
Tourniquet test procedure, results, considerations
The tourniquet test The Rumpel-Leede test is a test performed to explore the fragility of a patient's blood vessels. It is a simple, easy-to-perform test, generally used in patients with dengue symptoms..
It consists of placing a loop or an element on the patient's arm that interrupts normal circulation. When small red lesions appear on the patient's skin in a number greater than 30, the test is considered positive.
Although the positivity of the test is not a definitive diagnosis of dengue or any circulatory disease, although it works as a predictor for the possibility of bleeding in this patient.
The tourniquet test is a type of physical examination widely used, especially in health centers where there are not the necessary resources to perform the necessary blood tests that give a diagnosis of a disease that causes bleeding..
Article index
- 1 Tourniquet test
- 1.1 Procedure
- 1.2 Results
- 2 Clinical considerations
- 2.1 Dengue
- 3 References
Tourniquet test
The tourniquet test is a technique used primarily to evaluate diseases that cause capillary fragility or decreased number of platelets in a patient..
The phenomenon that occurs in the patient when the test is positive was described by Dr. Theodor Rumple in 1909 and again in 1911 by Dr. Carl Stockbridge Leede..
At that time, they were conducting studies on patients with scarlet fever or scarlet fever, which is an infectious disease caused by contamination with the bacteria. Streptococcus pyogenes. This condition presents with the appearance of small red skin lesions called petechiae..
Petechiae appear when the smallest blood vessels, called capillaries, become brittle due to disease or when the patient's platelet count is very low. Platelets are responsible for controlling bleeding, therefore when there are not enough, clotting disorders occur.
Process
Ideally, the test should be done with the cuff of a blood pressure meter. For its correct performance, the patient's blood pressure must be measured and the mean arterial pressure (MAP) used as a limit to inflate the cuff and not subject the patient to unnecessary and painful damage to the arm..

For example, knowing that the normal values of mean arterial pressure are between 60 and 80 mmHg, if the patient has a pressure of 120/80 mmHg we can do the test by inflating the cuff up to 70 mmHg.
Although this calculation should be carried out with all the elements that the mathematical formula has (MAP = (cardiac output x systemic vascular resistance) + central venous pressure), the objective of the test is to be a rapid test, so it is calculates an average based on the patient's pressure at the time of the exam.
Once the blood pressure is averaged, the cuff is inflated to that number and waits 5 minutes to deflate it. After two minutes the evaluation of the patient's limb is performed.
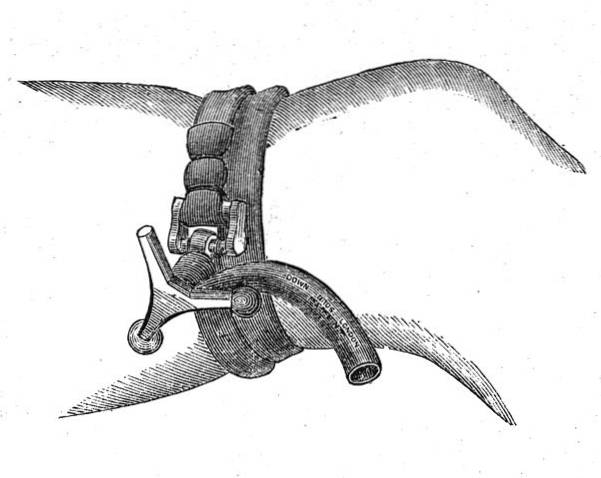
In case of not having the necessary equipment, the examination can be performed with a tourniquet, which is an elastic band with which blood circulation is stopped, with a loop or with any device that can interrupt the flow of blood to the limb of the patient.

Results
When the arm pressure exerted by the cuff, or by the element that has been used, is released, the skin on the patient's limb is evaluated.
If the formation of petechiae is evidenced in a number greater than 30 in an area of 10 cm, or greater than 10 in an area of 3 cm, the test will be positive.
Petechiae are small, point-shaped lesions that are located on the skin. They are flat, millimetric and red in color. Its appearance indicates bleeding due to the fragility of the capillaries, which are the terminal blood vessels of very small diameter.
When capillaries become brittle due to clinical conditions, extravasation of blood cells called erythrocytes occurs. This abnormal outflow of red blood cells into the skin is what causes the appearance of petechiae..
A positive result indicates that the patient has a condition that is causing fragility of the blood vessels or a decrease in the platelet count, which causes disorders in the normal clotting process.
In tropical and subtropical countries it is common to think that dengue is the disease that causes this abnormal clotting process. However, the test can be positive in patients with other conditions such as diabetes mellitus, high blood pressure or scarlet fever, among others..
Clinical considerations
When the tourniquet test is positive, the doctor begins his investigation into the patient's diagnosis..
From the questioning and the background of the person being treated, a particular profile is formed that leads to the diagnostic approach.
If the patient has a history of high blood pressure or some type of hereditary anemia, these may be the cause of capillary fragility.
In a patient with no medical history who presents with fever and weakness, and who has a positive tourniquet test result, dengue infection may be suspected.
Dengue
Dengue is a viral disease transmitted by the bite of a mosquito. It is the most common disease worldwide that is transmitted by the bite of an insect. The exception is in Europe, where it is very rare for cases to occur.
More than one hundred million people suffer the condition annually in the world and it is the cause of 25,000 annual deaths in more than one hundred countries. Dengue deaths occur mainly in children.
It is transmitted by the female species of the mosquito Aedes aegypti, which is commonly located in tropical and subtropical countries. However, it is a rapidly multiplying insect, which is why it is currently a species found in many countries without distinction of climates..

The disease causes, among other symptoms, fever and capillary fragility through a little-known and well-studied mechanism, and can lead to death in the most severe cases of the disease..
References
- Grande, A. J; Reid, H; Thomas, E; Foster, C; Darton, T. C. (2016). Tourniquet Test for Dengue Diagnosis: Systematic Review and Meta-analysis of Diagnostic Test Accuracy. PLoS neglected tropical diseases. Taken from: ncbi.nlm.nih.gov
- Halsey, E. S; Vilcarromero, S; Forshey, B. M; Rocha, C; Bazan, I; Stoddard, S. T; Morrison, A. C. (2013). Performance of the tourniquet test for diagnosing dengue in Peru. The American journal of tropical medicine and hygiene. Taken from: ncbi.nlm.nih.gov
- Mayxay, M; Phetsouvanh, R; Moore, C. E; Chansamouth, V; Vongsouvath, M; Sisouphone, S; Newton, P. N. (2011). Predictive diagnostic value of the tourniquet test for the diagnosis of dengue infection in adults. Tropical medicine & international health: TM & IH. Taken from: ncbi.nlm.nih.gov
- Pacheco Acuña, R; Romero Zúñiga, J. (2008). Tourniquet test as a predictor of spontaneous bleeding in cases of classic dengue due to den-2. Costa Rican Journal of Public Health, 17 (33), 19-23. Taken from: scielo.sa.cr
- Varela, D; Tran, D; Ngamdu, K; Trullender, B; Mukherjee, D; Abbas, A. (2016). Rumpel-Leede phenomenon presenting as hypertensive urgency. Proceedings (Baylor University. Medical Center), 29 (2), 200-201. Taken from: ncbi.nlm.nih.gov
- Schaefer, TJ; Wolford, RW. (2019). Dengue Fever. Treasure Island (FL): StatPearls Publishing. Taken from: ncbi.nlm.nih.gov
- Gubler, D. J. (1998). Dengue and dengue hemorrhagic fever. Clinical microbiology reviews, 11 (3), 480-496. Taken from: ncbi.nlm.nih.gov

Yet No Comments