
Safenectomy what it consists of, complications and recovery
The saphenectomy It is a surgical procedure in which the great saphenous vein is ligated and removed. This large vein crosses the entire lower limb on its anterior and internal face, from the dorsum of the foot to the groin where it ends up draining into the femoral vein..
It is used for the purpose of treating varicose disease and as a procedure in autotransplantation for coronary revascularization, one of the most performed procedures in cardiac surgery (taking segments of the saphenous vein to bypass or bypass obstructed coronary arteries).

By FerIndigo97 [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], from Wikimedia Commons
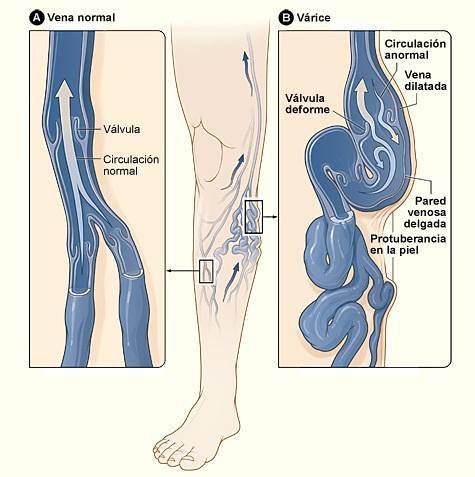
Varicose disease (or varicose veins) is a disorder in which the veins of the lower limbs become swollen and dilated. It is mainly caused by valve incompetence secondary to venous disease.
To solve this situation there are several types of interventions and procedures; however, saphenectomy continues to be the gold standard in treatment.
Article index
- 1 What does?
- 1.1 Indications
- 2 The technique
- 3 Complications
- 3.1 Skin
- 3.2 Vascular
- 3.3 Neurological
- 3.4 Others
- 4 Recovery
- 5 References
What does it consist of?
It consists of completely removing the saphenous veins, both internal and external. Of the veins of the lower limb, the saphenous are the most prone to form varicose veins because they are very superficial.
Indications
Several causes lead to the decision to perform this procedure:
- Varicose vein thrombosis. It happens when clots form inside them, preventing normal blood flow.
- Phlebitis. Inflammation of the veins due to clots and thrombi.
- Bleeding. Due to the high probability that dilated and inflamed veins will rupture.
- Venous ulcers. A broken varicose vein takes a long time to heal and can lead to ulcers, more often in people with diabetes..
- Pigmentations and skin disorders. Which is the only aesthetic indication for saphenectomy.
The technique
The procedure was initially described by Babcock in 1907 and later modified by Myers in 1947, when he devised the elastic phleboextractor. It must be performed in the operating room by a general, cardiovascular, angiologist or phlebologist surgeon.
Local or spinal anesthesia is placed on the patient (or general, according to the anesthesiologist's indication) and the surgeon proceeds to make an incision in the inguinal fold and to tie the vein at the level of its outlet in the femoral vein..
A similar procedure is then performed near your birth on the back of the foot (usually at the ankle level)..
Subsequently, the entire course of the vein is dissected with the help of the vein extractor (which allows the path of the vein to be followed from the foot to the thigh) and finally its removal. This is the classic procedure.
After the excision, the skin is sutured and a compression bandage is placed that will be kept for 1 to 2 weeks. The surgical procedure has an average duration of about 90 minutes.
The patient is regularly discharged 24-48 hours after the intervention, depending on the existence or not of comorbidities (diabetes, heart disease, etc.).
In some centers it is an outpatient procedure and the patient is discharged the same day. There are many alternative techniques that have been developed over time by virtue of medical and technological advances..
Even so, saphenectomy continues to be the standard procedure for the treatment of varicose veins, preferably with the 3S modification, in which classic saphenectomy is combined with sclerotherapy.
By National Heart Lung and Blood Institute (NIH) [Public domain], via Wikimedia Commons
Complications
Most complications are associated with immunosuppression secondary to diabetes, advanced age, failure of other organs (liver and kidney), use of inhaled or systemic steroids, malnutrition, and decreased local blood supply..
Complications of saphenectomy impact prolonged hospital stay, increased costs, reoperations, and even loss of the limb.
They can be classified according to the time of appearance of complications (immediate, mediate and late) or according to the compromised system, which is the one that functionally seems most appropriate..
Cutaneous
- Postoperative infection of the saphenectomy area in up to 25% of patients in some studies.
- Transient pigmentation of the surgical tract.
- Induration of the area, product of the manipulation and as an inflammatory response perhaps to the powder of the gloves.
- Rejection and / or leakage of suture material.
- Necrosis due to local anesthesia.
- Pathological scar (keloids).
- Seromas.
Vascular
- Residual varicose veins and microvarices (telangiectasias and reticular varices).
- Bruising, from the use of heparin during the procedure.
- Postoperative hemorrhage due to incorrect bandage.
- Superficial phlebitis.
- Lower limb edema.
- Lymphatic pseudocyst (rare).
Neurological
- Paresthesias and / or dysesthesias. Average duration: 1 year.
- Intense, sudden or lacerating neurogenic pain in the leg and / or the back of the foot refractory to analgesic treatment. Average duration: 1 year.
- Deep nerve anesthesia due to poorly administered local anesthesia.
- Feeling of flaw.
Others
- Pulmonary embolism.
In the same way, relapses (or reappearance) at 5 years are not frequent, so it is a really effective treatment..
Recovery
During the saphenectomy recovery process, once the bandage is removed, the patient should take 15-minute walks every hour.
The use of elastic compression stockings that go from the roots of the fingers to the groin is suggested for at least 4 weeks after the removal of the bandage. These will be worn during the day and removed at night.
Additionally, the patient will be kept lying down resting the limbs up. Conventional analgesia (paracetamol, or any anti-inflammatory analgesic) is indicated, in addition to phlebotonic drugs and subcutaneous anticoagulants.
Specific management of the different complications is beyond the coverage of this article..
References
-
- Ortiz Tarín, Immaculate. Twelve-year evolution of the 3-S Safenectomy technique: Study of varicose recurrence. Doctoral Thesis. Valencia Spain. 2014.
- Córdova-Quintal P et al. Efficacy of management in chronic venous disease with USG-guided sclerotherapy and crosectomy compared with conventional saphenectomy in the Angiology and Vascular Surgery Service, in the Regional Hospital Lic. Adolfo López Mateos. Rev Mex Angiol 2013; 41 (1): 25-29.
- Sánchez-Beorlegui J, Arribas-Cerezo A. et al. Surgical treatment of venous insufficiency in the territory of the external saphenous vein. Rev Mex Angiol 2018; 46 (2): 68-75.
- Sánchez-Beorlegui J, Arribas A. et al. Short versus long safenectomy in the treatment of primary varicose veins of the lower limbs. Rev Colomb Cir. 2018; 33: 181-8.
- Rodriguez, Carlos. Varicose disease: treatment techniques. Rev Colomb Cir. 1998; 13 (2): 114-120.
- Selles R, Arenas J et al. Phlebectomy or foam sclerosis for the treatment of the distal venous segment in the 3-S saphenectomy technique. Cir Esp 2008; 84 (2): 92-99.
- Silva L, Buitrago A, Maldonado J et al. Infection rate at the surgical site in myocardial revascularization surgery at the Fundación Santa Fe de Bogotá. Rev Colomb Cardiol 2011; 18: 158-161.
- Payró LE, Carmona GA et al. Saphenectomy complications in patients undergoing myocardial revascularization surgery. Cir Gen 2012; 34 (2): 125-129.


Yet No Comments