
What are the Gibbs criteria?
The Gibbs criteria are a series of clinical guidelines that have classically been used to make the diagnosis of chorioamnionitis. Chorioamnionitis is an acute infectious inflammatory process of the placental membranes accompanied by an infection of the amniotic content, that is, of the amniotic fluid, the umbilical cord and / or the fetus..
Chorioamnionitis is also called intra-amniotic infection or amnionitis and can be accompanied by premature rupture of the membranes or amniotic sac and premature delivery. It affects between 2 and 11% of pregnant women and in these cases 5% of fetuses.
Chorioamnionitis should always be suspected when the pregnant woman presents with a fever with no other apparent source of infection..
Chorioamnionitis is an important cause of maternal-fetal morbidity and mortality. For the mother, it is associated with an increased risk of adult respiratory distress, sepsis, postpartum hemorrhage, hysterectomy, and mortality. For the fetus, the risk of low APGAR score, sepsis, hemorrhage, premature birth, neurodevelopmental disturbances and fetal death increases..
Although the Gibbs criteria allow a clinical diagnosis of this pathology, other tests, mainly amniocentesis (taking a sample of amniotic fluid), allow to corroborate the diagnosis, identify the germ and establish an adequate therapy.
Article index
- 1 Gibbs clinical criteria
- 2 Other diagnostic criteria
- 3 Treatment
- 3.1 Standards of asepsis
- 4 References
Gibbs clinical criteria
In 1982, Gibbs et al. Reported a series of clinical criteria that allow the diagnosis of chorioamnionitis. These criteria are still in force, although they have been modified and supplemented.
Gibbs Clinical Criteria:
- Appearance of maternal fever greater than or equal to 37.8 ° C. (Currently ≥ 38 ° C)
The above criteria and two or more of the following:
- Fetal tachycardia greater than 160 beats / minute.
- Maternal leukocytosis greater than 15,000 leukocytes / mm3.
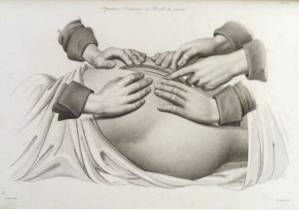
- Uterine irritability manifested by pain on palpation or with fetal movements and / or with uterine contractions.
- Vaginal leukorrhea or foul-smelling vaginal discharge.
Some of these criteria are very nonspecific and allow the suspicion of chorioamnionitis, but they must be confirmed by means of amniocentesis.
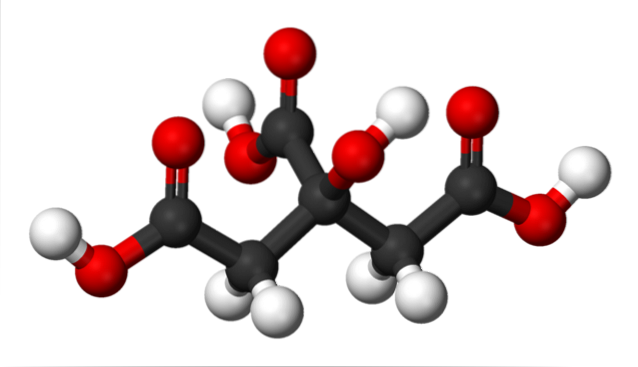
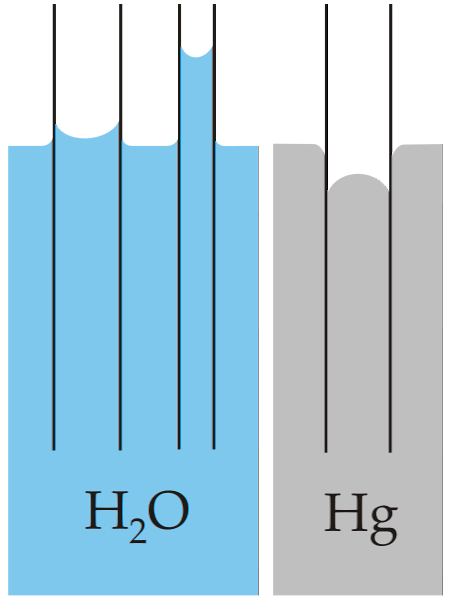
In amniocentesis, a biochemical study of the amniotic fluid is carried out to measure glucose and the presence of leukocytes and a microbiological study with Gram stain, in addition to a culture and antibiogram, for aerobic and anaerobic microorganisms..
In cases where amniocentesis cannot technically be performed, such as when the sacs have ruptured and anhydramnios is present, the Gibbs criteria are the ones that can guide the diagnosis..
Other diagnostic criteria
In some cases, even if the Gibbs criteria are not met, chorioamnionitis may be suspected when the mother has a persistent fever with no other apparent focus, signs of uterine irritability, and increased C-reactive protein (CRP). In these cases, some paraclinical tests can help confirm the diagnosis..
Blood count and C-reactive protein show leukocytosis and increased CRP.
Amniocentesis can show very low glucose levels (less than 5%), germs can even be seen with the Gram stain. Once the amniocentesis is done, a culture and antibiogram of the sample will be indicated. This can confirm the diagnosis of chorioamnionitis..
Non-stress fetal cardiotocography (NST) tests can show, in these cases, very high fetal heart rates (more than 160 x minute) and irritating uterine dynamic activity that does not respond to tocolytics..
Another test that allows evaluating the fetal state is the so-called “fetal biophysical profile”, which is a real-time sonographic test that allows evaluating the spontaneous movements of the fetus, respiratory movements, muscle tone and amniotic fluid. The biophysical profile in these cases is altered.
If the maternal temperature, with no other apparent source of infection, is greater than or equal to 38 ° C, a blood culture is indicated.
Treatment
Once the clinical diagnosis of chorioamnionitis has been confirmed, the pregnancy should be interrupted regardless of the gestation age and antibiotics should be administered. Amnionitis is not an indication for caesarean section. Cesarean section will be performed only under obstetric indications.
Vaginal delivery is a much safer route, since it represents a lower risk for the mother. During vaginal delivery, continuous fetal monitoring and antibiotic treatment of the mother should be maintained. The time until delivery should not exceed 12 hours.
The antibiotics of choice initially are:
- Gentamicin: 1.5 mg / kg IV as a starting dose to follow with 1 mg / kg IV every 8 h (if there is no renal involvement).
- Clindamycin: 900 mg IV every 8 h.
- Penicillin: 3,000,000 IV units every 4 h.
- Vancomycin: 15 mg / kg and piperacillin / tazobactam 4.5 g IV every 6 h.
Treatment is maintained until after delivery. If after delivery the fever persists, continue the treatment and the modifications will be made according to the results of the cultures and antibiograms already indicated..
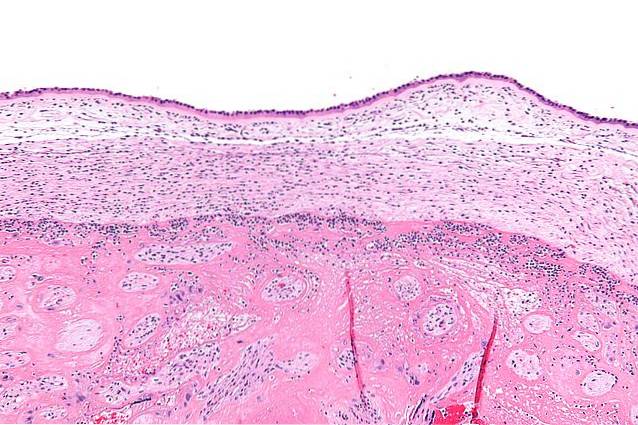
After delivery, a sample of the placenta will be taken for culture and an anatomopathological study of the same will be indicated..
Asepsis standards
If there is a formal indication to terminate the pregnancy with caesarean section, certain special aseptic rules must be followed during surgery to avoid contamination of the extrauterine tissues. These standards include the following:
- Compresses should be used to prevent contaminated amniotic fluid from draining out of the uterus.
- The use of the electrosurgical unit should be restricted.
- All areas or tissues that may have been contaminated and infected should be thoroughly washed.
- The surgeon must change the gloves to proceed to the closure of the abdominal wall.
- There are no advantages in terms of the different approaches to cesarean section, since the incidence of infections in these cases is the same.
- In the postoperative period and for a period of at least 7 days, antibiotic therapy should be maintained..
Since the greatest risk factor for fungal amnionitis is pregnancies with IUD or cerclage, in these patients fluconazole 400 mg / day IV should be added to the antibiotic treatment..
Depending on the weeks of gestation (30 to 33 weeks), treatment will be placed to promote lung maturation of the fetus. In these cases, if possible, you should wait 48 hours before terminating the pregnancy to be able to place two doses of betamethasone..
References
- Cunningham, F., Leveno, K., Bloom, S., Spong, C. Y., & Dashe, J. (2014). Williams obstetrics, 24e. Mcgraw-hill.
- Espitia-De la Hoz Franklin J. (2008) Diagnosis and treatment of clinical chorioamnionitis. Colombian Journal of Obstetrics and Gynecology Volume 59 No. 3
- Kasper, D. L., Hauser, S. L., Longo, D. L., Jameson, J. L., & Loscalzo, J. (2001). Harrison's principles of internal medicine.
- McCance, K. L., & Huether, S. E. (2018). Pathophysiology-Ebook: the biologic basis for disease in adults and children. Elsevier Health Sciences.
- Oats, J. J., & Abraham, S. (2015). Llewellyn-Jones Fundamentals of Obstetrics and Gynaecology E-Book. Elsevier Health Sciences.
- Phelan, J. P. (2018). Critical care obstetrics. John Wiley & Sons.

Yet No Comments