
Characteristic platelets, morphology, origin, functions
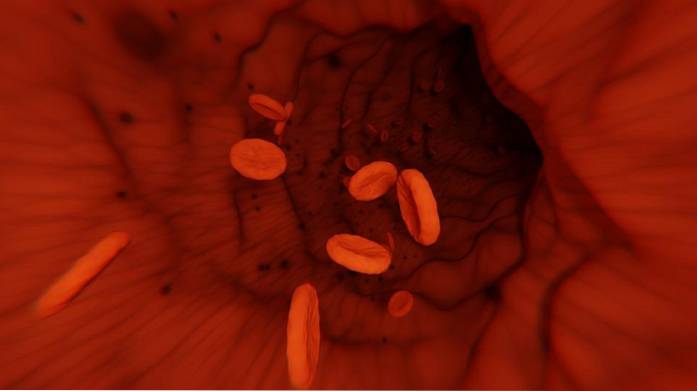
The platelets or thrombocytes They are cell fragments of irregular morphology that lack a nucleus and we find them forming part of the blood. They are involved in hemostasis - the set of processes and mechanisms that are responsible for controlling bleeding, promoting coagulation.
The cells that give rise to platelets are called megakaryocytes, a process orchestrated by thrombopoietin and other molecules. Each megakaryocyte will progressively fragment and give rise to thousands of platelets.
Platelets form a kind of "bridge" between hemostasis and the processes of inflammation and immunity. They not only participate in aspects related to blood clotting, but also release antimicrobial proteins, which is why they are involved in defense against pathogens.
In addition, they secrete a series of protein molecules related to wound healing and connective tissue regeneration..
Article index
- 1 Historical perspective
- 2 Characteristics and morphology
- 2.1 Overview of platelets
- 2.2 Central region
- 2.3 Peripheral region
- 2.4 Cell membrane
- 3 How did they originate?
- 3.1 The megakaryoblast
- 3.2 The little promegacario
- 3.3 The basophilic megakaryocyte
- 3.4 The megakaryocyte
- 3.5 Process regulation
- 3.6 Incomplete cell division of megakaryocytes
- 3.7 Role of thrombopoietin
- 3.8 In which organ are platelets formed?
- 4 Functions
- 5 Normal Values in Humans
- 6 Diseases
- 6.1 Thrombocytopenia: low platelet levels
- 6.2 Thrombocythemia: high platelet levels
- 6.3 von Willebrand disease
- 7 References
Historical perspective
The first investigators to describe thrombocytes were Donne et al. Later, in 1872, Hayem's research team corroborated the existence of these blood elements, and confirmed that they were specific to this liquid connective tissue..
Later, with the arrival of electron microscopy in the 1940s, the structure of these elements could be elucidated. The discovery that platelets are formed from megakaryocytes is attributed to Julius Bizzozero - and independently to Homer Wright.
In 1947, Quick and Brinkhous found a relationship between platelets and thrombin formation. After the 1950s, improvements in cell biology and the techniques to study it led to the exponential growth of existing information on platelets..
Characteristics and morphology
Platelets overview
Platelets are disc-shaped cytoplasmic fragments. They are considered to be small - their dimensions are between 2 to 4 um, with an average diameter of 2.5 um, measured in an isotonic buffer..
Although they lack a nucleus, they are complex elements at the level of their structure. Its metabolism is very active and its half-life is a little over a week.
Circulating platelets often exhibit a biconvex morphology. However, when blood preparations treated with a substance that inhibits clotting are observed, the platelets take a more rounded shape..
Under normal conditions, platelets respond to cellular and humoral stimuli, acquiring an irregular structure and a sticky consistency that allows adherence between their neighbors, forming aggregates..
Platelets can exhibit certain heterogeneity in their characteristics, without this being the product of any disorder or medical pathology. In each microliter of circulating blood, we find more than 300,000 platelets. These help clotting and preventing potential damage to blood vessels.
Central region
In the central region of the platelet we find several organelles, such as mitochondria, endoplasmic reticulum and Golgi apparatus. Specifically, we find three types of granules inside this blood element: alphas, dense and lysosomal..
Alpha granules are responsible for housing a series of proteins that are involved in hemostatic functions, including platelet adhesion, blood clotting, endothelial cell repair, among others. Each plate has from 50 to 80 of these granules.
In addition, they contain antimicrobial proteins, since platelets have the ability to interact with microbes, being an important part of the defense against infections. By releasing some molecules, platelets can recruit lymphocytes.
The dense-core granules contain mediators of vascular tone, such as serotonin, DNA, and phosphate. They have endocytosis capacity. They are less numerous than the alpha ones, and we find from two to seven per platelet.
The last type, lysosomal granules, contain hydrolytic enzymes (as occurs in lysosomes that we normally know as organelles of animal cells) that play an important role in the dissolution of the thrombus..
Peripheral region
The periphery of platelets is called the hyalomer, and it contains a series of microtubules and filaments that regulate the shape and motility of the platelet..
Cellular membrane
The membrane that surrounds platelets has a structure identical to any other biological membrane, composed of a double layer of phospholipids, distributed asymmetrically.
Phospholipids of a neutral nature such as phosphatidylcholine and sphingomyelin are located on the outer side of the membrane, while lipids with anionic or polar charges are located towards the cytoplasmic side..
Phosphatidylinositol, which belongs to the latter group of lipids, participates in the activation of platelets
The membrane also contains esterified cholesterol. This lipid can move freely inside the membrane and contributes to its stability, maintains its fluidity and helps control the passage of substances..
On the membrane we find more than 50 different categories of receptors, among them integrins with the capacity to bind to collagen. These receptors allow platelets to bind to injured blood vessels..
How do they originate?
Generally speaking, the platelet formation process begins with a stem cell (from the English stem cell) or pluripotential stem cell. This cell gives way to a state called megakaryoblasts. This same process occurs for the formation of the other elements of the blood: erythrocytes and leukocytes..
As the process progresses, the megakaryoblasts originate the promegakaryocyte that will develop into a megakaryocyte. The latter divides and produces a high number of platelets. We will develop each of these stages in detail below..
The megakaryoblast
The platelet maturation sequence begins with a megakaryoblast. A typical one has a diameter between 10 and 15 um. In this cell, the considerable proportions of nucleus (single, with several nucleoli) in relation to the cytoplasm stand out. The latter is scarce, bluish in color and lacking in granules..
The megakaryoblast resembles a lymphocyte or other cells of the bone marrow, so its identification, based strictly on its morphology, is complicated.
While the cell is in the megakaryoblast state it can multiply and increase in size. Its dimensions can reach 50 um. In certain cases, these cells can enter into circulation, traveling to places outside the marrow where they will continue their maturation process..
The little promegacario
The immediate result of the megakaryoblast is the promegakaryocyte. This cell grows, until it reaches a diameter close to 80 um. In this state, three types of granules are formed: alpha, dense and lysosomal, dispersed throughout the cell cytoplasm (those described in the previous section).
The basophilic megakaryocyte
In this state it is possible to visualize different granulation patterns and the nucleus divisions are finished. The cytoplasmic demarcation lines begin to be seen more clearly, delineating individual cytoplasmic areas, which will later be released in the form of platelets..
In this way, each area contains inside: a cytoskeleton, microtubules and a part of the cytoplasmic organelles. In addition, it has a glycogen deposit that helps support platelets for a period of time greater than one week..
Subsequently, each fragment described develops its own cytoplasmic membrane where a series of glycoprotein receptors are located that will participate in activation, adherence, aggregation and crossover events..
The megakaryocyte
The final stage of platelet maturation is called a megakaryocyte. These are cells of considerable size: between 80 and 150 um in diameter.
They are located mainly at the bone marrow level, and to a lesser extent in the lung region and in the spleen. In fact, they are the largest cells found in the bone marrow..
Megakaryocytes mature and begin to release segments in an event called a platelet burst. When all platelets are released, the remaining nuclei are phagocytosed.
Unlike other cellular elements, the generation of platelets does not require many progenitor cells, since each megakaryocyte will give rise to thousands of platelets.
Process regulation
Colony stimulating factors (CSF) are generated by macrophages and other stimulated cells participate in the production of megakaryocytes. This differentiation is mediated by interleukins 3, 6, and 11. Megakaryocyte CSF and granulocyte CSF are responsible for synergistically stimulating the generation of progenitor cells..
The number of megakaryocytes regulates the production of megakaryocyte CSFs. That is, if the number of megakaryocytes decreases, the amount of CSF megakaryocytes increases.
Incomplete cell division of megakaryocytes
One of the characteristics of megakaryocytes is that their division is not complete, lacking the telophase and leading to the formation of a multilobed nucleus..
The result is a polyploid nucleus (generally 8N to 16N, or in extreme cases 32N), since each lobe is diploid. Furthermore, there is a positive linear relationship between the magnitude of ploidy and the volume of the cell's cytoplasm. The average megakaryocyte with an 8N or 16N nucleus can generate up to 4,000 platelets
Role of thrombopoietin
Thrombopoietin is a 30-70 kD glycoprotein that is produced in the kidney and liver. It is made up of two domains, one for binding to the megakaryocyte CSF and a second that gives it greater stability and allows the molecule to be durable for a longer time limit..
This molecule is in charge of orchestrating the production of platelets. There are numerous synonyms for this molecule in the literature, such as C-mpl ligand, megakaryocyte growth and development factor, or megapoietin..
This molecule binds to the receptor, stimulating the growth of megakaryocytes and the production of platelets. It is also involved in mediating their release.
As the megakaryocyte develops towards platelets, a process that takes between 7 or 10 days, thrombopoietin is degraded by the action of the platelets themselves.
The degradation occurs as a system that is responsible for regulating the production of platelets. In other words, platelets degrade the molecule that stimulates their development..
In which organ are platelets formed?
The organ involved in this formation process is the spleen, which is responsible for regulating the amount of platelets produced. Approximately 30% of the thrombocytes that reside in the peripheral blood of humans are located in the spleen.
Features
Platelets are essential cellular elements in the processes of stopping bleeding and clot formation. When a vessel is damaged, platelets begin to agglutinate either to the subendothelium or to the endothelium that suffered the injury. This process involves a whole change in the structure of the platelets and they release the content of their granules..
In addition to their relationship in coagulation, they are also related to the production of antimicrobial substances (as we noted above), and through the secretion of molecules that attract other elements of the immune system. They also secrete growth factors, which facilitates the healing process..
Normal values in humans
In one liter of blood, the normal platelet count should be close to 150.109 up to 400.109 platelets. This hematological value is usually slightly higher in female patients, and as age progresses (in both sexes, over 65 years) the platelet count begins to decrease..
However, this is not the number total or full of platelets that the body has, since the spleen is responsible for recruiting a significant number of platelets to be used in an emergency - for example, in the event of an injury or a serious inflammatory process.
Diseases
Thrombocytopenia: low platelet levels
The condition that results in abnormally low platelet counts is called thrombocytopenia. Levels are considered low when the platelet count is less than 100,000 platelets per microliter of blood.
In patients with this pathology, reticulated platelets, also known as "stress" platelets, are usually found, which are markedly larger..
Causes
The decline can occur for various reasons. The first of these is as a result of taking certain drugs, such as heparin or chemicals used in chemotherapies. The elimination of platelets occurs through the action of antibodies.
Destruction of platelets can also occur as a result of an autoimmune disease, where the body forms antibodies against platelets in the same body. In this way, platelets can be phagocytosed and destroyed..
Symptoms
A patient with low platelet levels may present bruises or "bruises" on his body that have appeared in areas that have not received any type of abuse. Along with bruising, the skin may turn pale.
Due to the absence of platelets, bleeding can occur in different regions, often from the nose and gums. Blood can also appear in stool, urine, and when you cough. In some cases blood can pool under the skin.
The reduction of platelets is not only related to excessive bleeding, it also increases the patient's susceptibility to being infected by bacteria or fungi.
Thrombocythemia: high platelet levels
In contrast to thrombocythemia, the disorder that results in abnormally low platelet counts is termed essential thrombocythemia. It is a rare medical condition, and it usually occurs in males over 50 years of age. In this condition, it is not possible to specify what is the cause of the increase in platelets.
Symptoms
The presence of a high number of platelets results in the formation of harmful clots. The disproportionate increase in platelets causes fatigue, a feeling of exhaustion, frequent headaches, and vision problems. In addition, the patient tends to develop blood clots and often has bleeding.
An important risk of blood clots is the development of an ischemic attack or a stroke - if the clot forms in the arteries responsible for supplying the brain.
If the cause that is producing the high number of platelets is known, the patient is said to have thrombocytosis. The platelet count is considered problematic if the numbers exceed 750,000.
Von Willebrand disease
The medical problems associated with platelets are not restricted to abnormalities related to their number, there are also conditions associated with the functioning of platelets.
Von Willebrand disease is one of the most common clotting problems in humans, and it occurs due to errors in the adhesion of platelets, causing bleeding..
Types of pathology
The origin of the disease is genetic and they have been categorized into several types depending on the mutation that affects the patient.
In type I disease, bleeding is mild and is an autosomal dominant production disorder. It is the most common and is found in almost 80% of patients affected by this condition.
There are also types II and III (and subtypes of each) and the symptoms and severity vary from patient to patient. The variation lies in the clotting factor that affects.
References
- Alonso, M. A. S., & i Pons, E. C. (2002). A practical manual of clinical hematology. Antares.
- Hoffman, R., Benz Jr, E. J., Silberstein, L. E., Heslop, H., Anastasi, J., & Weitz, J. (2013). Hematology: basic principles and practice. Elsevier Health Sciences.
- Arber, D. A., Glader, B., List, A. F., Means, R. T., Paraskevas, F., & Rodgers, G. M. (2013). Wintrobe's clinical hematology. Lippincott Williams & Wilkins.
- Kierszenbaum, A. L., & Tres, L. (2015). Histology and Cell Biology: an introduction to pathology E-Book. Elsevier Health Sciences.
- Pollard, T. D., Earnshaw, W. C., Lippincott-Schwartz, J., & Johnson, G. (2016). Cell Biology E-Book. Elsevier Health Sciences.
- Alberts, B., Bray, D., Hopkin, K., Johnson, A. D., Lewis, J., Raff, M.,… & Walter, P. (2013). Essential cell biology. Garland science.
- Nurden, A. T., Nurden, P., Sanchez, M., Andia, I., & Anitua, E. (2008). Platelets and wound healing. Frontiers in bioscience: a journal and virtual library, 13, 3532-3548.



Yet No Comments