
Cullen's sign symptoms, causes, treatment
The cullen sign It is a clinical symptom that presents a purple or violet color and that can be found in the central part of the abdomen, in the periumbilical skin. It is visible on physical examination, is not particularly painful, and is indicative of bleeding from an organ within the abdominal cavity.
The hematoma forms in the umbilical region when the blood reaches the round ligament of the liver, which communicates that organ with the navel. This sign occurs in serious and life-threatening illnesses.

The most common disease in which the patient manifests it is acute necrotizing pancreatitis, but only when the head of the pancreas is affected. It can also be present in women with a ruptured ectopic pregnancy. In this type of pregnancy, the embryo usually implants in the uterine tubes..
Cullen's sign is associated with another with similar characteristics, Gray Turner's sign, which is the violet coloration of the skin on the flanks of the abdomen..
Article index
- 1 Description and pathophysiology
- 1.1 Pathophysiology
- 2 Associated pathologies
- 2.1 Acute pancreatitis
- 2.2 Others
- 3 Treatment
- 4 References
Description and pathophysiology
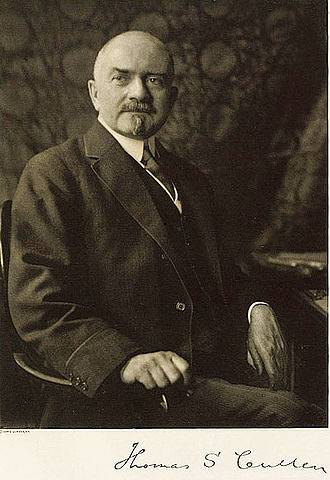
Cullen's sign was described in by Canadian gynecologist Dr. Thomas S. Cullen at John Hopkins Hospital in Baltimore, USA..
Cullen devoted much of her professional life to the study of uterine cancer and ectopic pregnancy. In 1918 he received a 38-year-old patient who reported abdominal pain of 3 weeks of evolution.
One week after the onset of abdominal pain, he reported the appearance of a bluish color around the navel without having suffered trauma in this area..
In his article “A New Sign in Broken Ectopic Pregnancy,” Dr. Cullen described it as follows: “The bluish appearance of the navel that is not associated with trauma along with a para-uterine mass, completes the diagnosis of extra-uterine pregnancy almost with certainty.".
Since that publication, the violet or bluish discoloration of the umbilicus related to bleeding within the abdominal cavity has been called Cullen's sign, regardless of the etiology..
Cullen's sign is a rare manifestation that is present in less than 5% of patients with intra-abdominal bleeding. However, in those cases in which it is observed it is indicative of serious disease.
It is associated with another skin sign, the Gray Turner sign. In this case, the hematoma is found on the lateral part of the abdomen, the flanks, and is found in patients with retroperitoneal bleeding, that is, in those cases in which the bleeding organ is located behind the layer that covers the abdomen..
Both the Gray Turner and Cullen signs are commonly associated with necrotizing hemorrhagic pancreatitis, although they can be present in various pathologies; and it is very bad prognosis to find both in the same patient.
Pathophysiology
The violet or bluish coloration, characteristic of Cullen's sign, is observed in the umbilicus due to bleeding within the abdomen that reaches the falciform ligament of the liver.
This structure communicates with the navel through the round ligament of the liver, which is a vestige of the umbilical vein of the fetus which after birth is completely closed, giving rise to this element.
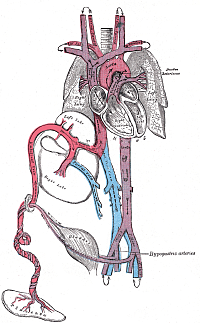
In the case of patients with necrotizing pancreatitis, there is the presence of inflammatory fluid around the pancreas which contains enzymes that degrade the tissue and are capable of penetrating the muscle until reaching the subcutaneous cellular tissue of the navel..
The bluish color, typical of bruises, normally forms when hemoglobin breaks down.
Associated pathologies
Acute pancreatitis
Acute pancreatitis is inflammation of the pancreas as a result of an exaggerated activation of pancreatic digestive enzymes.
It is mainly associated with obstruction of the pancreatic duct outlet to the duodenum caused by stones or lithiasis stuck in the bile duct.
In its acute phase, the patient with pancreatitis refers to pain that is located in the epigastrium and, as time passes, the abdomen and back are taken at that level. This symptom is described as band abdominal pain and is typical of pancreatitis.
One of the complications of acute pancreatitis is hemorrhagic necrotizing pancreatitis. It occurs in 10% of cases of acute pancreatitis.
It occurs when digestive enzymes continue the process of self-digestion of pancreatic tissue despite treatment, causing necrosis of the pancreatic surface.
Cases of acute pancreatitis with severe necrosis can lead to the installation of serious complications in the patient including diabetes. In 30% of cases, hemorrhagic necrosis of the pancreas is fatal.
Hemorrhagic necrotizing pancreatitis is usually located in the body and tail of the pancreas, but it can also reach the head of that organ.
When the necrosis reaches the area of the head of the pancreas, the Cullen's sign can be evidenced. In most cases in which there are cutaneous manifestations, the sign of Gray Turner is observed.

The presence of both signs indicates that the entire pancreatic parenchyma is compromised. This situation can bring serious consequences to the patient including diabetes and even death.
In general, pancreatitis is a self-limited condition, this means that it does not need specific treatments since the improvement occurs by itself.
Patients must be hospitalized in an intensive care unit (ICU) to monitor their fluid balance. They should stay hydrated and in pain control.
The treatment depends on the cause. When stones are obstructing the passage of pancreatic fluid into the duodenum, an invasive procedure must be performed to remove the stones and allow that fluid to resume its normal course..
So that the pancreas can rest from its work in digestion, the administration of nutrition through the vein or parenteral nutrition is indicated.
In the case of necrotizing pancreatitis, antibiotics should be indicated to avoid the formation of peri-pancreatic abscesses..
When there is very extensive necrosis or large abdominal abscesses have formed, surgical drainage is chosen. This procedure is reserved for cases in which non-invasive techniques have failed..
Others
Other associated pathologies are ectopic pregnancy and abdominal trauma..
Treatment
Cullen's sign is not a pathology as such, but the physical evidence of a primary disease of the abdomen.
In the event that the bruise becomes hard, painful or contaminated, appropriate medications should be administered for each of these complications..
Gel or cream anticoagulants can improve hardening by helping to finish dissolving the clot.
In the case of pain, it can occur when the bruise covers a very large area. Nonsteroidal pain relievers, such as aspirin and diclofenac, generally improve pain.
The most serious complication is contamination of the hematoma by bacteria. When the bruised area becomes warm and the skin is very sensitive, it is very likely that there is infection.
In these cases, the intravenous administration of antibiotics should be started immediately and thus avoid other associated pathologies such as cellulitis, abscess and even skin necrosis..
References
- Bendersky, V. A; Mallipeddi, M. K; Laziness; Pappas, T. N. (2016). Necrotizing pancreatitis: challenges and solutions. Clinical and experimental gastroenterology. Taken from: ncbi.nlm.nih.gov
- Mookadam, F; Cikes, M. (2005). Images in clinical medicine. Cullen's and Turner's signs. N. Engl. J. Med. Taken from: ncbi.nlm.nih.gov
- Birnaruberl, C.G; RiBe, M; Kettner, M; Schnabel, A; Ramsthaler, F; Verhoff MA. (2016). So-called skin signs in acute pancreatitis. Taken from: ncbi.nlm.nih.gov


Yet No Comments