue that colonizes.
Fungi are eukaryotic organisms belonging to the fungi kingdom, which require interaction with another living organism to survive. The tissues for which it has an affinity can be of animal or plant origin, depending on its species. The dissemination and reproduction of the fungus is through spores that it releases into the environment.

The fungal infection occurs in man when he is exposed to the spores present in his environment. These can enter the body by direct contact with the skin, inhalation or accidental inoculation. The variety of symptoms that occur depend on the location of the fungus, in addition to its ability to cause disease.
Mainly pathogenic fungi are microorganisms whose development occurs within the host cell. Thus, it takes advantage of the available resources to survive and multiply, guaranteeing its development..
The property of a fungus to produce disease is called pathogenicity, and it involves different mechanisms. Changes in its structure, adherence to tissues, secretion of proteolytic enzymes and synthesis of the protective envelope are some of the processes that allow infection..
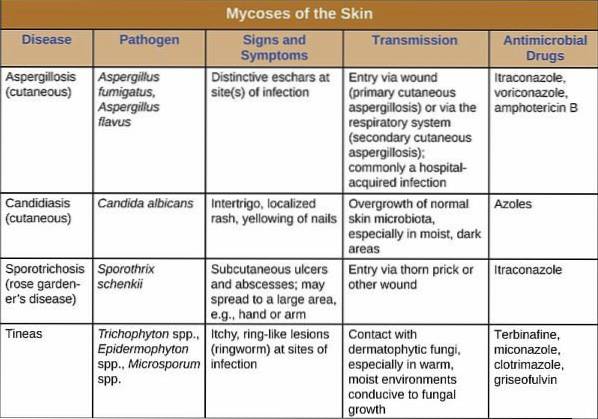
There is a classification of mycoses, according to the place of infection: superficial and deep. The former - more frequent - are limited to the skin and cutaneous annexes, while the others invade and infect internal organs and are more serious.
The distribution of this pathology is worldwide, without discrimination of age and sex. Some activities predispose to suffer them. The most susceptible groups are children, the elderly and the immunosuppressed.
Article index
- 1 Types, symptoms and causes
- 1.1 Superficial mycoses
- 1.2 Deep or systemic
- 1.3 Subcutaneous mycoses
- 2 Treatments
- 2.1 Non-pharmacological
- 2.2 Pharmacological
- 3 References
Types, symptoms and causes
The division of the fungal infection has been established taking into account the species involved and the tissue that it colonizes. According to this, they are classified as superficial, subcutaneous and deep..
The so-called superficial mycoses are a group of diseases that affect both skin and hair and nails. They are usually frequent in the population, benign and disappear with the opportune treatment.
Deep mycoses - also called systemic or disseminated - are characterized by their attack on internal organs. They are less frequent, but more serious, in addition to requiring in-hospital management for their treatment.
Some deep mycoses may have skin manifestations as a result of their spread.
Superficial mycoses
Ringworms, tines, or dermatophytosis
Ringworms are caused by dermatophytes, fungi characterized by their affinity to keratin. They have proteolytic enzymes capable of degrading keratin and thus allowing it to adhere to the tissue. The species involved in dermatophytoses belong to the genera Trichophyton, Microsporum and Epidermophyton.
Dermatophytoses are named according to the area where the lesions are located:
Tinea capitis
It is caused mainly by Microsporum canis and Trichophyton tonsurans. It affects the scalp, causing various types of injury, from hyperkeratotic grayish plaques to inflammatory plaques with hair loss. A variety of ringworm - the Querion de Celso - occurs when abscesses appear in the affected area.
Hair involvement occurs if the causative agent is able to penetrate inside or not. In the first case, the hair can become weak or break. Alopecia occurs when inflammation spreads to the hair follicles.
Tinea faciei
This variety occurs in hair-free facial areas and can coexist with tinea corporis. It can affect men, women and children.
Several species of fungi are implicated, including Microsporum canis, and Trichophyton mentagrophytes, rubrum, and tonsurans..
The classic ring-like, serpeginous, and pruritic lesions can occupy any portion of the face. Desquamation of lesions is common.
Tinea barbae
As its name suggests, it occurs in the facial area occupied by the beard and is limited to adult men. The main causative agents are Trichophyton verrucosum and mentagrophytes, in addition to Microsporum canis.
Symptoms include inflammatory, nodular, exudative plaques, and hardening of the skin. The non-inflammatory lesions are similar to those found in ringworm. The presence of folliculitis is variable and produces localized alopecia.
Tinea corporis

It affects most of the body surface. Trichophyton rubrum is the main causal agent, in addition to T. tonsurans. Initially the lesion is characterized by reddish plaques that later expand from the center, forming a reddish ring around healthy areas. The active border has both papules and vesicles and pustules.
Symptoms associated with plaques include itching, scaling, and a burning sensation. Sometimes a nodular folliculitis -Majocchi granuloma- occurs, which usually causes pain. A variety of plates are purplish or gray in color.
One form of ringworm produces multiple confluent plaques that occupy large areas. It is the characteristic of tinea imbricata caused by Trichophyton concentricum.
Tinea cruris
It is located in the inguinal folds, and can extend to the genitals, perineum, gluteal folds, and inner thighs. Germs can be transferred by transfer - hands, towels - from a tinea pedis.
It produces multiple itchy reddish plaques or large plaques with active border. The affected area is usually moist and eroded by scratching, releasing a serous exudate. Discoloration or hyperkeratosis is also related to scratching.
It is a common condition and the causative agents involved are Epidemophyton floccosum and Trichophyton rubrum. Lack of hygiene, tight clothing and hot weather are triggers.
Tinea pedis
Fungal infection of the feet is very common and is also known as "athlete's foot." It is due to contact with Trichophyton rubrum, tonsurans or mentagrophytes, but also with Epidermophyton floccosum. It is a recurrent and sometimes chronic infection.
The clinical signs are plaques that thicken the skin, predominantly plantar and lateral on both feet. In the affected areas there is thick scaling and itching. Scratching can cause bacterial superinfection and spread -by transfer- to other parts of the body.
It is very common to find infection in the interdigital folds. There, the fissures, ulcerations, exudate and maceration of the tissue are secondary to the localized infection. The presence of tinea pedis is a predisposing factor, or trigger, for onychomycosis.
Tinea manuum
It occurs by transfer of ringworm of the feet, so they have the same causative agents and type of injury in common. The risk of bacterial superinfection is high.
Pityriasis versicolor

Its most common cause is Malassezia furfur infection. The term versicolor is due to the presence of whitish, reddish or grayish spots and plaques. There is fine scaling in the lesions and they are not pruritic.
They are predominantly located on the face, neck, upper part of the thorax and sometimes upper limbs and abdomen. Risk factors for this infection are humidity, the presence of body fat, and the immune system. There is a family predisposition for this condition.
Candidiasis
Superficial candidiasis is a manifestation of Candida albicans infection that affects the skin and mucous membranes. The characteristic symptoms are reddening of the area, exudate and maceration of the tissue. When it affects mucous membranes, whitish plaques are usually observed that when detached, cause bleeding.
The normal location of this mycosis is in dermal folds, genital area -vagina and glans-, as well as in the oral mucosa. Vulvovaginitis and balanitis produce local redness associated with itching, burning, and thick whitish exudate.
Mycosis of the hair
White stone and black stone are hair fungal infections caused by Trichosporum sp. and Piedraia hortae respectively. This mycosis is usually asymptomatic.
In the black stone the nodules are black and firm in consistency, while the whitish and soft nodules characterize the white stone. Rarely does mycosis coexist with tinea capitis.
Onychomycosis
It corresponds to the mycosis of the nails. Dermatophytes have keratolytic enzymes capable of degrading the keratin of the nail and producing the changes that are observed in it.
It predominantly attacks the distal edge of the annex producing changes in color, texture and shape until it reaches onycholysis or destruction of the nail. It also causes its separation from the nail bed.
It is a risk factor related to the appearance of onychocryptosis. The cause in most cases is contact with Trichophyton rubrum, but also by Epidermophyton floccosum and T. mentagrophytes.
Candida produces paronychia, an infection that attacks the soft tissues around the nail. When it involves the proximal nail bed, it produces deformity and separation of the nail root.
Deep or systemic
These pathologies occur when internal organs are compromised by a fungal infection. Subcutaneous mycoses are included in this group..
Deep mycoses are caused by primary and opportunistic pathogenic fungi. In the first case, any healthy individual can acquire the disease, while immunosuppression allows the attack of opportunists.
Histoplasmosis
It is a primary infection that occurs by inhalation of Hystoplasma capsulatum spores. Its entry into the respiratory tract produces mild respiratory symptoms - dry cough or expectoration - or it may be asymptomatic. In most cases it cures without consequences.
Complicated cases of histoplasmosis cause destruction and fibrosis in the lung, causing symptoms of chronic respiratory infection. The spread of the infection can cause a large number of symptoms, related to the affected system:
- Anemia
- Weightloss.
- Bloating and abdominal pain.
- Jaundice.
- Fever.
Blastomycosis
Caused by Blastomyces dermatitidis. The spores of this fungus are found in soils contaminated with excrement or decomposed organic matter. When inhaled, they enter the respiratory tract, causing asymptomatic infection, or symptoms of pneumonia..
Like histoplasmosis, it can cause lung injury, with fibrosis and cavities, in complicated cases. Cough with greenish or bloody sputum, shortness of breath, and fever are common symptoms. There may be pleural effusion and alveolar exudate.
When it spreads, it can pass to mucous membranes and skin, producing very painful hard-edged ulcers..
Coccidioidomycosis
The fungus that causes it - Cocidioides immitis - has an infectious form, arthroconidia, which are inhaled and pass into the respiratory system. It produces from mild respiratory infection to acute or chronic pneumonia. Coughing up blood is common. The chronic form is associated with continuous fever and progressive weight loss.
Spread includes skin and subcutaneous involvement, bones, joints and bones, producing severe infection. In skin it produces ulcers, while in bone it can produce purulent exudate. It is possible to find, in severe cases, meningitis.
Aspergillosis
Opportunistic infection caused by fungi of the genus Aspergillus, specifically A. fumigatus. Various forms of aspergillosis are distinguished, including allergic sinusitis and bronchitis, aspergilloma, and disseminated infection.
Symptoms depend on the clinical form, with rhinorrhea, nasal obstruction, headache, cough, wheezing, and respiratory distress being common. Aspergilloma produces clinical signs of chronic lung infection, such as coughing up blood.
Paracoccidioidomycosis
Mainly the cause is due to the presence of Paracoccidioides brasiliensis. Initial symptoms can be mild or absent. It colonizes the respiratory tract and from there it spreads. Respiratory infection produces cough with expectoration, dyspnea, and fever. Produces hard, inflammatory ulcers in respiratory mucosa.
In the clinical picture, weight loss, skin ulcers, swollen and suppurative lymph nodes may also be present..
Pneumocystosis
Opportunistic pneumonia related to HIV / AIDS infection and other immunosuppressive conditions. Its causal agent is Pneumocystis carinii, previously called P. jirovecii.
It initially causes symptoms of the common cold, followed by frequent and severe cough, dyspnea with pulling, and chest pain. In immunosuppressed patients it is a relatively serious infection.
Candidiasis
Infection extended to respiratory and digestive mucosa involving Candida sp. and Candida albicans. This fungus is a normal resident of the skin and intestinal mucosa. When the immune system fails, opportunistic infection appears, which can spread to the mouth and esophagus, producing whitish plaques and painful local inflammation..
Its dissemination is serious, causing symptoms according to the invaded organs.
Subcutaneous mycoses
They are considered deep infections, since they involve tissues below the cutaneous plane. These infections include:
Chromoblastomycosis
Subcutaneous nodules that can develop polymorphic lesions, such as plaques, warts, nodular chains, among others. It is usually of a chronic course. The causative agents are Fonsecaea pedrosoi, F. compacta, Cladosporium carrionii or Phialophora verrucosa.
Mycetomas
Subcutaneous nodular lesions that can invade deep planes up to the bone. The presence of a raised plaque or nodule that forms a fistula and presents granulations inside is characteristic. It is produced by Madurella mycetomatis.
Sporotrichosis
Gardeners or farmers disease. The fungus -Sporothrix schenckii is usually found on the stem, branches or thorns of a plant and its contagion is by accidental puncture.
It invades the lymphatic vessels producing subcutaneous nodules that continue on its way. Superficial ulceration of the nodules is common.
Its spread through the lymphatic pathway makes it possible for it to invade other organs - such as bones and joints, lung and meninges - or to spread throughout the body..
Treatments

Non-pharmacological
Education aimed at prevention and proper hygiene is one of the main tools for non-pharmacological treatment.
- The care of the skin, nails and hair, use of suitable clothing, body and clothing hygiene is important to prevent superficial fungal infections.
- The risk factors associated with deep fungal infections must be taken into account.
- Avoid or exercise caution in endemic areas for some pathogenic fungi.
- Avoid contact with animals or people with suspicious injuries, especially if they are communicable infections.
Pharmacological
Given the variety of clinical manifestations of mycoses, treatment can vary. Each treatment scheme will be adapted taking into account the causative agent and the severity of the symptoms..
For superficial mycoses, the use of topical medication -cream, emulsions, lotions, shampoo, lacquers- combined with systemic treatment is the most effective..
Deep and disseminated mycoses require the use of oral or parenteral antifungals. It is necessary to take into account the treatment of the symptoms that accompany fungal infections:
- Hydration.
- Diet regimen.
- Analgesics, anti-inflammatories and antipyretics.
- Steroids.
- Antibiotics.
Topical
- Ketoconazole, shampoo, cream, lotion.
- Clotrimazole 1%, lotion or cream.
- Luliconazole 1%, cream.
- Econazole, cream.
- Miconazole, solution or cream.
- Selenium Sulfate, shampoo.
- Zinc pyritonate, shampoo.
- Terbinafine, cream.
- Naftifine 1%, cream.
- Fluconazole, cream.
- Sertaconazole Nitrate, cream.
Orally
- Ketoconazole, tablets.
- Griseofulvin, tablets
- Fluconazole, as capsules or tablets.
- Itraconazole, capsules.
- Pramiconazole, tablets.
- Voriconazole, tablets.
Parenteral route
- Fluconazole, as a solution for injection.
- Amphotericin B, solution for injection.
References
- Ryan, KJ. Pathogenic fungi. Sherris Medical Microbiology. 6th edition (2014). Part IV, Chapter 42 - 47
- Wikipedia (last rev 2018). Pathogenic fungus. Recovered from en.wikipedia.org
- Casadevall, A (2007). Determinants of virulence in the pathogenic fungi. Recovered from ncbi.nlm.nih.gov
- Kurosawa, CS; Sugizaki, MF; Serrão Peraçoli, MT (1998). Virulence factors in fungi of systemic mycoses. Journal of the Institute of Tropical Medicine of São Paulo. Recovered from scielo.br
- Mohamed, AW (2012). Fungal infection. Recovered from healthline.com
- Satter, E (2017). Superficial mycoses: Dermatophytosis. Recovered from infectiousdiseaseadvisor.com
- CDC (s.f.). Types of fungal diseases. Recovered from cdc.gov
- Andrews, S (2017). Tinea in emergency medicine. Recovered from emedicine.medscape.com
- Knott, L (2014). Systemic mycoses. Recovered from patient.info
- Walsh, TJ; Dixon, DM (1996). Spectrum of mycoses. Medical microbiology. Recovered from ncbi.nlm.nih.gov
- Johnson, J (Last rev 2017). What you need to know about fungal infections. Recovered from medicalnewstoday.com
- Fleta Zaragozano, J (2001). Deep mycoses. Recovered from elsevier.es
- Informed (2010). Deep mycoses and opportunistic mycoses. Recovered from infodermatologia.com
- The University of Adelaide (s.f.). Dimorphic Systemic Mycoses. Recovered from mycology.adelaide.edu.au
- Schenfield, NS (2018). Cutaneous candidiasis. Recovered from emedicine.medscape.com
- Crouse, LN (2018). Tinea versicolor. Recovered from emedicine.medscape.com
- Harman, EM (2018). Aspergillosis. Recovered from emedicine.medscape.com
- King, JW (2017). Cryptococcosis. Recovered from emedicine.medscape.com
- Agudelo Higuita, MA (2017). Sporotrichosis. Recovered from emedicine.medscape.com
- Schwartz, RA (2018). Stone. Recovered from emedicine.medscape.com
- Schwartz, RA (2018). Chromobastomycosis. Recovered from emedicine.medscape.com
- Ayoade, FO (2017). Mycetoma. Recovered from emedicine.medscape.com


Yet No Comments