
Cloistered syndrome symptoms, causes, treatments

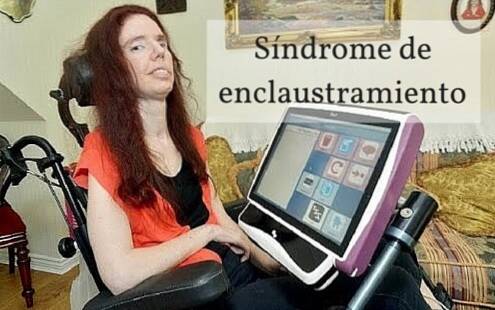
The locked-in syndrome is a rare neurological disorder characterized by a generalized and complete paralysis of the voluntary muscles of the body, except for those that control eye movements (National Institute of Neurological Disorders and Stroke, 2007).
This pathology leaves individuals totally paralyzed and worlds, so on many occasions it is frequent that the terms and "captivity syndrome" or "confinement syndrome" are used to refer to it..
The cloistered syndrome is a secondary condition to a significant lesion at the level of the brainstem with an involvement of the corticospinal and corticobulbar pathways (Collado-Vázquez & Carrillo, 2012).
In addition, these damages to the brain can occur as a result of suffering from various conditions: head trauma, various pathologies related to the circulatory system, diseases that destroy the myelin of nerve cells or by overdose of some drugs (National Institute of Neurological Disorders and Stroke, 2007).
People with locked-in syndrome are fully conscious, that is, they can think and reason, but they will not be able to speak or perform movements. However, they may be able to communicate through eye movement (National Institute of Neurological Disorders and Stroke, 2007).
Despite this, the majority of cases in which there is a serious alteration or damage to the brainstem there is no specific surgical or pharmacological repair and, therefore, neurological deficits can be chronic (Collado-Vázquez and Carrillo , 2012).
Mortality in the acute phase occurs in approximately 60% of cases and there is rarely a recovery of motor function, although patients with a non-vascular etiology have a better prognosis (Riquelme Sepúlveda et al., 2011).
Therefore, the therapeutic intervention in this type of pathologies focuses on the basic care that maintains the vital functions of the patient and the treatment of possible health complications (Collado-Vázquez and Carrillo, 2012).
Article index
- 1 What is the locked-in syndrome or Locked-in syndrome?
- 2 Statistics
- 3 Signs and symptoms
- 4 Types of Captivity Syndrome or Locked-in Syndrome
- 5 Causes
- 5.1 Etiological factors of brain damage
- 6 Diagnosis
- 7 Treatment
- 8 References
What is locked-in syndrome or Locked-in syndrome?
The cloistered syndrome presents a clinical picture characterized by tetraplegia (total paralysis of the four limbs) and anarthria (inability to articulate sounds), with preservation of the state of consciousness, respiratory function, vision, coordination of eye movements and hearing (Mellado et al., 2004).
At an observational level, a patient with locked-in syndrome is represented awake, immobile, without the ability to communicate through language and with preserved eye movements (Mellado et al., 2004).
This pathology was first described in the novel The Count of Monte Cristo by Alejandro Dumas, about the year 1845. It was not until 1875 when the cloistered syndrome appears described in the medical literature by Darolles with the first clinical case (Collado-Vázquez and Carrillo, 2012).
The main clinical characteristics of this affectation were already described in Dumas's novel:
The elderly Noirtier de Villefor has been totally paralyzed for six years: “motionless as a corpse”, perfectly lucid and communicating through a code of eye movements.
Due to the devastating consequences of the locked-in syndrome it has been described in presenting in many works both cinematographic and television.
Statistics
The syndrome of confinement or captivity is a common disease. Although its prevalence is not exactly known, in 2009, 33 cases had been documented and published, so some investigations estimate its prevalence in <1 caso por cada 1.000.000 personas (Orphanet, 2012).
Due to the fact that there are many cases of captivity syndrome that are not detected or that are misdiagnosed, it is difficult to determine the real number of people who suffer or have suffered this type of pathology in the general population National Organization for Rare Diseases, 2010).
Regarding sex, it affects women and men equally and, in addition, it can affect a person of any age, however, it is more common in older adults due to suffering from cerebral ischemia or hemorrhage (National Organization for Rare Diseases, 2010 ).
The estimated average age for the occurrence of locked-in syndrome due to vascular causes is 56 years, while the average age for its condition due to non-vascular factors is estimated to be around 40 years (Collado-Vázquez and Carrillo, 2012).
Signs and symptoms
The American Congress of Rehabilitative Medicine (1995) defined Locked-in Syndrome (LIS) as a pathology characterized by the preservation of consciousness and cognitive functions, with one for the performance of movements and communication through language (Brain Foundation , 2016).
Generally, 5 criteria are considered that can define the presence of locked-in syndrome in most cases (National Rehabilitation Information Center, 2013):
- Quadriplegia or tetraparesis
- Maintenance of superior cortical functions.
- Severe aphonia or hypophonia.
- Ability to open eyes and perform vertical movements.
- Using eye movements and blinking as a means of communication.
However, depending on the location and severity of the injury, the presentation of several other signs and symptoms may be noted (Luján-Ramos et al., 2011):
- Anticipatory signs: headache, vertigo, paraesthesia, hemiparesis, diplopia.
- Preservation of wakefulness and consciousness.
- Motor disorders: tetraplegia, anarthria, facial diaplegia, decerebrate rigidity (abnormal posture with arms and legs extended and head and neck bowed back).
- Eye signs: paralysis of bilateral conjugation of horizontal eye movements, maintenance of blinking and vertical eye movements.
- Remaining motor activity: distal finger movements, facial and tongue movement, head flexion.
- Involuntary episodes: grunting, crying, oral automatisms, among others.
In addition, in the presentation of the captivity syndrome, two phases or moments can be distinguished (National Organization for Rare Diseases, 2010):
- Initial or acute phase: the first phase is characterized by anarthraia, respiratory involvement, total muscular paralysis and episodes of loss of consciousness.
- Post-acute or chronic phase: consciousness, respiratory function, and vertical eye movements are fully restored.
Types of Captivity Syndrome or Locked-in Syndrome
The captivity syndrome has been classified according to different criteria: severity, evolution and etiology. Despite this, generally the etiology and severity are the factors that offer us more information about the future prognosis of the patient (Sandoval and Mellado, 2000).
Depending on the severity, some authors such as Bauer have described three categories for locked-in syndrome (Brain Foundation, 2016):
- Classic locked-in syndrome (Classic LIS): preservation of consciousness, total muscle paralysis except for vertical eye movements and blinking.
- Total locked-in syndrome (Complete or total LIS): preservation of consciousness, in the absence of linguistic communication and eye movements. Complete muscle and motor paralysis.
- Incomplete locked-in syndrome (Incomplete LIS): preservation of consciousness, recovery of some voluntary movements and maintenance of eye movements.
In addition, in any of these types, a patient with captivity syndrome can present two conditions:
- Transient locked-in syndrome: characterized by neurological improvement that can become complete in the absence of permanent brain damage (Orphanet, 2012).
- Transient locked-in syndrome: there is no substantial neurological improvement and is usually associated with the presence of permanent and irreparable brain damage (Orphanet, 2012).
Causes
Classically, Locked-in syndrome occurs as a consequence of the existence of lesions in the brainstem, occlusion or lesion of the vertebral or basilar artery or compression of the cerebral peduncles (Orphanet, 2012).
Many of the cases are caused specifically by damage to the pons (brainstem area). The pons has important neural pathways that connect the rest of the brain areas with the spinal cord (National Organization for Rare Diseases, 2010).
Lesions usually occur at the level of the corticobulbar, corticospinal, and corticopontine pathways, resulting in muscle paralysis and anarthria. Normally, the ascending somatosensory and neuronal pathways remain intact, so the level of consciousness, the wake / sleep cycles and the excitability of external stimulation are maintained (Samaniego, 2009; Riquelme Sepúlveda et al., 2011).
Etiological factors of brain damage
In general, etiological factors are usually divided into two categories: vascular and non-vascular events..
In both adults and children, the main cause is dancing thrombosis, it occurs in 60% of cases (Sepúlveda et al., 2011).
On the other hand, among the non-vascular causes, the most frequent are traumatic accidents, due to a contusion in areas of the brain stem (Sepúlveda et al., 2011).
In addition, it is also possible that the development of cloistered syndrome secondary to tumors, encephalitis, multiple sclerosis, Guillian Barré disease, amyotrophic lateral sclerosis or myasthenia gravis, among others (Sepúlveda et al., 2011).
Diagnosis
The diagnosis of this pathology is based both on the observation of clinical indicators and on the use of various diagnostic tests.
Often, eye movements can be observed spontaneously and the willingness to communicate through this can also be identified by family members and caregivers. For these reasons, it is essential that changes in eye movement in response to simple commands be examined (Orphanet, 2012). To perform a differential diagnosis with the vegetative or minimally conscious state.
Additionally, a physical examination will be essential to confirm muscle paralysis and inability to articulate speech.
On the other hand, the use of functional neuroimaging techniques allows detecting the location of brain damage and examining signs of consciousness.
Some of the techniques used in the diagnosis of captivity syndrome or Locked-in syndrome are (National Organization for Rare Diseases, 2010):
- Magnetic Resonance Imaging (MRI): are often used to confirm brain damage in areas related to captivity syndrome.
- Magnetic resonance angiography: are used to identify the possible presence of a blood clot or thrombus in the arteries supplying the brainstem.
- Electroencephalogram (EEG): It is used to measure brain activity, it can reveal the presence of signal processing in the absence of explicit consciousness, wakefulness and sleep cycles, among other aspects.
- Electromyography and nerve conduction studies: are used to rule out the presence of damage to the peripheral nerves and muscles.
Treatment
There is currently no cure for captivity syndrome, nor a protocol or standard course of treatment (National Institute of Neurological Disorders and Stroke, 2007).
The initial treatment in this pathology is aimed at treating the etiological cause of the disorder (National Organization for Rare Diseases, 2010).
In the first phases, it will be necessary to use basic medical care both to protect the life of the patient and to control possible complications. They usually require the use of artificial measures of respiration or feeding through gastrostomy (feeding through a small tube inserted into the stomach (National Organization for Rare Diseases, 2010).
Once the acute phase is over, the therapeutic interventions are oriented towards the autonomous recovery of respiratory function, recovery of swallowing and independent urination, development of motor skills of the head and neck fingers, and finally, the establishment of a communicative code through eye movement (Orphanet, 2012).
Later, the treatment is directed towards the recovery of the voluntary movements. In some cases, the movement of the fingers, the control of swallowing or the production of some sounds is achieved, while in others, the control of any voluntary movement is not achieved National Organization for Rare Diseases, 2010).
References
- Brain Foundation. (2016). Locked-in Syndrome (LIS). Obtained from Disorders. Brain Foundation: brainfoundation.org.au
- Collado-Vázquez, S., & Carrillo, J. (2012). The captivity syndrome in literature, cinema. Rev Neurol, 54(9), 564-570.
- MD. (2011). Locked In Syndrome. Obtained from WebMD: webmd.com
- Mellado, P., Sandoval, P., Tevah, J., Huete, I., & Castillo, L. (2004). Intra-arterial thrombolysis in basilar artery thrombosis. Recovery in two patients with cloistered syndrome. Rev Méd Chil, 357-360.
- NARIC. (2012). What is cloistered syndrome? Obtained from National Rehabilitation Information Center: naric.com
- NIH. (2007). Locked-In Syndrome . Retrieved from National Institute of Neurological Disorders and Stroke: ninds.nih.gov
- NORD. (2010). Locked In Syndrome. Obtained from National Organization for Rare Disorders: rarediseases.org
- Orphanet. (2012). Cloistered syndrome. Obtained from Orphanet: orpha.net
- Riquelme Sepúlveda, V., Errázuriz Puelma, J., & González Hernández, J. (2011). Cloistered syndrome: clinical case and literature review. Rev. Mem., 8, 1-9.
- Sandoval, P., & Mellado, P. (2000). Locked-in syndrome. Obtained from Neurology Notebooks: school.med.puc.cl


Yet No Comments