
Obstructive Bronchial Syndrome Symptoms and Treatments
The Obstructive bronchial syndrome It is a set of signs and symptoms produced by the decrease in the caliber of the airways. The main triggers for this syndrome are respiratory infections and bronchial hypersensitivity. The latter is a very common immune disorder in preschool and school children.
The name of this syndrome has changed a lot over time. The medical community does not quite agree which terminology is more appropriate for the simple fact of having a multifactorial pathophysiology and very varied symptoms. It even receives different names according to the age group it affects..

Statistically speaking, obstructive bronchial syndrome is one of the main causes of emergency consultation and hospitalization in pediatrics. This condition has an important seasonal behavior, increasing its incidence in the cold and rainy months, improving in summer or by increasing environmental temperatures..
Article index
- 1 Symptoms
- 1.1 Wheezing
- 1.2 Prolonged expiration
- 1.3 Dyspnea
- 1.4 Cyanosis
- 1.5 Neurological disorders
- 2 Pathophysiology
- 2.1 Contraction of bronchial smooth muscle
- 2.2 Edema and inflammation
- 2.3 Retention of secretions
- 2.4 Loss of elastic support
- 2.5 Remodeling the wall
- 3 Treatments
- 3.1 Bronchodilators
- 3.2 Steroids
- 3.3 Oxygen
- 3.4 Antibiotics
- 3.5 Other treatments
- 4 References
Symptoms
Obviously, the respiratory manifestations are the most important in this syndrome, but not the only ones. The most relevant signs and symptoms of this condition are described below:
Wheezing
It is one of the cardinal symptoms of bronchial obstruction. It is a high-pitched, whistling sound, predominantly expiratory, that is generated in the smallest and deepest airways of the lung. It is related to bronchial narrowing and shows the difficulty that air has to leave the lungs.
Bronchial obstruction due to the presence of excessive mucus or bronchoconstriction exerts a valve effect. It can allow the entry of air with little difficulty but not the exit of the same.
Hence, the beep occurs almost always on expiration, although in severe cases it can also be inspiratory prior to auscultatory silence..
Prolonged expiration
It is an important clinical sign, but it can be difficult to evaluate if you do not have the necessary experience. As explained in the previous section, in patients with bronchial obstruction the air enters the airways easily but it is difficult to get out, so that expiration becomes slow, painful and prolonged..
The physical examination may reveal expiratory effort, choppy ventilation, cough, and rib pulling. On auscultation of the chest, aggregates will be heard at the end of expiration, such as wheezing and universal rhonchi..
Dyspnoea
The third cardinal symptom of obstructive bronchial syndrome is respiratory distress; always accompanies this pathology to a lesser or greater extent.
The decrease in oxygen concentration in the blood triggers a series of signals that are sent to the upper respiratory centers and ventilatory compensation systems are activated..
Clinically there is nasal flutter, intercostal pulling, xiphoid retraction and, occasionally, cyanosis.
On auscultation we can hear universal wheezing and scattered rhonchi. In severe cases, auscultatory silence occurs due to the total closure of the airways that does not allow the entry or exit of air.
Cyanosis
Violet or bluish discoloration of the skin due to hypoxemia. As the amount of deoxygenated hemoglobin increases, the blood loses its usual reddish color and turns blue due to the optical effects of light on tissues without oxygen..
Neurological disorders
Hypoxia at the brain level can cause behavioral disturbances. From psychomotor agitation to lethargy, they are signs of severe illness and urgent measures must be taken to improve the clinical picture. The ultimate consequences of sustained hypoxia can be seizures and coma..
Pathophysiology
Although there are several causes of bronchial obstructive syndrome, the two most important are infectious and immunological. Most infections are viral in origin. Immunological causes depend on the age group and can be initially bronchiolitis and end in asthma.
The pathophysiological mechanisms can vary somewhat depending on the cause, but are summarized in five main pathways:
Contraction of bronchial smooth muscle
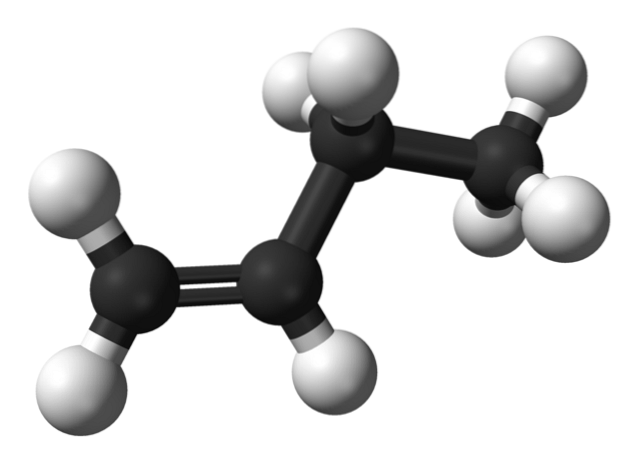
The presence of a germ or an allergen in the respiratory tract produces the release of various local pro-inflammatory substances. Histamine, leukotriene D4, prostaglandins and thromboxanes are some of these substances whose receptors are found in the bronchial smooth muscles.
These receptors are coupled to phospholipase C, which releases IP3 and PKC. In turn, it activates intracellular calcium, which is closely linked to the sustained contraction of the bronchial muscles and, therefore, in the generation of symptoms. The action of IP3 and PKC is often the subject of investigation for new treatments.
Edema and swelling
The same substances that stimulate phospholipase C and cause bronchoconstriction also cause inflammation. Swollen airways do not allow the normal passage of air and contribute to the appearance of the usual symptoms of bronchial obstruction.
Retention of secretions
Mucus production is a normal phenomenon of the airways. It is used for defensive tasks and expulsion of foreign bodies.
When the goblet cells of the lung are overstimulated and produce excessive mucus, this cannot be adequately eliminated due to the bronchial obstruction itself and accumulates in the airway.
As mentioned before, this mucus causes a valve effect in the bronchioles, allowing air to enter but not to exit, generating air retention and clinical deterioration of the patient..
Loss of elastic support
Chronic local inflammation, whatever its origin, can cause permanent effects in the airway. One of these effects is the loss of elasticity in the muscles of the bronchial wall due to elastin dysfunction, among other causes. This leads to a slower recovery and possible chronicity of the respiratory disease..
Wall remodel
Another cause of chronic obstructive disease is remodeling of the bronchial wall. The constant contraction of the bronchial smooth muscle produces its hypertrophy, like any muscle subjected to an exercise regimen, and this increase in size changes the normal structure of the wall and permanently decreases the airway lumen..
Treatments
Knowing the pathophysiological phenomena of obstructive bronchial syndrome, treatments can be established. There are basic therapeutic lines, including the following treatments:
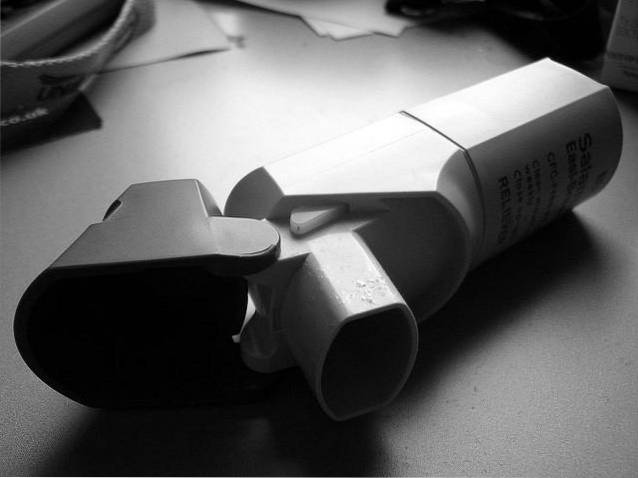
Bronchodilators
They can be short-acting or long-acting, depending on their acute or chronic use. They are inhaled medications and the most popular are beta-2 adrenergic agonists, anticholinergics and theophylline.
Steroids
They have an anti-inflammatory and immunoregulatory function. They can be administered by inhalation or intravenous route. Its use should be controlled due to its adverse effects.
Oxygen
The supply of oxygen at different concentrations is necessary when there is clinical and laboratory evidence compatible with hypoxemia. In severe cases it can be administered directly to the lungs through an endotracheal tube..
Antibiotics
If the origin of the disease is suspected to be infectious bacteria, antibiotics should be started immediately, either orally or intravenously. Some authors recommend its prophylactic use in severe cases of unknown origin..
Other treatments
Other medications such as antihistamines, mucolytics, antileukotrienes and immunomodulators can be used to control the symptoms associated with obstructive bronchial syndrome. All have shown a positive effect and good tolerance.
References
- Novozhenov, VG et al. (1995). The pathogenesis of a broncho-obstructive syndrome in patients with chronic bronchitis. Klinicheskaia Meditsina, 73 (3): 40-44.
- Khan Academy (2018). Broncho-obstructive syndrome in children. Recovered from: doctorsask.com
- Bello, Osvaldo et al. (2001). Infant bronchial obstructive syndrome. Outpatient management. Archives of Pediatrics of uruguay, volume 72, number 1.
- Puebla Molina, S et al. (2008). The Tal scale as a diagnostic test and clinical diagnosis as the gold standard in infantile bronchial obstructive syndrome. Pediatrics Primary Care, volume X, number 37, 45-53.
- Picó Bergantiños, María Victoria and collaborators (2001). The role of bronchial smooth muscle and nerves in the pathophysiology of bronchial asthma. Cuban Journal of Comprehensive General Medicine, 17 (1): 81-90.
- Wikipedia (last edition 2018). Bronchodilator. Recovered from: en.wikipedia.org


Yet No Comments