
Coagulase test rationale, procedure, and uses

The coagulase test it is a laboratory technique used to reveal the presence of the coagulase enzyme. This enzyme has the property of coagulating plasma. Loeb in 1903 was the first to describe this enzyme.
This test is carried out on Gram positive cocci, catalase positive, allowing to distinguish the strains of Staphylococcus aureus of the rest of the staphylococci, since it is the only microorganism of clinical importance that produces it.
In this sense, members of the Staphylococaceae Family that test negative are often referred to as coagulase negative Staphylococcus..
There are some different strains to S. aureus that can produce coagulase, such as Staphylococcus schleiferi spp coagulans, S. hyicus, S. intermedius and S. delphini.
However, the first three are of clinical importance at the veterinary level and could very rarely be found as a causative agent of infections in humans, while S. delphini it is found only in marine environments.
Furthermore, they are easily differentiated because S. hyicus Y S. intermedius do not ferment mannitol and S. schleiferi spp coagulans does not ferment maltose, nor trehalose, while S. aureus does ferment these carbs.
The presence of the coagulase enzyme has been linked to the virulence of the strains. However, this theory has been falling apart, in view of the fact that other virulent coagulase negative species capable of producing important infections are observed..
Article index
- 1 Rationale
- 2 Procedure
- 2.1 -Slide coagulase test
- 2.2 -Tube coagulase test
- 2.3 -Coagulase test using fibrinogen
- 3 Use
- 4 Quality control
- 5 Limitations
- 6 References
Basis
Staphylococcus aureus produces two types of coagulase, one that remains attached to the cell wall, also called agglutination factor or reactive coagulase factor (CRF), and an extracellular that is released in liquid cultures. That is why they are called bound coagulase and free coagulase respectively..
The coagulase enzyme owes its name to the action it produces. This has the ability to transform fibrinogen into fibrin, creating an evident clot when found in plasma, that is, this enzyme simulates the activity of thrombin in the coagulation cascade.
In fact, one of the most widely accepted theories is that bound coagulase reacts with free coagulase to activate clotting factors. This activation generates a substance that acts in a similar way as prothrombin does, creating a compound with the function of thrombin..
The difference with the normal coagulation cascade is that this reaction does not require the presence of calcium and is not affected by heparin.
To perform the coagulase test, it is enough to face a fresh culture of Staphylococcus with a preferably rabbit plasma and thus observe the formation or not of the clot.
There are specific techniques to detect bound coagulase and bound and free coagulase at the same time..
Some strains of S. aureus they give a positive result faster than others. The rate of clot formation is directly proportional to the concentration of coagulase present..
The slide coagulase test detects bound coagulase and the tube test detects both bound and free coagulase.
Process
-Slide coagulase test
Materials
-Clean slide
-Rabbit plasma preferably, human or horse plasma can also be used. Plasma can be purchased commercially lyophilized and reconstituted for use, or it can be used fresh (fresh). Another viable alternative is the use of fibrinogen.
-Sterile saline (0.85%) (SSF).
Obtaining fresh plasma
Draw venous human or animal blood. Any of the following anticoagulants can be used: EDTA, calcium oxalate, heparin, or sodium citrate. Mix well and centrifuge. Aseptically remove the supernatant (plasma), without red blood cells and place in a sterile tube.

Lyophilized plasma
Reconstitute as specified on the commercial kit vial.
Fresh fibrinogen
Using citrated plasma, mix the plasma in equal parts with a saturated sodium chloride solution. Allow to precipitate and centrifuge.
Discard supernatant, reconstitute the precipitate up to 5 times its volume with sterile distilled water. Add 5 units of heparin for each ml of fibrinogen. Store in a sterile tube.
Technique
A drop of saline solution and a drop of plasma are placed on a slide separately. Take with the platinum loop 1 or 2 pure colonies of the microorganism to be tested.
Mix the bacterial load in the plasma drop and repeat the operation on the SSF drop. Observe the results immediately. A positive result will be one in which the formation of a macroscopic agglutination (white precipitate) is observed after one minute on the side of the drop with plasma.
The SSF drop serves as a negative control. If agglutination is observed with SSF, this means that the microorganism self-agglutinates, which can give false positive results. In this case, it must be corroborated with the tube test.
It is also recommended to mount a positive control with a known strain of S. aureus.
Interpretation
Agglutination within 5-20 sec (strong positive test).
Variable agglutination occurring between 20 seconds and one minute (delayed positive test).
Some degree of agglutination after one minute (doubtful evidence). It is recommended to repeat the test or confirm by the tube method.
No agglutination (negative test).
Result with SSF. It must always give negative, if it automatically gives positive the test result is invalidated.
-Tube coagulase test
Materials
-Sterile test tube
-Plasma
-Water bath at 37 ° C.
Technique
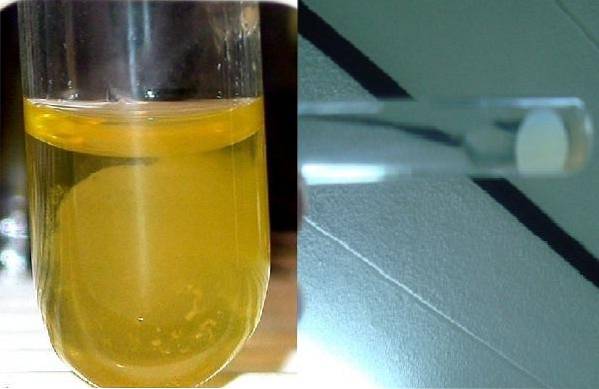
Pipette 0.5 ml of plasma into a 12 x 75 test tube with a sterile pipette. Load the platinum loop with 2 to 4 pure colonies to study from a solid culture for 18 to 24 hours and dissolve in the plasma carefully mix and incubate at 37 ° C for 4 hours.
Examine the tube in the first hour without shaking it, just gently tilt it. If a clot is still not seen, it can be observed every 30 minutes until the 4 hours are completed. If after 4 hours it is still negative, it can be left for up to 24 hours but at room temperature. Observe and report the result.
Based on experience, some microbiologists recommend using 500 µl of a bacterial suspension from an 18-hour culture in liquid medium to perform the test..
It appears to offer faster and more reliable results than when emulsifying colonies from solid media, especially if human plasma obtained from the blood bank has been used..
The use of strains from a broth helps to dilute the possible presence of human anti-staphylococcal antibodies in the plasma that can inhibit the action of coagulase..
Interpretation
If a clot is seen that encompasses all of the fluid (complete clotting) or clot with nothing in the remaining fluid (partial clotting) it should be considered a positive test.
If no clot is formed, that is, the suspension remains homogeneous, the test is negative.
-Coagulase test using fibrinogen
Fibrinogen is used the same as plasma and is suitable for both the slide and tube tests. Proceed as described for plasma and interpret in the same way.
Use
It is used to differentiate the Staphylococcus aureus of coagulase negative staphylococci.
QA
Have fresh cultures of a strain of S. aureus to be used as a positive control. You can also have a strain of S. epidermidis as negative control.
Limitations
-A positive test should not be left in incubation for 24 hours, as the S. aureus produces a fibrinolysin that dissolves the clot.
-For a reliable test, fresh or newly reconstituted plasma should be used, as well as using fresh bacterial cultures (18-24 h). This avoids false negatives.
-The test must be performed in conjunction with a negative and a positive control.
-Some solid media can interfere with the coagulase test. It is not recommended to use colonies from salty mannitol agar.
-If citrated plasma is used, it is recommended to place 5 units of heparin per ml of plasma to avoid false positives. This is because some microorganisms other than S. aureus they can break down citrate and cause plasma to clot. In this case, it is advisable to do a Gram and a catalase test..
-It is important, in the tube test, to monitor the reaction every 30 minutes, as there are strains of S. aureus They produce high concentrations of fibrinolysin and will dilute the newly formed clot quickly. Avoid false negatives.
-When monitoring the test, avoid shaking the tube abruptly, this can destroy the initiation of clot formation that will not be restored later, causing false negatives.
References
- Koneman E, Allen S, Janda W, Schreckenberger P, Winn W. (2004). Microbiological Diagnosis. 5th ed. Editorial Panamericana S.A. Argentina.
- Forbes B, Sahm D, Weissfeld A. (2009). Bailey & Scott Microbiological Diagnosis. 12 ed. Editorial Panamericana S.A. Argentina.
- Mac Faddin J. (2003). Biochemical tests for the identification of bacteria of clinical importance. 3rd ed. Editorial Panamericana. Buenos Aires. Argentina.
- Pro-Lab Laboratories. Rabbit coagulates plasma. Available at: pro-lab.com
- "Coagulase." Wikipedia, The Free Encyclopedia. 12 Feb 2019, 04:23 UTC. 22 Apr 2019, 15:50 wikipedia.org.


Yet No Comments