
Syncytiotrophoblast characteristics, function, placental apoptosis
The syncytiotrophoblast It is a multinucleated cytoplasmic mass that forms the outer layer of the trophoblast and contacts maternal tissue. This cell layer is found invading the epithelium and stroma of the endometrium during embryonic development of mammals. The cells that make up the syncytiotrophoblast fuse with each other, losing their cell membranes.
This layer of cells originates from cell differentiation of the cytotrophoblast and is responsible for the exchange of gases and nutrients between the mother and the fetus. In addition, it is capable of producing hormones and peptides in the implantation phase of the blastocyst to the endometrium and the formation of the placenta..
Article index
- 1 Features
- 2 Role in embryonic development
- 2.1 Nidation or implantation
- 2.2 Utero-placental circulation
- 3 Placental apoptosis
- 3.1 Apoptosis and preeclampsia
- 3.2 Evidence of the relationship between apoptosis and preeclampsia
- 4 References
Characteristics
As its name indicates, the syncytiotrophoblast cells have lost their membranes and fused, giving this cell layer a multinucleated syncytial-like appearance..
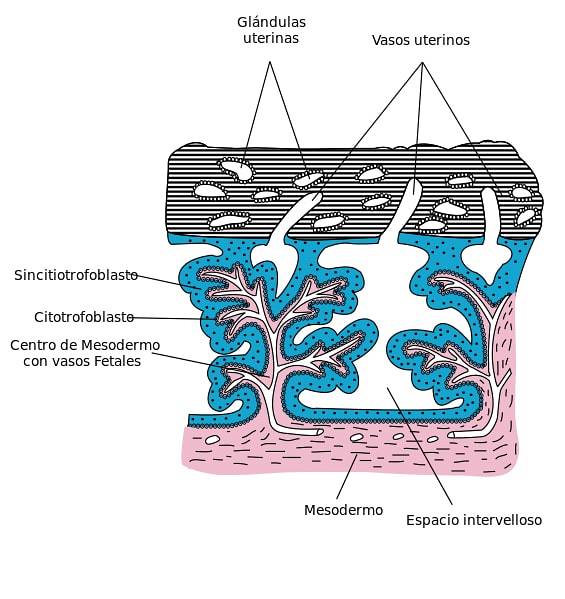
These cells continuously cover the chorionic villous surface, the decidua basalis and the chorionic plate and form part of the placental barrier that is responsible for separating the mother's and fetal blood.
The syncytiotrophoblast originates from the proliferation and fusion of cytotrophoblast cells. The cells of this layer do not have proliferative capacity, that is, they do not undergo mitosis, so the expansion and maintenance of this cell layer depends only on the continuous incorporation of cells from the cytotrophoblast, ensuring its functionality..
These cells have Golgi complexes and abundant smooth and rough endoplasmic reticulum, as well as a large number of mitochondria and lipid inclusions..
This layer of cells also has a secretory function, releasing progesterone, estrogen, human chorionic gonadotropin (hCG) and lactogens. As the cellular material ages, it is wrapped in a protective membrane and discarded through the maternal circulation..
Role in embryonic development
Nidation or implantation
The blastocyst joins the endometrium initiating a stage of rapid cell proliferation, with the differentiation of the trophoblast into cytotrophoblast and syncytiotrophoblast. The latter extends through the endometrial epithelium until reaching its stroma, where the cells fill with lipids and glycogen, becoming decidual cells..
These decidual cells undergo degenerative processes that allow them to provide nutrients to the developing embryo..
Once the blastocyst is implanted in the endometrium by the implantation or nesting process, the fusion of the outermost cells of the trophoblast, give rise to the primitive syncytiotrophoblast.
Later, lagoons are formed occupied by glandular secretions of the endometrium that will later be replaced by maternal blood, by weakening the capillary vessels and endometrial venules..
These intracellular gaps filled with maternal blood define the lacunar or trabecular phase and extend until they reach the opposite side of the implantation site..
The gaps in the syncytiotrophoblast are called trabeculae. Embryogenesis, which consists of changes in the embryoblast inside the blastocyst, also occurs at this stage.
Utero-placental circulation
One of the fundamental functions of the syncytiotrophoblast is the metabolic exchange between the mother and the fetus, demonstrating a high endocrine activity and participating in the homeostasis of embryonic development..
The appearance of intracellular or trophoblastic gaps in the syncytiotrophoblast initiates the development of the utero-placental circulation. Sinusoids derived from the capillaries of the maternal portion of the placenta flow into these lagoons..
A directional flow is formed by the differential pressure between the circulatory vessels and the trophoblastic lagoons. This flow goes from the arteries to the veins, forming the primitive utero-placental circulation..
There is a transfer of nutrients from the maternal vessels to the embryo, which is evident when observing the abundant pinocytic vesicles of the syncytiotrophoblast..
The syncytial cell layer lines the floating villi of the placenta. These villi come into contact with maternal blood when the utero-placental circulation is established, thus regulating the transport of oxygen and nutrients..
Placental apoptosis
Apoptosis or programmed cell death turns out to be an important component in embryonic development, thus the elimination of selected cells occurs, to prevent the indiscriminate loss of cells. Syncytial fusion of cytotrophoblast cells is the initial phase of the apoptotic cascade.
In the initial stage of apoptosis, cytotrophoblast cells proliferate and fuse to form the syncytial layer or syncytiotrophoblast..
In the apoptosis execution phase, the cytoplasmic and nucleic material of the cytotrophoblast has passed into the syncytial layer, so the cells of this last layer are equipped with the necessary material for the apoptotic cascade to start..
The apoptotic process presents a temporary pause due to the action of antiapoptotic enzymes, however, the enzyme caspase 3 reactivates this process, as it in turn activates components that degrade proteins and nucleic acids in cells. Other enzymes responsible for degrading cellular microfilaments are activated.
After the degradation of the cellular components, the waste is packaged in the apical membranes of the syncytiotrophoblast, originating the syncytial or apoptotic nodes, which will be finally released into the mother's bloodstream..
Apoptosis and preeclampsia
Preeclampsia is a pathology presented during pregnancy. Some research has shown that this pathology is caused by an alteration in the differentiation of the trophoblast due to an excess of apoptotic processes at this level.
The release of apoptotic wastes into the maternal bloodstream does not provoke inflammatory responses in the mother because these wastes are protected by a membrane that prevents them from coming into contact with maternal structures. The waste coating process takes a few weeks.
In preeclampsia, there is an excess of proliferation and fusion of cytotrophoblast cells, which causes an increase in cellular degradation in the syncytiotrophoblast. This increase causes an accumulation of cellular debris, and a delay in the formation of their protective membrane..
This causes partially degraded debris and microfragments, including syncytiotrophoblast enzymes to enter the mother's bloodstream, causing tissue damage. In addition to preeclampsia, hypoxic states in the placenta have been associated with an increase in cellular apoptosis.
Evidence for the relationship between apoptosis and preeclampsia
Significant cytoplasmic concentrations of microfragments of the syncytiotrophoblast have been found in patients with preeclampsia. These microfragments can alter macrophage behavior, causing both increased neutrophil activation and decreased endothelial relaxation..
These alterations in maternal blood cells explain the systemic damage and the manifestation of pre-eclampsia, which causes epithelial damage and an inflammatory response. In addition to causing damage to the placenta due to an increase in fibrinoid deposits on the villi.
References
- Flores, A. M., Montoya, J. B., Aguilar, A. O., & Ortega, F. V. (2006). Development and validation of an in vitro culture model for the study of the differentiation of human trophoblast. Gynecology and obstetrics of Mexico, 74 (12), 657-665.
- Hernández-Valencial, M., Valencia-Ortega, J., Ríos-Castillo, B., Cruz-Cruz, P. D. R., & Vélez-Sánchez, D. (2014). Elements of implantation and placentation: clinical and melecular aspects. Mexican Journal of Reproductive Medicine, 6 (2), 102-116.
- Reece, E. A., & Hobbins, J. C. (2010). Clinical Obstetrics / Clinical Obstetrics. Panamerican Medical Ed..
- Rodríguez, M., Couve, C., Egaña, G., & Chamy, V. (2011). Placental apoptosis: molecular mechanisms in the genesis of preeclampsia. Chilean Journal of Obstetrics and Gynecology, 76 (6), 431-438.
- Ross, M. H., & Pawlina, W. (2007). Histology. Panamerican Medical Ed..
- Roura, L. C. (2007). Obstetrics and Maternal-Fetal Medicine. Panamerican Medical Ed..



Yet No Comments