
What are Endocervical Cells?
The endocervical cells, in the fields of medicine, gynecology and histology, they are those that are usually found in the cervix, more specifically in its mucosa. These cells rapidly degenerate when in contact with agents of various types due to their very low resistance capacity..
Endocervical cells, as their name suggests (note the prefix endo-, that is, "within", "from within", "within", and the cervical noun, of the cervix), are in the internal part of the organs corresponding to the reproductive system of women. This means that these cells are not entirely alone, but are situated within an anatomical context in which they have a definite role in female sexual health..

Therefore, endocervical cells have a relevance that is not limited to the purely biological, since they also have a medical value.
In other words, these cells are evaluated by specialists with advanced diagnostic methods that determine if the woman has health problems. In this way, a better quality of life is guaranteed that, through preventive health procedures, can anticipate various types of ailments.
The endocervix in the female reproductive system
As mentioned before, endocervical cells are not isolated but are part of a whole. Therefore, they are located in a set, in an anatomical context known as the female reproductive system, which is composed of various organs that are closely related to each other..
Among them are the canal of the cervix and what is commonly known as the cervix, which is between the vagina and the uterus itself..
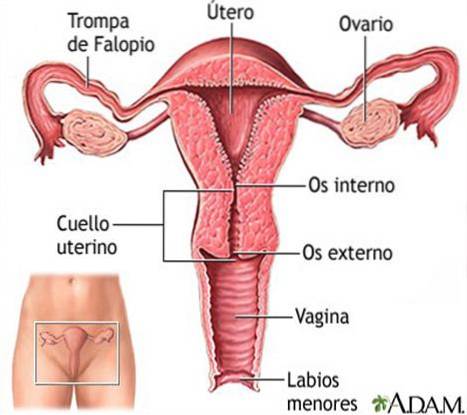
The cervix consists of two parts; an internal one that is the endocervix, which is close to the body of the uterus, and an external one that is the exocervix, which faces the vagina.
In contrast, both the endocervix and the exocervix have more than terminological differences, because they basically differ in the types of cells they contain. While there are glandular cells in the endocervix, squamous cells are present in the exocervix..
The so-called “transformation zone” is nothing but the area where the endocervix and exocervix touch; in fact, this is the meeting point where glandular cells come into contact with squamous cells..
This is where the vast majority of cervical cancer cases have been recorded, which do not develop overnight but over a much longer period of time (hence the need for periodic cytology examinations).
Additionally, the cervix is itself the communication channel between the vagina and the uterus; it is a conduit in which there is an exchange of fluids and consequently of cells of various kinds that interact with each other.
Likewise, secretions take place in the cervix that serve to protect the uterus from infections, hence its two parts - the endocervix and the exocervix - harbor microscopic walls that contain the invasion of these pathogens..
The secretion of cervical mucus, therefore, is not negligible at all and is a true reflection of physiological functions of the female reproductive system that are most normal. Although the frequency of this discharge is continuous, its fluidity, consistency and quantity vary depending on the woman's menstrual cycle and age..
Regarding its shape, the cervix itself looks different in women who had children from those who did not have them or who are in full pregnancy.
In this way, it can be seen that the anatomy and physiology of the organs of the female reproductive system are not as simple as is usually believed, since they have nuances and implications that are not always visible to the naked eye..
If this is how various parts of a woman's sex change due to menstruation, age, pregnancy, and even menopause, then nothing different can be expected in its most recondite aspects, which occur on a microscopic scale, out of sight..
It is clear, then, that women experience changes throughout their lives that affect the cervix both externally and internally. The endocervix is a good example of this because it is a scientifically studied case, in which it has been proven that endocervical cells undergo transformations that obey all the factors mentioned in the previous paragraphs, and whose appearance in the microscope will be variable depending on the sample taken in the cytology.
Importance of endocervical cells
The emphasis has been placed on the study of endocervical cells not only to satisfy the thirst for knowledge in matters of anatomy, but also to aid the development of medicine..
That is, the analysis of these cells is very useful to know if a woman may have cervical cancer or any other related disease, such as genital infections or sexually transmitted diseases. All this is done under laboratory conditions and must be complemented with more specialized tests..
Endocervical cells and cytological tests
It should be noted, however, that the presence of endocervical cells does not by themselves indicate that there is a disorder; what comes out in the tissue analysis in addition to those cells is to set off the alarms: bacteria, viruses and cells with abnormal appearance or amounts. This should be accompanied by other useful information about the woman such as age, family history, children (if they have had them), menstrual rhythm, sexual activity, symptoms of discomfort, among others..
Only the doctor can give a correct interpretation of the results of these tests, which are based on cytology tests such as the papanicolau and the performance of an endocervical culture..
These can be repeated to obtain more precise results or to make sure of the existence / non-existence of these cells and their exact meaning in the tests. Of course, it will be necessary for the patient to go to the gynecologist in order to clarify any doubts she may have in this regard..
References
- Abrahams, Peter H; Spratt, Jonathan D. et al (1977). McMinn and Abrahams' Clinical Atlas of Human Anatomy (7th ed., 2013). Amsterdam, the Netherlands. Elsevier Health Sciences.
- çDrake, Richard; Wayne Vogl, A. and Mitchell, Adam W.M. (2004). Gray's Anatomy for Students (2nd ed., 2009). Amsterdam, the Netherlands. Elsevier.
- Hansen, John T. (2005). Netter's Clinical Anatomy (3rd ed., 2014). Amsterdam, the Netherlands. Elsevier Health Sciences.
- Hughey, Mike (2014). Endocervical Cells [Online article]. Chicago, United States. The Brookside Associates, LLC. Accessed January 30, 2017, at booksidepress.org.
- Jenny, Jacques (No year). Taking a cytological smear in the context of gynecological cancer prevention. Zurich, Switzerland. CSM Graf. Accessed January 30, 2017.
- Pap test results. For Women with an Abnormal Pap Test [Online article] (2014). Melbourne, Australia. Cancer Council Victoria. Accessed January 30, 2017.
- What is cervical (cervical) cancer? [Online article] (2016). Georgia, United States. American Cancer Society. Accessed January 30, 2017, at cancer.org.
- Sacks, Daniel N. (review, 2015). Endocervical culture [Article online]. Maryland, United States. MedlinePlus [Website], US National Library of Medicine. Accessed January 30, 2017, at medlineplus.gov.
Source of the images
- Atlas of Histology. Female Genital System (2013). Mexico, D.F., Mexico. National Autonomous University of Mexico, Faculty of Medicine, Department of Cell and Tissue Biology.
- Vorvick, Linda J. (review, 2016). Uterus [Image hosted online]. Maryland, United States. MedlinePlus. National Library of Medicine of the United States. Accessed January 30, 2017.



Yet No Comments