
Mycoplasma genitalium characteristics, morphology, pathogenesis
Mycoplasma genitalium It is a very demanding bacterium that has been isolated from the human genital and respiratory tracts, as well as from primates. However, the pathogenic role that this microorganism plays in these places is not very clear, since they can be there without causing damage..
Some researchers assure that there is sufficient data to associate it as a causative agent of non-gonococcal, non-chlamydial urethritis in men and various urogenital diseases in women and even with infertility.
Article index
- 1 Features
- 2 Taxonomy
- 3 Morphology
- 4 Virulence factors of Mycoplasma genitalium
- 5 Pathogenesis
- 6 Clinical manifestations
- 7 Pathology
- 8 Diagnosis
- 9 Treatment
- 10 References
Characteristics
-This microorganism is very difficult to cultivate and when it is cultivated it grows very slowly..
-Biochemical tests give very similar to M. pneumoniae. It is characterized by fermenting glucose and does not use arginine, nor does it split urea.
-Their optimum pH is 7, they grow well at 35 ° C with a CO atmosphere.two.
-Of all the Mycoplasmas, the genitalium species is the one with the smallest genome.
Taxonomy
Domain: Bacteria
Phylum: Firmicutes
Class: Mollicutes
Order: Mycoplasmatales
Family: Mycoplasmataceae
Genus: Mycoplasma
Species: genitalium
Morphology
It has a soft and flexible trilaminar cytoplasmic membrane that is why it belongs to the class Mollicutes which means soft skin, referring to the fact that they lack a rigid bacterial cell wall.
Mycoplasma genitalium presents many morphological characteristics similar to Mycoplasma pneumoniae.
Especially in its tapered bottle shape and the presence of a specialized apical structure that facilitates adherence to tissue cells, erythrocytes, and inert plastic or glass material.
Virulence factors of Mycoplasma genitalium
As a prominent virulence factor in M. genitalium is the presence of a 140 kDa protein called P140, this being a structural and functional counterpart of the 170 kDa P1 adhesin present in M. pneumoniae.
Likewise, M. genitalium presents antigenic epitopes shared with M. pneumoniae which causes cross reactions between these microorganisms.
Pathogeny
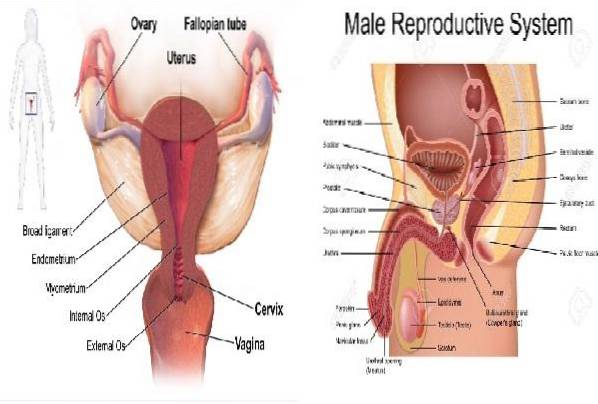
Infection by M. genitalium it is characterized by a stage of colonization of the urogenital epithelium and subsequently followed by an acute stage of active multiplication of the microorganism.
Inflammation of the tissue appears and the appearance of clinical manifestations.
At this stage, it should be treated with an antibiotic, if not, the infection can become chronic where signs and symptoms disappear, leading to a presumed remission..
However, microorganisms continue to multiply on the surface of the urogenital epithelium. This chronic infection can compromise reproductive capacity in women..
Likewise, it is known that this bacterium is located extracellularly but there are indications that it can also be located intracellularly, the infection being more severe in the latter case.
This characteristic suggests a massive invasion of the microorganism with intracellular multiplication that guarantees its persistence and therefore a more uphill treatment..
On the other hand, it is common to observe that non-gonococcal urethritis in men presents without symptoms or abnormal urethral discharge, the only manifestation being the appearance of moderate leukocyturia in the urine..
Clinical manifestations
Lower abdominal pain, pelvic inflammation, and endometritis usually occur. And in men there may be burning when urinating, there may or may not be purulent urethral discharge and leukocyturia.
Pathology
The role of this microorganism in human diseases is controversial since it has been found in asymptomatic people, therefore it is believed that it may act as an opportunistic pathogen.
In this sense, it has been attributed as a causal agent in non-gonococcal, non-chlamydial urethritis in men. With the particularity that you are more likely to find M. genitalium of the urethra of homosexual men than of heterosexuals.
While, M. genitalium has been isolated in women with non-gonococcal, non-chlamydial, or attributable salpingitis M. hominis. As well as mucopurulent cervicitis.
However, the prevalence rate is relatively low (10%) in both symptomatic and asymptomatic women. Increasing by 30% in sex workers.
In the respiratory tract its participation in respiratory diseases is not well defined, but it has been suggested that it can act synergistically with M. pneumoniae, resulting in a more severe pneumonic infection.
It may even contribute to the extrapulmonary complications of infection by M. pneumoniae.
Now in addition to the respiratory and genital tract also M. genitalium has been isolated from aspirated joint fluid from arthritis patients and from the blood of HIV patients.
Diagnosis
For the diagnosis of M. genitalium the clinical samples par excellence are: vaginal exudate, urethral exudate, endocervical exudate and urine samples in women and urethral exudate and urine in men.
As special culture media for M. genitalium Diphasic broth SP-4 and agar SP-4 are used.
For semi automated identification of Mycoplasmas genitalum and other urogenital pathogens, the A.F. Genital System, which contains biochemical tests and the antibiogram.
The differentiation of the presence of M. genitalium and other bacteria like M. hominis Y U. urealyticum is colorimetric and semi-quantitative.
However, because the culture can be negative due to the difficulty of its recovery, it is recommended to make the diagnosis through molecular tests..
Such as: use of nucleic acid primers and probes for PCR that are specific for M. genitalium.
As this microorganism is generally found in low concentration in clinical samples, a highly sensitive diagnostic method such as PCR is needed..
Treatment
On some occasions, patients with urogenital pathologies are treated empirically with antibiotics to eradicate other urogenital pathogens, but if the microorganism present is M. genitalium these therapies fail, especially if beta-lactam antibiotics are used.
The reason for the failure is due to the fact that this bacterium lacks a cell wall, therefore it cannot be treated with antibiotics whose mechanism of action is exerted on this structure..
Mycoplasma genitalium can be treated with erythromycin at a concentration < 0,015 µg/mL.
References
- Koneman E, Allen S, Janda W, Schreckenberger P, Winn W. (2004). Microbiological Diagnosis. (5th ed.). Argentina, Editorial Panamericana S.A.
- Lilis R, Nsuami M, Myers L, Martin D, Utility of urine, vaginal, cervical, and rectal specimens for detection of Mycoplasma genitalium in women. J Clin Microbiol 2011; 49 (5) 1990-1992
- Mondeja-Rodríguez B, Skov J, Rodríguez-Preval N, Capote-Tabares M, Rodríguez-González I, Fernández-Molina C. Detection of Mycoplasma genitalium by polymerase chain reaction in urogenital samples from sexually active Cuban individuals. VacciMonitor 2014; 23 (1): 17-23. Available at: scielo.org
- Fernández-Molina C, Rodríguez-Preval N, Rodríguez-González I, Agnese-Latino M, Rivera-Tapia J, Ayala-Rodríguez I. Diagnosis of Mycoplasma genitalium by amplification of the mgPa genes and 16S ribosomal RNA. Public health Mex. 2008; 50 (5): 358-361. Available at: scielo.org
- Arraíz N, Colina S, Marcucci R, Rondon N, Reyes F, Bermúdez V, and Romero Z. Detection of Mycoplasma genitalium and correlation with clinical manifestations in a population of the State of Zulia., Venezuela. Rev. Chil infectol. 2008; 25 (4): 256-261. Available at scielo.org
- Rivera-Tapia J, Rodríguez-Preval N. Mycoplasmas and antibiotics. Public health Mex. 2006; 48 (1): 1-2. Available at scielo.org


Yet No Comments