
Whipple triad history, what it consists of, usefulness

The Whipple's triad it is the association of three clinical characteristics that are considered key to define whether one is in the presence of a patient with hypoglycemia. It was proposed by Dr. Allen Whipple in 1930 and is currently in force..
Hypoglycemia is a disorder that involves multiple factors and that manifests itself with a significant decrease in plasma glycemia, being capable of generating signs and symptoms that warn about its appearance.
It is difficult to establish from what value is considered hypoglycemia, as this can vary from one individual to another for multiple reasons. However, a cut-off point of ≤55 mg / dl is accepted in non-diabetic patients and < a 70 mg/dl para diabéticos.
It should be noted that hypoglycemia can have many causes. It is very common in diabetic patients with a lack of control in the treatment or in non-diabetic patients, with or without an underlying disease (endogenous hypoglycemia).
Given the serious consequences that this can cause in the patient, it is necessary that it be diagnosed as quickly as possible to be able to treat it in time. To determine if a patient is hypoglycemic, the entire triad must be met.
Article index
- 1 History
- 2 What is the Whipple triad?
- 3 Utility of Whipple's triad
- 3.1 Symptoms of hypoglycemia
- 3.2 Determination of blood glucose
- 3.3 Treatment of hypoglycemia
- 4 Causes of hypoglycemia
- 4.1 Hypoglycemia in diabetic patients
- 4.2 Endogenous hypoglycemia
- 5 References
Story
Whipple's triad was named after the surgeon Allen Whipple, who was a specialist in pancreatic surgeries..
In 1930 it was discovered that the main cause of hypoglycemia not associated with diabetes (endogenous hypoglycemia) was due to the presence of an insulin-producing tumor in the pancreas (insulinoma), and that removal of the tumor cured the patient.
He proposed the criteria that should be taken into consideration before proceeding to pancreatic surgery in search of an insulinoma, this being the most frequent cause of endogenous hypoglycemia.
Although it was later determined that there were patients with hypoglycemia who were cured without the need for pancreatic surgery, because hypoglycemia had a cause other than the presence of insulinoma.
Today the triad is useful to suspect hypoglycemia, regardless of the cause that produces it..
What is the Whipple triad?
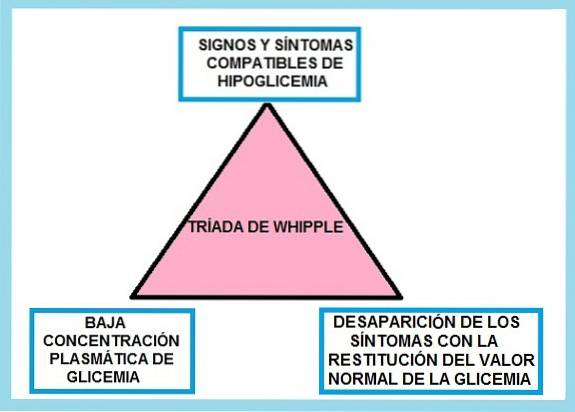
Whipple's triad consists of the fulfillment of 3 well-defined clinical conditions, these are:
1) The patient has characteristic symptoms of hypoglycemia, either autonomic or neuroglycopenic.
2) The hypoglycemic status of the patient (low glycemia) is confirmed through a blood glucose analysis, with venous sampling.
3) The disappearance of symptoms is observed when the glycemic values return to the normal range.
The most difficult thing is to establish what blood glucose value is considered hypoglycemia, since there are patients who may have low blood glucose values, being a normal condition in them. Examples: children and young women. In these cases there are no symptoms.
Other factors also influence, such as a prolonged fast, age, pregnancy, diabetes or other conditions or pathologies, among others..
In this sense, it is thought that for a non-diabetic patient, glycemic values below 55 mg / dl are suspicious and should be studied. While values above 70 mg / dl rule out the diagnosis of endogenous hypoglycemia, whether or not there are associated symptoms.
In non-diabetic patients with prolonged fasting it can be considered from 45 mg / dl downwards, and in the case of diabetic patients a low glycemia with values below 70 mg / dl is considered.
Utility of Whipple's triad
Determining whether a patient is experiencing hypoglycemia is extremely important, since glucose is essential for the proper functioning of the brain, muscles, and the heart system, among others. Therefore, a decrease in glucose can have serious consequences if it is not treated in time..
In this sense, the American Society for Endocrinology continues to recommend the use of Whipple's triad as a basis for the diagnosis and treatment of hypoglycemia..
Symptoms of hypoglycemia
Whipple's triad indicates that there must be symptoms related to hypoglycemia, therefore, it is important to know that there are two types of symptoms: autonomic and neuroglycopenic.
The autonomous ones are the first to appear. Generally, the body issues its first alerts when blood glucose is below 50 mg / dl. Under this circumstance, the production of catecholamines and acetylcholine is triggered, causing symptoms such as: anxiety, tremors, tachycardia, nervousness, paleness, dry mouth, among others..
If blood glucose continues to drop, neuroglycopenic symptoms will occur. These indicate that the neurons' glucose stores were depleted. In this case, the glycemia is below 45 mg / dl.
The symptoms that are observed are: headaches, irritability, confusion, difficulty speaking, confusion, paraesthesia, ataxia, drowsiness, weakness, seizures, coma and even if it is not treated, it can cause death..
Determination of blood glucose
To comply with Whipple's triad, it is important that the patient's blood value is determined..
It is important to emphasize that blood glucose determination with venous sampling is preferred. Arterial blood is not recommended, since it has been determined that arterial blood glucose has higher values than venous blood, which can mask or confuse the picture..
Treatment of hypoglycemia
What confirms the diagnosis of hypoglycemia, according to Whipple's triad, is the disappearance of symptoms with the restoration of normal blood glucose concentration..
Treatment will depend on the severity of the condition. If the hypoglycemia is mild or moderate, the oral route of administration will be the most convenient.
The patient is given liquid or solid foods, which have an approximate value of 15-20 grams of rapidly absorbed glucose, such as: cookies or juices, among others. The procedure can be repeated every 20 minutes, until symptoms resolve.
If the above does not improve, the condition may require the placement of 1 mg of glucagon intramuscularly. Glucose level should be restored in 5-10 minutes.
In unconscious or uncooperative patients, glucagon can be applied directly and, upon seeing improvement, administer 20 grams of glucose initially and then 40 grams of a complex carbohydrate. If there is no improvement, 100 mg of IV hydrocortisone and 1 mg of epinephrine SC can be administered..
The parenteral route with glucose solution will be the route of choice in more severe cases (patients who require hospitalization and who do not respond to the previous therapy)..
The recommended dose is a 50% glucose solution (25 g of glucose per 50 ml) and after observing improvement, continue with a 10% glucose solution.
Capillary blood glucose values should be monitored every 30 minutes to 1 hour and then spaced every 1 to 4 hours. Finally, it is important not only to establish an adequate treatment, but also to determine the cause.
Causes of hypoglycemia
Not all cases of hypoglycemia are the same, those caused by hypoglycemic drugs (sulfonylureas and meglitinides) tend to recur.
For this reason, the patient should not be discharged immediately after the symptoms reestablish, while those that occur due to the administration of insulin do not meet this pattern..
On the other hand, certain conditions can be a predisposing factor to suffer a hypoglycemia, for example, in pregnancy it is common to have low blood sugar, but these can be easily solved with a balanced diet and avoiding prolonged fasting.
Likewise, low blood glucose values are found in the newborn, especially at birth (25-30 mg / dl). This value increases after 3-4 hours. After this time, it should be monitored that it remains above 45 mg / dl.
Hypoglycemia in diabetic patients
Hypoglycemia is one of the most common problems in the management of patients with diabetes, both type 1 (insulin dependent) and type 2 diabetes (non-insulin dependent).
Endogenous hypoglycemia
It is important to classify possible patients with endogenous hypoglycemia into two large groups.
The first group is represented by those patients with an underlying pathology, other than diabetes mellitus. This condition is called hypoglycemia in the sick patient..
Meanwhile, the other group includes patients with low blood glucose values, without an apparent pathology, that is, hypoglycemia may be the only disorder.
In these patients, the presence of an insulinoma (insulin-producing pancreatic tumor) should be suspected..
References
- Nares-Torices M, González-Martínez A, Martínez-Ayuso F, Morales-Fernández M. Hypoglycemia: time is brain. What are we doing wrong? Med Int Mex. 2018; 34 (6): 881-895. Available at: Scielo.org
- Malo-García F. What are the criteria for hypoglycemia? Update guide on diabetes. 2015. 79-80. Available at: redgdps.org
- Nicolau J, Giménez M and Miró O. Hypoglycemia. Urgent attention. No. 1,627. Available at: files.sld.cu
- Ottone C, Tallarico C, Chiarotti P, López I. Hypoglycemia. Roque Sáenz Peña Hospital Medical Clinic Service. Rosary beads. Santa Fe. Argentina. 2015.. Available at: clinic-unr.
- Pineda p. Endogenous hypoglycemia. Study and management. Med. Clin.



Yet No Comments