
Staphylococcus aureus characteristics, morphology, pathogenesis
Staphylococcus aureus it is the most pathogenic species of the genus Staphylococcus, being the main cause of 60% of acute purulent infections in the world, because it is a pyogenic germ par excellence.
This microorganism is widely distributed in nature, it can be found in the environment and as a common microbiota of the skin and mucous membranes of the mouth, intestine and nose in humans and animals..

That is why the isolation of S. aureus it will be clinically important if there is an obvious infectious process, as it is a common skin colonizer.
When S. aureus overcomes natural defense barriers and enters the body, can cause pathologies ranging from localized lesions, systemic infections to distant poisonings.
Some people are classified as asymptomatic carriers of S. aureus when they harbor pathogenic strains in the nostrils and on the hands. The percentage of carriers ranges between 20 - 40%, being responsible for its dissemination.
Article index
- 1 Features
- 2 Taxonomy
- 3 Morphology
- 4 Virulence factors
- 4.1 The capsule
- 4.2 Peptidoglycan
- 4.3 Teichoic acid
- 4.4 Protein A
- 4.5 Enzymes
- 4.6 Toxins
- 5 Pathogenesis and pathology
- 5.1 Localized skin affections
- 5.2 Systemic infections
- 5.3 Clinical manifestations produced by staphylococcal toxins
- 6 Transmission
- 7 Diagnosis
- 8 Treatment
- 9 Prevention
- 10 References
Characteristics
The Staphylococcus genus differs from the Streptococcus genus in that they are catalase positive, in addition to their way of being distributed in space as clusters.
Likewise, to Staphylococcus aureus it is distinguished from the rest of the species by producing an enzyme called coagulase. That is why all members of this genus isolated from clinical samples other than the aureus species are called coagulase negative Staphylococcus..
A relevant feature of S. aureus, the thing iscan survive on the surface of objects, pus, dried sputum, sheets, clothing, handwraps, and fomites in general, for long periods of time.
This means that they are highly resistant to many adverse conditions despite not forming spores. They are capable of withstanding temperatures of up to 60º C for up to one hour. Likewise, they are more resistant than other bacteria to certain common disinfectants..
However, they are destroyed by basic dyes and by moist heat under pressure..
Something that has concerned the medical community is that S. aureus has developed the ability to generate various mechanisms of resistance to antibiotics to circumvent treatments.
Among them we have the production of beta-lactamases (enzymes that degrade beta-lactam antibiotics such as penicillin) and the modification of the binding site of antibiotics.
Likewise, it is capable of receiving plasmids that contain genetic information for resistance to other antibiotics, which are transferred from one bacterium to another by bacteriophages..
Taxonomy
S. aureus belongs to Domain: Bacteria, Kingdom: Eubacteria, Phylum: Firmicutes, Class: Bacilli, Order: Bacillales, Family: Staphylococcaceae, Genus: Staphylococcus, Species: aureus.
Morphology
Staphylococcus are spherical cells 0.5 to 1 μm in diameter called cocci, which are arranged in groups, simulating bunches of grapes..
Before the Gram staining technique, they are stained purple, that is, they are Gram positive.
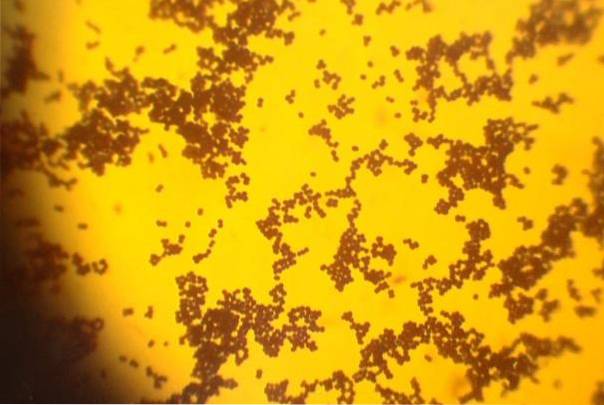
S. aureus it is not mobile, does not form spores, some strains have a polysaccharide capsule.
From a laboratory point of view they are easily cultivable and identifiable. They are facultative anaerobes, they grow well at 37ºC in 24 hours of incubation in simple media..
Its colonies are creamy, generally golden yellow, hence its name aureus, although some strains do not produce pigment and are observed to be white..
On blood agar they can develop pronounced beta-hemolysis.
Virulence factors
S. aureus it has many elements to produce different diseases, but not all virulence factors are found in all strains. This means that some strains of S. aureus are more virulent than others.
Among them we have:
The capsule
It is polysaccharide and protects the microorganism from being phagocytosed by polymorphonuclear leukocytes (PMN). It also makes it easier for you to adhere to host cells and artificial devices such as prosthetics. Increases its ability to form biofilms. There are 11 different capsular types, the most pathogenic being 5 and 8.
Peptidoglycan
It activates the complement and contributes to the inflammatory response. Stimulates endogenous pyrogen production.
Teicoic acid
Participates in the adherence to the mucosa and activates the complement.
Protein A
Interferes with opsonization by binding to the Fc portion of IgG immunoglobulins.
Enzymes
Catalase
Inactivates hydrogen peroxide and toxic free radicals.
Coagulase
Converts fibrinogen to fibrin, to protect against opsonization and phagocytosis.
Leukocidin
Destroys PMNs by forming pores in their membrane.
Hyaluronidase
Hydrolyzes hyaluronic acid from collagen to spread the microorganism in tissues.
Lipases
Hydrolyzes lipids for the spread of bacteria to skin and subcutaneous tissue.
Staphylokinase or fibrinolysin
Fibrinolytic enzyme that dissolves clots.
Endonuclease / DNAse
Hydrolyzes DNA.
Betalactamase
Hydrolyzes penicillin.
Toxins
Hemolysin
Α-Hemolysin destroys PMN, smooth erythrocytes, is dermonecrotic, and neurotoxic. Whereas β-hemolysin is a sphingomyelinase. Other hemolysins act as a surfactant and by activating adenylate cyclase.
Exfoliative toxin
It is proteolytic, it smooths the intracellular junctions of the cells of the stratum granulosa of the epidermis, acting specifically on desmoglein-1. It is responsible for scalded skin syndrome.
Toxin Shock Syndrome (TSST-1)
Superantigen that activates a large number of lymphocytes with exaggerated production of cytokines. This toxin is produced by some strains of aureus that colonize the vagina.
Enterotoxin
They are a group of proteins (A, B, C, D) that cause pseudomembranous colitis, diarrhea and vomiting and are responsible for food poisoning caused by consuming food contaminated with aureus.
Pathogenesis and pathology
The production of infection by S. aureus depends on multiple factors, including: strain involved, inoculum, gateway, and host immune response.
As a gateway you can use wounds, burns, insect bites, lacerations, surgical interventions and previous skin diseases.
Localized skin affections
It is characterized by the appearance of pyogenic lesions such as boils or abscesses, which is an infection of the hair follicle, sebaceous gland or sweat gland.
If these lesions spread and converge, lesions called carbuncles are formed. These lesions can be aggravated and the organism can invade the bloodstream..
On the other hand, if the infection spreads through the subcutaneous tissue, it produces a diffuse inflammation called cellulitis..
All of these are infectious processes caused by S. aureus at the skin level that involves inflammatory mechanisms with the participation of neutrophils, production of lysosomal enzymes that destroy the surrounding tissue.
There is accumulation of dead neutrophils, edematous fluid, dead and live bacteria that make up the pus.
Another skin condition is usually secondary infection of a Streptococcus pustular impetigo or they can produce bullous (bullous) impetigo on their own..
They are generally caused by strains that produce exfoliative toxin and it is usually the localized focus that causes scalded skin syndrome.
Systemic infections
When drainage of the contents of an abscess into a lymphatic or blood vessel occurs, serious deep infections such as osteomyelitis, meningitis, pneumonia, nephritis, endocarditis, septicemia can occur.
In deep locations the microorganism has the ability to produce destructive metastatic abscesses.
Clinical manifestations produced by staphylococcal toxins
Scalded skin syndrome
The exfoliative toxin produced from a local lesion causes distant damage characterized by erythema and intraepidermal scaling. Lesions can begin on the face, armpits, or groin, but can spread to the entire body. It is common in children under 5 years of age and immunosuppressed adults.
Toxic Shock Syndrome
The activation of toxin production has been associated with the use of a tampon during menstruation, although it can also occur under other circumstances, producing high fevers, hypotension, muscle aches, diarrhea, rash, shock with liver and kidney damage..
Food poisoning
It occurs by eating food contaminated with aureus that have excreted their enterotoxins in carbohydrate-rich food. Produces diarrhea and vomiting without fever 5 hours after consuming the food. Recovery is spontaneous.
Transmission
S. aureus is spread from one person to another by manual contact with asymptomatic carriers of pathogenic strains or contaminated objects, or by aerosols emitted by patients with pneumonia caused by this bacterium.
Neonates are colonized through the manipulation of carriers, often within the hospital.
Healthcare workers, diabetics, hemodialysis patients, HIV + seropositive patients, and intravenous drug addicts are more likely to become chronic carriers of this bacteria.
Asymptomatic carriers should not be food handlers or vendors, to avoid food poisoning by this bacterium in the community.
Diagnosis
Staphylococcus are easy to isolate and identify.
The observation of typical colonies on blood agar, growth of yellow colonies on salty mannitol agar, or black colonies on Baird-Parker agar, plus positive catalase and coagulase test, are sufficient for the identification of the aureus species..
In some countries, candidates who wish to opt for food handling jobs are required as a pre-employment test to carry out a pharyngeal swab and culture of the nostrils..
This is essential to rule out the condition of asymptomatic carrier of S. aureus.
Treatment
In mild local affectations, the lesions generally resolve spontaneously after drainage. In more serious or deep affectations, it may require surgical drainage and subsequent treatment with antibiotics..
In the past they were treated well with penicillin. However, today most strains are resistant to this antibiotic due to the production of beta-lactamases..
Therefore, they are treated with beta-lactamase-resistant penicillin (methicillin, oxacillin, or nafcillin) and first-generation cephalosporins (cefazolin, cephalothin)..
In the case of methicillin resistant strains (MRSA) or patients allergic to beta-lactams, other alternatives, such as vancomycin, should be used, as long as it is not a (VISA) OR (VRSA) strain, that is, with intermediate resistance or resistance. constitutive to vancomycin respectively.
Clindamycin and erythromycin can also be used when these are susceptible. They cannot be used in RIC strains (E-test positive), that is, with inducible resistance to clindamycin.
Prevention
Aseptic measures are essential to try to minimize its spread. Carrier status is difficult to remove.
It is recommended that these patients bathe with chlorhexidine soaps, hexachlorophene, use topical antimicrobial creams in the nasal passages such as (mupirocin, neomycin and bacitracin) and oral therapy with rifampicin or ciprofloxacin.
During and after surgeries, chemoprophylaxis is usually used to avoid infections with this microorganism such as methicillin, cephalosporin and vancomycin..
References
- Ryan KJ, Ray C. Sherris. Microbiology Medical, 6th Edition McGraw-Hill, New York, U.S.A; 2010.
- World Health Organization. Antimicrobial resistance. Geneva. 2015. [consulted in June 2015] Available at: who.int/
- Echevarria J. The problem of Staphylococcus aureus methicillin resistant. Rev. Med. Hered. 2010; 21 (1): 1-3.
- Koneman, E, Allen, S, Janda, W, Schreckenberger, P, Winn, W. (2004). Microbiological Diagnosis. (5th ed.). Argentina, Editorial Panamericana S.A.
- Wikipedia contributors. Staphylococcus aureus. Wikipedia, The Free Encyclopedia. September 2, 2018, 06:51 UTC. Available at: en.wikipedia.org/. Accessed September 8, 2018.
- Otto M. Staphylococcus aureus toxins. Current opinion in microbiology. 2014; 0: 32-37.
- Tong SYC, Davis JS, Eichenberger E, Holland TL, Fowler VG. Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. Clinical Microbiology Reviews. 2015; 28 (3): 603-661. doi: 10.1128 / CMR.00134-14.


Yet No Comments