
Patellar or patellar reflex how it occurs, physiology, absence
The patellar or patellar reflex It consists of the involuntary contraction of the quadriceps femoris muscle, and therefore the extension of the leg, in response to a stimulus that consists of stretching said muscle by means of a blow applied to its tendon below the patella.
The tendon is a relatively rigid tissue and the blow does not stretch it, but undergoes a deformation that consists of a depression or sinking that transmits traction to the more elastic tissues that make up the muscle, which undergo a sudden and brief stretching.

Among the stretched elements are sensory receptors that react to this physical stimulus and send a nerve signal to the spinal cord, in which a direct connection is established with the motor neurons that innervate the quadriceps, which when activated produce the contraction of said quadriceps. muscle.
In this video you can see this reflection:
And here is how the nerve impulse reaches the spinal cord:
Article index
- 1 The reflex arc
- 2 How does the knee jerk reflex occur?
- 3 Physiology
- 3.1 Neuromuscular spindle
- 3.2 Central connections of the afferent fibers
- 3.3 Spinal cord and efferent pathways
- 3.4 Reflex function
- 3.5 Function during voluntary movement
- 3.6 Muscle tone
- 4 Absence of patellar reflex (possible causes)
- 5 References
The reflex arc
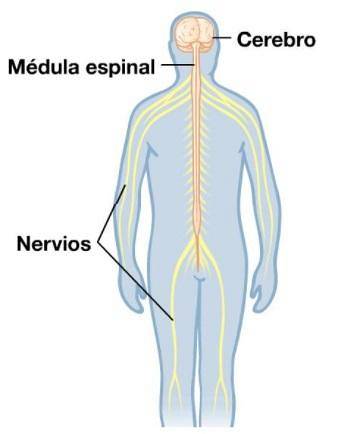
The organization of the elements involved in this stimulus-response association obeys the concept of reflex arc, which is the anatomical-functional unit of the nervous system. It is made up of receptors that detect stimuli or energetic variations, an afferent sensory pathway, an integrating nervous center, an efferent pathway and an effector that emits a final response..
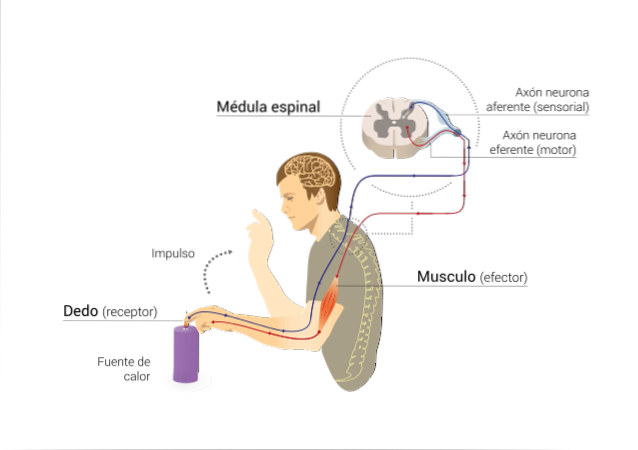
The name afferent or efferent for the nerve pathways is related to the direction of the flow of excitation that they transmit. If this is directed to the central nervous system, then the nerve pathway is said to be afferent. If the excitation is directed towards the periphery, away from the central nervous system, then the pathway is efferent.
According to the number of synapses that are established one after another in the medullary integrating center from the entry of the afferent fiber until the information exits through the efferent pathway, the reflexes can be monosynaptic, bisynaptic and polysynaptic.
In the course of the physical examination, the physician examines some basic reflexes, including the patellar reflex. When applying the appropriate stimulus, the examiner observes whether or not there is a response to the stimulus and its degree. If the appropriate response occurs, the clinician is confident that all components of the reflex arc are intact and healthy..
How does the knee jerk reflex occur?
When the patellar or patellar reflex is to be revealed, the person to be examined sits on a table with the legs dangling and flexed over the edge of the table. The feet must not touch the floor, that is, they must not be supported but free so that the lower limb is relaxed and allows free pendulum movement.

The examiner takes a reflex hammer, palpates the quadriceps tendon, and just below the kneecap applies a sharp blow while distracting the patient with some conversation. As a result of this stimulus, the tendon is stretched by the deformation inflicted by the blow and this stretch is also transmitted to the muscle..
Within the muscle there are stretch receptors called neuromuscular spindles that are connected to an afferent fiber. As the spindles are stimulated by the stretch generated by the blow to the tendon, the afferent fiber is stimulated and carries the information to the spinal cord.
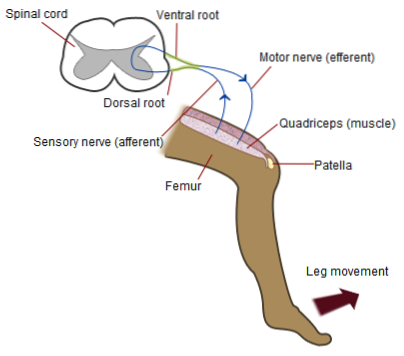
The spinal cord is the integrating center and there the afferent fiber makes direct synapses with the efferent neuron, which is a fast transmitting alpha motor neuron that innervates the quadriceps and stimulates the muscle that consequently contracts..
This contraction cannot be voluntarily inhibited, it is an automatic and involuntary contraction. The reflex is monosynaptic, it is a myotatic reflex and is called the osteotendinous or proprioceptive reflex, it is a stretch reflex.
Physiology
First, each of the components of the patellar reflex arc will be described and then its physiological function will be explained..
Neuromuscular spindle
The neuromuscular spindle is a stretch receptor for skeletal muscle. It is composed, on average, of about 10 specialized muscle fibers (cells) packaged in a connective tissue capsule. They are in a parallel arrangement to the contractile fibers of the muscle.
The spindle fibers are called intrafusal fibers to distinguish them from contractile fibers outside and around the spindle which are called extrafusal fibers. The intrafusal fibers of the neuromuscular spindles of mammals are of two types: nuclear sac fibers and nuclear chain fibers.
Nuclear sac fibers have a dilated, bag-like region filled with nuclei. Nuclear chain fibers are thinner, have no pockets, and their cores are arranged in a row within the fiber..
There are about four fibers in a nuclear chain and about two in a nuclear bag for each spindle. The nuclear chain fibers are attached at each end to the nuclear bag fibers. The central portions of both types of fibers are not contractile while their distal portions are..
The spindles have a sensitive ending called primary or annulospiral and a secondary arborescent one. The primary endings are fast conducting “Ia” nerve fibers that divide into two branches upon entering the spindle. One branch wraps in a spiral around the nuclear sac or bag and the other around the nuclear chain.
Secondary endings are slower conducting type "II" sensory fibers. The contractile portions of the spindle have their own motor innervation through efferent motor fibers γ or “small motor fibers”, these innervate both types of intrafusal fibers.
Central connections of afferent fibers
Sensory afferent fibers are axons belonging to bipolar neurons whose nuclei are found in the ganglia of the dorsal root of the spinal cord. These axons enter the medulla through the posterior roots.
Experimentally it can be proved that this reflex is monosynaptic. Thus, the sensory fibers connect directly with the motor neurons, in the anterior roots of the spinal cord, whose axons innervate the extrafusal fibers..
This is done by measuring the reaction time of the reflex and subtracting the afferent and efferent conduction times, which are calculated based on the known speed of transmission of the fibers involved and the distance traveled between the spinal cord and muscle..
The difference between these two times corresponds to the synaptic delay, that is, the time it takes for electrical activity to travel through the marrow. As the minimum delay time of a synapse is already known, if these times coincide, it means that there was only one synaptic contact..
If these times are longer, it means that there was more than one synapse and thus the number of synaptic contacts for each reflex can be calculated.
Spinal cord and efferent pathways
The spinal cord is a very orderly structure, its posterior horns receive the axons of the sensory neurons and therefore the posterior horns are said to be sensitive. The anterior horns contain the bodies of the motor neurons that will innervate most of the skeletal muscles..
These neurons are called alpha motor neurons, and their axons exit through the anterior horns of the spinal cord. They join or bundle to form the different nerves that supply the extrafusal fibers of the corresponding muscles.
Also found in these anterior horns are γ-motor neurons, which send out their axons to innervate the contractile portions of the spindles..
Reflex function
When the quadriceps femoris tendon deforms, the quadriceps femoris muscle to which the quadriceps femoris belongs is stretched. As the spindles are arranged in parallel with the extrafusal fibers, as these fibers stretch, the spindles also distend.
The distention of the neuromuscular spindle deforms the annulospiral or primary endings of the spindle, which generates a receptor potential that ends up producing a discharge of action potentials in the afferent fiber.
The frequency of action potentials generated in the afferent fiber is proportional to the degree of stretching of the primary end of the spindle. These action potentials end up promoting the release of a neurotransmitter at synaptic terminals on the body from the alpha motor neuron..
This neurotransmitter is a stimulator. Therefore, the alpha motor neuron is excited and discharges action potentials through its axon, which ends up activating the extrafusal fibers and causing the muscle that underwent the stretch to contract..
The contraction of the stretched muscle produces a shortening of the extrafusal fibers and also a reduction in the distension of the intrafusal fibers, with which their stretching ceases and the triggering stimulus of the reflex disappears.
Function during voluntary movement
During voluntary muscle contraction, the neuromuscular spindles allow the central nervous system to keep informed about the length of the muscle during the course of contraction. To do this, the ends of the intrafusal fibers contract, stimulated by the γ motor neurons..
This keeps the spindle stretched despite the fact that the extrafusal fibers are contracted and shorter in length. In this way, the sensitivity of the spindle is maintained and the contractile activity is reinforced..
The activity of the γ-motor neurons is controlled in turn by descending pathways that come from different brain areas. This allows to regulate the sensitivity of the neuromuscular spindles and the threshold of stretch reflexes..
Muscular tone
Another function of the gamma motor neuron system across the neuromuscular spindles is to maintain tone. Muscle tone is a smooth and sustained or permanent contraction that can be defined as resistance to stretching..
If the motor nerve of a muscle is cut, it becomes flaccid without tone, since the reflex circuit cannot be completed.
Absence of patellar reflex (possible causes)
The absence of patellar reflex implies a lesion in some of the anatomical components of the patellar reflex arc. Lesions can be located in the sensory afferents, in the spinal cord, or in the efferent motor pathways..
Lesions of the spinal nerves or of the bodies of the spinal motor neurons or lower motor neurons between the lumbar segments L II and L IV (as for example in polio) produce an abolition of the patellar reflex and a flaccid paralysis.
The characteristic is the abolition of stretch reflexes, loss of muscle tone and atrophy of the affected muscles, in this case the quadriceps femoris among others..
In contrast, injury to upper motor neurons or descending motor pathways causes spastic paralysis, characterized by increased muscle tone, exacerbation of stretch reflexes, and other signs of lower motor neuron overactivity..
References
- Barrett, K. E. (2019). Ganong's review of medical physiology (No. 1, pp. 1-1). : McGraw Hill Education.
- Fox, S. (2015). Human physiology. McGraw-Hill Education.
- Hall, J. E. (2010). Guyton and Hall textbook of medical physiology e-Book. Elsevier Health Sciences.
- Iatridis, P. G. (1991). Best and Taylor's Physiological Basis of Medical Practice. JAMA, 266(1), 130-130.
- Widmaier, E. P., Raff, H., & Strang, K. T. (2006). Vander's human physiology (Vol. 5). New York, NY: McGraw-Hill.



Yet No Comments