
Streptococcus pyogenes characteristics, morphology, pathogenesis
Streptococcus pyogenes, Also called Group A Beta-hemolytic Streptococcus, it is a species of Gram positive bacteria. It is one of the most virulent species of this genus, being the causative agent of acute pharyngitis, streptococcal pyodermatitis, erysipelas, puerperal fever and septicemia, among other pathologies.
Likewise, these pathologies can generate sequelae, causing autoimmune diseases such as rheumatic fever and acute glomerulonephritis. The most common disease is pharyngitis, which mainly affects children between the ages of 5 and 15 years..
Approximately 15% of individuals with strep throat can become asymptomatic carriers of the bacteria after treatment..
Article index
- 1 Taxonomy
- 2 Features
- 3 Morphology
- 4 Virulence factors
- 5 Pathologies
- 6 Diagnosis
- 7 Treatment
- 8 References
Taxonomy
Reino: Eubacteria.
Phylum: Firmicutis.
Class: Bacilli.
Order: Lactobacillales.
Family: Streptococcaceae.
Genus Streptococcus.
Species: pyogenes.
Characteristics
-Man is the only natural reservoir of the Streptococcus pyogenes. It lives in the throat and on the skin of healthy carriers and is transmitted from person to person through the respiratory route by expelling droplets of saliva when talking, coughing or sneezing.
-They are facultative anaerobes. They are not mobile, they do not form spores. They grow well under the following conditions: blood-enriched media, pH 7.4, temperature 37 ° C, 10% CO environmenttwo.
-The Streptococcus pyogenes are capable of fermenting some carbohydrates producing lactic acid as a final product.
-They are catalase negative, which differentiates it from the genus Staphylococcus.
-They are less resistant than Staphylococcus to survive outside the body. They are destroyed at 60ºC for 30 minutes.
Morphology
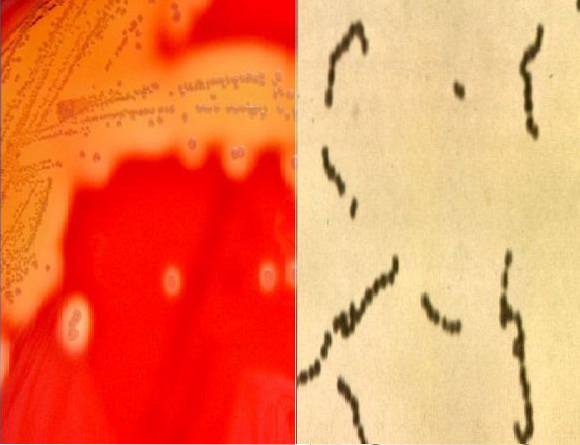
Streptococcus pyogenes They are Gram positive cocci that are arranged in short or semi-long chains made up of approximately 4 to 10 bacteria.
They have a capsule of hyaluronic acid and in their cell wall they contain a carbohydrate C that gives them group specificity..
The carbohydrate is made up of L-rhamnose and N-acetyl-D-glucosamine and is covalently bound to peptidoglycan.
Thanks to this carbohydrate, Streptococcus can be classified by groups (A, B, C, D). This classification was made by Lancefield, and in this sense S. pyogenes belongs to group A.
On blood agar the colonies are small creamy white with an area of beta-hemolysis around the colony (light halo produced by the lysis of red blood cells).
Virulence factors
Hyaluronic Acid Capsule
It confers antiphagocytic properties by preventing the opsonization of the microorganism.
Protein M
It is a surface antigen (fibrillar proteins) associated with the outermost part of the wall and protrudes from the cell surface. It confers antiphagocytic activity and prevents intracellular death by polymorphonuclear cells.
This protein is immunogenic, therefore it stimulates the immune system to produce anti-M protein antibodies. There are more than 80 different subtypes..
OF opacity factor
Surface antigen associated with M protein. It is an Alpha-lipoproteinase capable of opacifying media containing horse serum..
T and R antigens
They are present in some strains, but it is unclear if they are involved in virulence. Everything seems to indicate that no.
Hemolysins or Streptolysin O and S
Streptolysin O is an antigenic cytotoxin that forms transmenbranous pores on leukocytes, tissue cells, and platelets to lyse them. The immune system reacts by forming antistreptolysis antibodies O.
This cytotoxin is oxygen labile and therefore smooths red blood cells on the inside of the blood agar culture. While streptolysin S is stable against oxygen, it is not antigenic and is capable of lysing erythrocytes above and below blood agar..
It also forms pores on a wide variety of cells. It is especially leukotoxic, killing the leukocytes that engulf these streptococci..
Lipoteichoic acid
Forms a complex with the M protein and participates in adhesion to epithelial cells.
Streptokinase
It is an enzyme that causes the transformation of plasminogen into plasmin that digests fibrin.
Streptodornase
There are 4 types: A, B, C and D. They are also known as deoxyribonucleases or nucleases. It has the property of depolymerizing DNA in exudates and necrotic tissues.
Hyaluronidase
Hydrolyzes hyaluronic acid, which is the main constituent of connective tissue, thus giving it the ability to spread in tissues..
Erythrogenic or pyrogenic toxin
It is a superantigen that causes fever, rash (scarlet fever), proliferation of T lymphocytes, suppression of B lymphocytes, and increased sensitivity to endotoxins..
There are four types; A, B, C, and D. The production of types A and C depend on the presence of an early gene carried by a bacteriophage. B is produced by a chromosomal gene. D is not fully characterized.
Protein F and LTA
They are surface proteins that bind to fibronectin and interfere with opsonization.
Peptidase C5a
It is an enzyme that degrades the C5a component of complement (chemotactic substance), inhibiting the attraction of phagocytes to complement deposit sites.
Pathologies
Acute pharyngitis
The incubation period is 2 to 4 days. The disease begins abruptly, presenting fever, chills, severe sore throat, headache, general malaise.
The posterior wall of the pharynx is swollen and edematous, commonly reddened. It can also involve the uvula, soft palate and tonsils, appearing a grayish-white or yellowish-white exudate on these structures.
It is common for anterior cervical lymph nodes to become swollen, enlarged, and tender..
The disease is usually self-limited within a week, however it may spread and cause peritonsillar or retropharyngeal abscesses, otitis media, suppurative cervical adenitis, mastoiditis, and acute sinusitis..
Rarely can cause spread (bacteremia, pneumonia, meningitis, or metastatic infections to distant organs).
Some strains that produce pyrogenic toxins A, B, and C can produce a scarlitiniform rash..
Impetigo
Also called streptococcal pyodermatitis, it is characterized by small superficial vesicles surrounded by an area of erythema. The vesicles develop into a pustule within days, then rupture and form a yellowish crust.
These lesions usually appear in children between the ages of 2 and 5, especially on the face and lower extremities. If several lesions come together they can form deep ulcers.
These lesions are very contagious so it is easily spread by direct contact..
Erysipelas
They are slightly deeper lesions that occur at the level of the dermis (cutaneous and subcutaneous tissue).
It is manifested by a widespread area of diffuse erythema, edema, and induration of the affected skin (cellulitis that can present with lymphangitis and lymphadenitis). This injury progresses rapidly.
Systemic symptoms such as malaise, fever, chills may occur when bacteria invade the bloodstream. These lesions usually appear on the face and lower extremities. There may be a recurrence in the same place.
Puerperal infection
Although puerperal infection caused by Streptococcus agalactiae, Streptococcus pyogenes is able to penetrate the uterus after delivery and cause fatal septicemia.
The source is usually the hands or oropharyngeal secretions of the doctor or nurse, which behave as asymptomatic carriers. If health personnel do not comply with aseptic measures, they may be spreading the bacteria.
Scarlet fever
It occurs after streptococcal pharyngitis caused by strains that produce erythrogenic toxin in any of its types A, B and C.
It is characterized by starting with the appearance of a rash that reddens the oral mucosa, cheeks and temples, with a pale area around the mouth and nose (characteristic perioral pallor).
At the level of the hard and soft palate there are pinpoint hemorrhages and a yellowish whitish exudate and prominent red papillae (strawberry tongue) are observed on the tongue.
Subsequently, a fine rash appears that spreads to the chest and extremities. The skin is rough to the touch, similar to sandpaper.
Toxic shock-like syndrome (SSST)
It can affect healthy carriers or contacts when the Streptococcus pyogenes enter through a wound or laceration, affecting subcutaneous tissue, lymphagitis and lymphoadenitis, and subsequently reach the bloodstream.
Systemic disease begins with vague myalgia, chills, and severe pain at the infected site. Nausea, vomiting, diarrhea and hypotension are also manifested, up to Shock and multi-organ failure.
It is frequent that it generates a necrotizing fasciitis and myonecrosis.
Rheumatic fever
It is produced by rheumatogenic strains. It can appear 1-5 weeks after strep throat and without anti-inflammatory treatment it can last 2 or 3 months.
It is a non-suppurative inflammatory disease characterized by fever, carditis, subcutaneous nodules, chorea and migratory polyarthritis.
Clinically, it presents cardiac, myocardial and epicardial enlargement, which can lead to heart failure.
Acute post streptococcal glomerulonephritis
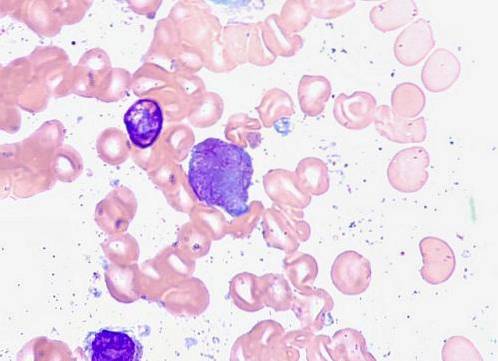
It is a disease mediated by antigen-antibody immune complexes that form in the circulation and are deposited in kidney tissue. Also antigens and antibodies can arrive separately and bind on the tissue.
This triggers the recruitment of immune cells, the production of chemical mediators and cytokines, and the local activation of complement, leading to a localized inflammatory response in the glomeruli..
This sequela is feasible if the strain that caused the previous streptococcal disease is a nephritogenic strain, that is, it contains nephrotoxic antigens..
These are: plasmin receptors associated with nephritis, identified as glyceraldehyde 3-phosphate dehydrogenase and streptococcal pyrogenic exotoxin (erythrotoxin) B and its zymogen precursor.
The disease can appear 1 to 4 weeks after strep throat or 3 to 4 weeks after a skin infection.
Clinically, it is characterized by edema, hypertension, proteinuria, and reduction in serum complement concentrations. Histologically there are diffuse proliferative lesions of the glomeruli.
The course is benign and self-healing in weeks or months, but if it becomes chronic it leads to kidney failure and death..
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal pyogenes infections
Also known as PANDAS Syndrome, it occurs after a severe strep infection, such as pharyngitis or scarlet fever. It is common in children from 3 years to adolescents.
It manifests with obsessive-compulsive disorder, accentuation of symptoms related to post-streptococcal infections, with abnormal neurological examination that includes hyperactivity, attention deficit, fast and arrhythmic involuntary movements, anorexia nervosa and vocalizations with variable complexity.
Diagnosis
For the diagnosis of pharyngitis, impetigo, erysipelas, bacteremia, abscesses, the culture of the corresponding sample on blood agar is useful for the isolation of the microorganism and subsequent identification through tests such as catalase, Gram and sensitivity to bacitracin taxa..
When rheumatic fever or post-streptococcal glomerulonephritis is suspected, the measurement of antistreptolysin O antibodies (ASTO) is useful. In these autoimmune diseases ASTO titers are high (above 250 Todd units).
Treatment
Streptococcus pyogenes is highly susceptible to penicillin G, also other beta-lactams and macrolides.
In patients allergic to penicillin or when mixed infections with S. aureus macrolides (erythromycin or azithromycin) are used.
Appropriate treatment for 10 days after pharyngeal infection can prevent rheumatic fever but not glomerulonephritis.
References
- Wikipedia contributors. Streptococcus pyogenes. Wikipedia, The Free Encyclopedia. August 11, 2018, 18:39 UTC. Available at: https://en.wikipedia.org/. Accessed September 20, 2018.
- Ryan KJ, Ray C. Sherris. MicrobiologyMedical, 6th Edition McGraw-Hill, New York, U.S.A; 2010.
- Koneman, E, Allen, S, Janda, W, Schreckenberger, P, Winn, W. (2004). Microbiological Diagnosis. (5th ed.). Argentina, Editorial Panamericana S.A.
- Chávez O, Crespo K, De Acha R, Flores A. Pediatric Neuropsychiatric Disorder Associated with Streptococcal Infections. Rev Cient Cienc Méd 2010; 13 (2): 86-89.
- Ferretti JJ, Stevens DL, Fischetti VA, editors. Streptococcus pyogenes: Basic Biology to Clinical Manifestations [Internet]. Oklahoma City (OK): University of Oklahoma Health Sciences Center; 2016-. Preface.


Yet No Comments